Abstract
Introduction
Nosocomial infections (NIs) are a major challenge worldwide. Identification of antibiotic resistance pattern extended spectrum beta-lactamases (ESBLs) and carbapenem-resistant Enterobacteriaceae (CRE) were the objectives of this study.
Methods
In this cross-sectional study, the antimicrobial susceptibility pattern of bacterial isolates collected from patients with NIs in ICU was determined. Overall, 42 Escherichia coli and Klebsiella pneumoniae isolates from different infection sites were used to determine phenotypic tests of ESBLs, Metallo-β-lactamases (MBLs) and CRE. Detection of ESBLs, MBLs and CRE genes were performed by the polymerase chain reaction (PCR) method.
Results
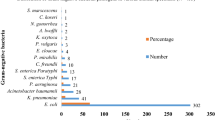
From 71 patients with NIs, 103 different bacterial strains were isolated. The most frequently isolated bacteria were E. coli (n = 29; 28.16%), Acinetobacter baumannii (n = 15; 14.56%), and K. pneumoniae (n = 13; 12.26%). Also, the rate of multidrug-resistant (MDR) isolates was 58.25% (60/103). Based on phenotypic confirmation tests, 32 (76.19%) isolates of E. coli and K. pneumoniae produced ESBLs, and 6 (14.28%) isolates were identified as CRE producers. PCR showed the high prevalence of the blaCTX-M (n = 29; 90.62%) in ESBL genes. In addition, blaNDM was detected in 4 (66.66%), blaOXA-23 in 3 (50%), and blaOXA-48 gene in 1 (16.66%) isolates. The blaVIM, blaKPC, and blaIMP genes were not detected in any of the isolates.
Conclusion
The Gram-negative bacteria E. coli, A. baumannii, and K. pneumoniae with high resistance levels were the most common bacteria causing NIs in the ICU. This study for the first time identified blaOXA-11, blaOXA-23, and blaNDM-1 genes in E. coli and K. pneumoniae in Ilam city of Iran.

Similar content being viewed by others
Data availability
The authors confirm that the data supporting the findings of this study are available within the article.
References
Mohammadi M, Vaisi Raiegan A, Jalali R, Ghobadi A, Salari N, Barati H (2019) The prevalence of nosocomial infections in Iranian hospitals. J Babol Univ Medical Sci 21:39–45
Hogeveen M, Heijting I, Jansen S, Hopman J, Overbeek MGD, Tostman A, Bekker V. (2021) Nosocomial infections in neonatal care: a scoping review protocol of published surveillance case definitions. https://osf.io/preprints/w9ce2/
Khammar M, Hassanzadeh S, Tara F, Siahsar M, Tahmasbi F, Keikha M, Ghazvini K (2021) A-4year Study on Antimicrobial Susceptibility Trends of Nosocomial Infections in a Mashhad Referral Hospital, Mashhad. Rev Clin Med, Iran, p 8
Nimer NA (2022) Nosocomial infection and antibiotic-resistant threat in the middle east. Infect Drug Resist. https://doi.org/10.2147/IDR.S351755
Rajabi M, Abdar ME, Rafiei H, Aflatoonia MR, Abdar ZE (2016) Nosocomial infections and epidemiology of antibiotic resistance in teaching hospitals in south east of Iran. Glob J Health Sci 8:190
Centers for disease control and prevention [CDC] Campaign to prevent antimicrobial resistance in healthcare settings: why a campaign? Atlanta GCfDCaP. (2001). https://www.cdc.gov/mmwr/preview/mmwrhtml/mm5115a5.htm
Agaba P, Tumukunde J, Tindimwebwa J, Kwizera A (2017) Nosocomial bacterial infections and their antimicrobial susceptibility patterns among patients in Ugandan intensive care units: a cross sectional study. BMC Res Notes 10:1–12
Leone M, Bouadma L, Bouhemad B, Brissaud O, Dauger S, Gibot S, Hraiech S, Jung B, Kipnis E, Launey Y (2018) Hospital-acquired pneumonia in ICU. Anaesth Crit Care Pain Med 37:83–98
Khan A, Miller WR, Arias CA (2018) Mechanisms of antimicrobial resistance among hospital-associated pathogens. Expert Rev Anti Infect Ther 16:269–287
Tolera M, Abate D, Dheresa M, Marami D (2018) Bacterial nosocomial infections and antimicrobial susceptibility pattern among patients admitted at Hiwot Fana Specialized University Hospital. Adv Med, Eastern Ethiopia. https://doi.org/10.1155/2018/2127814
Nwafia IN, Ohanu ME, Ebede SO, Ozumba UC (2019) Molecular detection and antibiotic resistance pattern of extended-spectrum beta-lactamase producing Escherichia coli in a Tertiary Hospital in Enugu. Nigeria Ann Clin Microbiol Antimicrob 18:1–7
Peralta G, Sanchez MB, Garrido JC, De Benito I, Cano ME, Martínez-Martínez L, Roiz MP (2007) Impact of antibiotic resistance and of adequate empirical antibiotic treatment in the prognosis of patients with Escherichia coli bacteraemia. J Antimicrob Chemother 60:855–863
Goltz J (2022) Investigating Factors Associated with Extended-Spectrum Beta-Lactamase-Producing Enterobacteriaceae Colonization and/or Infection in Humans: A One Health Approach: University of Guelph. https://atrium.lib.uoguelph.ca/xmlui/handle/10214/26906
Urase T, Okazaki M, Tsutsui H (2020) Prevalence of ESBL-producing Escherichia coli and carbapenem-resistant Enterobacteriaceae in treated wastewater: a comparison with nosocomial infection surveillance. J Water Health 18:899–910
Surgers L, Boyd A, Boelle P-Y, Lalande V, Jolivot P-A, Girard P-M, Arlet G, Cambier C, Homor A, Decre D (2017) Clinical and microbiological determinants of severe and fatal outcomes in patients infected with Enterobacteriaceae producing extended-spectrum β-lactamase. Eur J Clin Microbiol Infect Dis 36:1261–1268
Xiao T, Yang K, Zhou Y, Zhang S, Ji J, Ying C, Shen P, Xiao Y (2019) Risk factors and outcomes in non-transplant patients with extended-spectrum beta-lactamase-producing Escherichia coli bacteremia: a retrospective study from 2013 to 2016. Antimicrob Resist Infect Control 8:1–11
Maechler F, Schwab F, Hansen S, Fankhauser C, Harbarth S, Huttner BD, Diaz-Agero C, Lopez N, Canton R, Ruiz-Garbajosa P (2020) Contact isolation versus standard precautions to decrease acquisition of extended-spectrum β-lactamase-producing Enterobacterales in non-critical care wards: a cluster-randomised crossover trial. Lancet Infect Dis 20:575–584
Ding Y, Wang Y, Hsia Y, Sharland M, Heath PT (2019) Systematic review of carbapenem-resistant Enterobacteriaceae causing neonatal sepsis in China. Ann Clin Microbiol Antimicrob 18:1–8
Campion M, Scully G (2018) Antibiotic use in the intensive care unit: optimization and de-escalation. J Intensive Care Med 33:647–655
Garner J, Jarvis W, Emori T, Horan T, Hughes J (1991) CDC definitions for nosocomial infections 1988. Z Arztl Fortbild 85:818–827
Cheesbrough M (2005) District laboratory practice in tropical countries, part 2. Cambridge university press, Cambridge
Weinstein MP, Lewis JS (2020) The clinical and laboratory standards institute subcommittee on antimicrobial susceptibility testing: background, organization, functions, and processes. J Clin Microbiol 58:e01864-e11819
Yamagishi J, Sato Y, Shinozaki N, Ye B, Tsuboi A, Nagasaki M, Yamashita R (2016) Comparison of boiling and robotics automation method in DNA extraction for metagenomic sequencing of human oral microbes. PLoS ONE 11:e0154389
Golsha R, Ashoori N, Tajik M, Sohrabi A, Montazeri M (2020) Prevalence of nosocomial infections in intensive care units in shahid Sayyad-E-Shirazi Hospital of Gorgan During 2016-2018. Tabari Biomed Stu Res J. https://doi.org/10.18502/tbsrj.v2i2.3761
Birgani AG, Asadpoor S (2008-2009) Nosocomial infections in intensive care unit of Ahvaz Arya Hospital. Modern Care Journal. 2011;8(2): 58–93.
Tabatabaei SM, Pour FB, Osmani S. (2015) Epidemiology of hospital-acquired infections and related anti-microbial resistance patterns in a tertiary-care teaching hospital in Zahedan, Southeast Iran. Int J Infect. 2(4). e29079 https://doi.org/10.17795/iji-29079.
Zare-Bidaki M, Allahyari E, Nikoomanesh F, Ebrahimzadeh A (2021) A comparative analysis of nosocomial infections between internal and surgical intensive care units of university hospitals in Birjand, Iran from 2016 to 2017: a retrospective study. J Basic Res Med Sci 8:32–41
Boora S, Singh P, Verma A, Chauhan A, Lathwal A, Mathur P (2021) Point-prevalence survey for the hospital-acquired infections in intensive care units of trauma center in a tertiary care hospital of Northern India. J Lab Physicians 14(2):115–118
Wang J, Liu F, Tartari E, Huang J, Harbarth S, Pittet D, Zingg W (2018) The prevalence of healthcare-associated infections in mainland China: a systematic review and meta-analysis. Infect Control Hosp Epidemiol 39:701–709
Mitharwal SM, Yaddanapudi S, Bhardwaj N, Gautam V, Biswal M, Yaddanapudi L (2016) Intensive care unit-acquired infections in a tertiary care hospital: an epidemiologic survey and influence on patient outcomes. Am J Infect Control 44:e113–e117
Ott E, Saathoff S, Graf K, Schwab F, Chaberny IF (2013) The prevalence of nosocomial and community acquired infections in a university hospital: an observational study. Dtsch Arztebl Int 110:533
Nouri F, Karami P, Zarei O, Kosari F, Alikhani MY, Zandkarimi E, Zarandi ER, Taheri M (2020) Prevalence of common nosocomial infections and evaluation of antibiotic resistance patterns in patients with secondary infections in Hamadan. Iran Infect Drug Resist 13:2365
Rahimi-Bashar F, Karami P, Khaledi A, Dehghan A, Seifrabie MA, Yaghoobi MH (2018) Evaluation of the prevalence of nosocomial infection in different wards of Be’sat hospital of Hamedan. Avicenna J Clin Microbiol Infect 5:31–35
Shoaei S, Sali S, Yousefi H (2017) Incidence and resistance patterns of nosocomial infections in labbafi nejad hospital admitted patients during 2012–2014. Int J Infect Dis 3:78–81
Fortuin-de Smidt MC, Singh-Moodley A, Badat R, Quan V, Kularatne R, Nana T, Lekalakala R, Govender NP, Perovic O (2015) Staphylococcus aureus bacteraemia in Gauteng academic hospitals. South Africa Int J Infect Dis 30:41–48
Pournajafi A, Mahmoudi A (2020) Prevalence of extended-spectrum beta-lactamases production in Escherichia coli isolated from urinary tract infection samples in Zanjan hospitals. South Asian Res J Pharm Sci, Iran
Hasani A, Mohammadzadeh A, Kafil HS, Rezaee MA, Hasani A, Aghazadeh M (2015) Characterization of TEM-, SHV-, CTX-and AmpC-type β-lactamases from cephalosporin resistant Escherichia coli isolates from Northwest of Iran. J Pure Appl Microbiol 9:3401–3406
Bialvaei AZ, Kafil HS, Asgharzadeh M, Aghazadeh M, Yousefi M (2016) CTX-M extended-spectrum β-lactamase-producing Klebsiella spp, Salmonella spp, Shigella spp and Escherichia coli isolates in Iranian hospitals. Braz J Microbiol 47:706–711
Jabalameli L, Beigverdi R, Ranjbar HH, Pouriran R, Jabalameli F, Emaneini M (2021) Phenotypic and genotypic prevalence of extended-spectrum β-Lactamase-Producing Escherichia coli: a systematic review and meta-analysis in Iran. Microb Drug Resist 27:73–86
Saisi H, Makobe C, Kangongo M, Kariuki S (2019) Prevalence of CTXM, SHV, TEM AND OXA genes among extended-spectrum beta-lactamase producing Klebsiella pneumoniae from Mukuru Slum. Kenya Adv Microbiol 9:853–862
Zadeh SB, Shakib P, Zolfaghari MR, Sheikh AF (2021) Prevalence of Escherichia coli and Klebsiella pneumoniae, Producing Extended-Spectrum Beta-Lactamase (ESBLs) from Clinical Specimen in Khuzestan. Gene, Cell and Tissue, Iran, p 8
Shahbazi S, Karam MRA, Habibi M, Talebi A, Bouzari S (2018) Distribution of extended-spectrum β-lactam, quinolone and carbapenem resistance genes, and genetic diversity among uropathogenic Escherichia coli isolates in Tehran. Iran J Globa Antimicrob Resist 14:118–125
Nasiri MJ, Mirsaeidi M, Mousavi SMJ, Arshadi M, Fardsanei F, Deihim B, Davoudabadi S, Zamani S, Hajikhani B, Goudarzi H (2020) Prevalence and mechanisms of carbapenem resistance in Klebsiella pneumoniae and Escherichia coli: a systematic review and meta-analysis of cross-sectional studies from Iran. Microb Drug Resist 26:1491–1502
Shahcheraghi F, Nobari S, Rahmati Ghezelgeh F, Nasiri S, Owlia P, Nikbin VS, Imani Fooladi AA (2013) First report of New Delhi metallo-beta-lactamase-1-producing Klebsiella pneumoniae in Iran. Microb Drug Resist 19:30–36
Fazeli H, Norouzi-Barough M, Ahadi A, Shokri D, Solgi H (2015) Detection of New Delhi Metallo-Beta-Lactamase-1 (NDM-1) in carbapenem-resistant Klebsiella pneumoniae isolated from a university hospital in Iran. Hippokratia 19:205
Moghadampour M, Rezaei A, Faghri J (2018) The emergence of bla OXA-48 and bla NDM among ESBL-producing Klebsiella pneumoniae in clinical isolates of a tertiary hospital in Iran. Acta Microbiol Immunol Hung 65:335–344
Huang X, Cheng X, Sun P, Tang C, Ni F, Liu G (2018) Characteristics of NDM-1-producing Klebsiella pneumoniae ST234 and ST1412 isolates spread in a neonatal unit. BMC Microbiol 18:1–6
Kiaei S, Moradi M, Hosseini-Nave H, Ziasistani M, Kalantar-Neyestanaki D (2019) Endemic dissemination of different sequence types of carbapenem-resistant Klebsiella pneumoniae strains harboring blaNDM and 16S rRNA methylase genes in Kerman hospitals, Iran, from 2015 to 2017. Infect Drug Resist 12:45
Jalalvand K, Shayanfar N, Shahcheraghi F, Amini E, Mohammadpour M, Babaheidarian P (2020) Evaluation of phenotypic and genotypic characteristics of carbapnemases-producing enterobacteriaceae and its prevalence in a referral hospital in Tehran city. Iran J Pathol 15:86
Eyvazi S, Hakemi-Vala M, Hashemi A, Bejestani FB, Elahi N. (2018) Emergence of NDM-1-producing Escherichia coli in Iran. Arch Clin Infect Dis 13(4):e62029
Gao B, Li X, Yang F, Chen W, Zhao Y, Bai G, Zhang Z (2019) Molecular epidemiology and risk factors of ventilator-associated pneumonia infection caused by carbapenem-resistant enterobacteriaceae. Front Pharmacol 10:262
Acknowledgements
We would like to thank the Clinical Microbiology Research Center, Ilam University of Medical Sciences, Ilam, Iran, for their cooperation. The authors also acknowledge the Vice Chancellor for Research Affairs, Ilam University of Medical Sciences, for their executive and financial support.
Author information
Authors and Affiliations
Contributions
NS and HK contributed to the study conception and design. Data collection and analysis were performed by MH and SK. The first draft of the manuscript was written by MH and SK, and all the authors commented on the previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors report no conflict of interest in this study.
Ethical approval
The study protocol was approved by the local ethics committee of Ilam University of Medical Sciences Iran (ethical code: IR.MADILAM.REC.1400.003). Written informed consent was received from each patient.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hashemian, M., Kazemian, H., Kaviar, V.H. et al. Nosocomial infections and antimicrobial susceptibility patterns among patients admitted to intensive care unit of Imam Khomeini hospital in Ilam, Iran. Mol Biol Rep 50, 5565–5574 (2023). https://doi.org/10.1007/s11033-023-08476-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11033-023-08476-4