Abstract
Background
Overexpression of lysophosphatidylcholine acyltransferase 1 (LPCAT1) has been found in various solid cancers and is associated with disease progression, metastasis, and recurrence. However, the expression pattern of LPCAT1 in acute myeloid leukemia (AML) bone marrow remains unknown. The present study aimed to compare LPCAT1 expression differences in bone marrow samples from AML patients and healthy controls and assess the clinical relevance of LPCAT1 in AML.
Methods and results
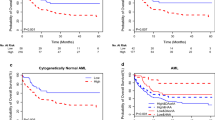
LPCAT1 expression in bone marrow was significantly lower in AML than in healthy controls predicted by public databases. Furthermore, real-time quantitative PCR (RQ-PCR) validated that LPCAT1 expression in bone marrow was significantly down-regulated in AML compared to healthy controls [0.056 (0.000–0.846) vs 0.253 (0.031–1.000)]. The DiseaseMeth version 2.0 and The Cancer Genome Atlas analysis revealed that the LPCAT1 promoter was hypermethylated in AML, and there was a strong negative correlation between LPCAT1 expression and methylation (R = − 0.610, P < 0.001). RQ-PCR revealed that the frequency of LPCAT1 low expression was lower in the FAB-M4/M5 subtype than in the other subtypes (P = 0.018). The ROC curve revealed that LPCAT1 expression could serve as a potential diagnostic marker for differentiating AML from controls with an area under the ROC curve of 0.819 (95% CI 0.743–0.894, P < 0.001). In cytogenetically normal AML, patients with LPCAT1 low expression had significantly longer overall survival than those without LPCAT1 low expression (median 19 versus 5.5 months, P = 0.036).
Conclusions
LPCAT1 is down-regulated in AML bone marrow, and LPCAT1 down-regulation could be used as a potential biomarker for AML diagnosis and prognosis.





Similar content being viewed by others
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
Estey E, Döhner H (2006) Acute myeloid leukaemia. Lancet 368:1894–1907
Ferrara F (2004) Unanswered questions in acute myeloid leukaemia. Lancet Oncol 5:443–450
Avivi I, Rowe JM (2005) Prognostic factors in acute myeloid leukemia. Curr Opin Hematol 12:62–67
Grimwade D (2001) The clinical significance of cytogenetic abnormalities in acute myeloid leukaemia. Best Pract Res Clin Haematol 14:497–529
Byrd JC, Mrózek K, Dodge RK et al (2002) Pretreatment cytogenetic abnormalities are predictive of induction success, cumulative incidence of relapse, and overall survival in adult patients with de novo acute myeloid leukemia: results from Cancer and Leukemia Group B (CALGB 8461). Blood 100:4325–4336
Mrózek K, Marcucci G, Paschka P et al (2007) Clinical relevance of mutations and gene-expression changes in adult acute myeloid leukemia with normal cytogenetics: are we ready for a prognostically prioritized molecular classification? Blood 109:431–448
Mrózek K, Döhner H, Bloomfield CD (2007) Influence of new molecular prognostic markers in patients with karyotypically normal acute myeloid leukemia: recent advances. Curr Opin Hematol 14:106–114
Santos CR, Schulze A (2012) Lipid metabolism in cancer. FEBS J 279:2610–2623
Kent C (2005) Regulatory enzymes of phosphatidylcholine biosynthesis: a personal perspective. Biochim Biophys Acta 1733:53–66
Shindou H, Shimizu T (2009) Acyl-CoA: lysophospholipid acyltransferases. J Biol Chem 284:1–5
Grupp K, Sanader S, Sirma H et al (2013) High lysophosphatidylcholine acyltransferase 1 expression independently predicts high risk for biochemical recurrence in prostate cancers. Mol Oncol 7:1001–1011
He RQ, Li JD, Du XF et al (2021) LPCAT1 overexpression promotes the progression of hepatocellular carcinoma. Cancer Cell Int 21(1):442
Sun Q, Liu X, Peng Q et al (2022) ncRNA-mediated high expression of LPCAT1 correlates with poor prognosis and tumor immune infiltration of liver hepatocellular carcinoma. J Immunol Res 2022:1584397
Ji W, Peng Z, Sun B et al (2021) LPCAT1 promotes malignant transformation of hepatocellular carcinoma cells by directly suppressing STAT1. Front Oncol 11:678714
Morita Y, Sakaguchi T, Ikegami K et al (2013) Lysophosphatidylcholine acyltransferase 1 altered phospholipid composition and regulated hepatoma progression. J Hepatol 59:292–299
Shen L, Gu P, Qiu C et al (2022) Lysophosphatidylcholine acyltransferase 1 promotes epithelial-mesenchymal transition of hepatocellular carcinoma via the Wnt/β-catenin signaling pathway. Ann Hepatol 27(3):100680
Lebok P, von Hassel A, Meiners J et al (2019) Up-regulation of lysophosphatidylcholine acyltransferase 1 (LPCAT1) is linked to poor prognosis in breast cancer. Aging (Albany NY) 11:7796–7804
Abdelzaher E, Mostafa MF (2015) Lysophosphatidylcholine acyltransferase 1 (LPCAT1) upregulation in breast carcinoma contributes to tumor progression and predicts early tumor recurrence. Tumour Biol 36:5473–5483
Zhao T, Zhang Y, Ma X et al (2021) Elevated expression of LPCAT1 predicts a poor prognosis and is correlated with the tumour microenvironment in endometrial cancer. Cancer Cell Int 21(1):269
Shida-Sakazume T, Endo-Sakamoto Y, Unozawa M et al (2015) Lysophosphatidylcholine acyltransferase1 overexpression promotes oral squamous cell carcinoma progression via enhanced biosynthesis of platelet-activating factor. PLoS ONE 10:e0120143
Tao M, Luo J, Gu T et al (2021) LPCAT1 reprogramming cholesterol metabolism promotes the progression of esophageal squamous cell carcinoma. Cell Death Dis 12(9):845
Huang Y, Wang Y, Wang Y et al (2022) LPCAT1 promotes cutaneous squamous cell carcinoma via EGFR-mediated protein kinase B/p38MAPK signaling pathways. J Invest Dermatol 142(2):303-313.e9
Wei C, Dong X, Lu H et al (2019) LPCAT1 promotes brain metastasis of lung adenocarcinoma by up-regulating PI3K/AKT/MYC pathway. J Exp Clin Cancer Res 38:95
Ding J, Ding X, Leng Z (2022) LPCAT1 promotes gefitinib resistance via upregulation of the EGFR/PI3K/AKT signaling pathway in lung adenocarcinoma. J Cancer 13(6):1837–1847
Yin C, Zhang J, Guan W et al (2021) High expression of CLEC11A predicts favorable prognosis in acute myeloid leukemia. Front Oncol 11:608932
Bagger FO, Sasivarevic D, Sohi SH et al (2016) BloodSpot: a database of gene expression profiles and transcriptional programs for healthy and malignant haematopoiesis. Nucleic Acids Res 44:D917–D924
Bennett JM, Catovsky D, Daniel MT et al (1985) Proposed revised criteria for the classification of acute myeloid leukemia. A report of the French-American-British Cooperative Group. Ann Intern Med 103:620–625
Vardiman JW, Harris NL, Brunning RD (2002) The World Health Organization (WHO) classification of the myeloid neoplasms. Blood 100:2292–2302
Lo Coco F, Foa R (1995) Diagnostic and prognostic advances in the immunophenotypic and genetic characterization of acute leukaemia. Eur J Haematol 55:1–9
Slovak ML, Kopecky KJ, Cassileth PA et al (2000) Karyotypic analysis predicts outcome of preremission and postremission therapy in adult acute myeloid leukemia: a Southwest Oncology Group/Eastern Cooperative Oncology Group Study. Blood 96:4075–4083
Lin J, Yao DM, Qian J et al (2012) IDH1 and IDH2 mutation analysis in Chinese patients with acute myeloid leukemia and myelodysplastic syndrome. Ann Hematol 91:519–525
Lin J, Yao DM, Qian J et al (2011) Recurrent DNMT3A R882 mutations in Chinese patients with acute myeloid leukemia and myelodysplastic syndrome. PLoS ONE 6:e26906
Yang X, Qian J, Sun A et al (2013) RAS mutation analysis in a large cohort of Chinese patients with acute myeloid leukemia. Clin Biochem 46:579–583
Qian J, Yao DM, Lin J et al (2012) U2AF1 mutations in Chinese patients with acute myeloid leukemia and myelodysplastic syndrome. PLoS ONE 7:e45760
Wen XM, Lin J, Yang J et al (2014) Double CEBPA mutations are prognostically favorable in non-M3 acute myeloid leukemia patients with wild-type NPM1 and FLT3-ITD. Int J Clin Exp Pathol 7:6832–6840
Wang K, Wu Z, Si Y et al (2021) Identification of LPCAT1 expression as a potential prognostic biomarker guiding treatment choice in acute myeloid leukemia. Oncol Lett 21:105
Abdelzaher Ahmed E, Abdel Bary Abdel-Latif A, Fahmy AM et al (2021) Differential lysophosphatidylcholine acyltransferase 1 (LPCAT1) expression confers aggressiveness and independently predicts recurrence in bladder urothelial carcinomas. J Histotechnol 44(4):196–205
Pabst T, Kortz L, Fiedler GM et al (2017) The plasma lipidome in acute myeloid leukemia at diagnosis in relation to clinical disease features. BBA Clin 7:105–114
Gottfried EL (1967) Lipids of human leukocytes: relation to celltype. J Lipid Res 8(4):321–327
Zhou JD, Zhang TJ, Xu ZJ et al (2020) Genome-wide methylation sequencing identifies progression-related epigenetic drivers in myelodysplastic syndromes. Cell Death Dis 11:997
Taby R, Issa JP (2010) Cancer epigenetics. CA Cancer J Clin 60:376–392
Yamashita K, Hosoda K, Nishizawa N et al (2018) Epigenetic biomarkers of promoter DNA methylation in the new era of cancer treatment. Cancer Sci 109:3695–3706
Funding
This study was supported by National Natural Science foundation of China (81970118), the Youth Medical Talents Project of “Ke Jiao Qiang Wei” project of Jiangsu province (QNRC2016449), and Zhenjiang Clinical Research Center of Hematology (SS2018009).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study’s conception and design. Material preparation, data collection and analysis were performed by Qin Chen, Zijun Xu, and Jiang Lin. The first draft of the manuscript was written by Qin Chen and Zhaoqun Deng. The manuscript revision was conducted by Jun Qian and Wei Qian. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
This study was conducted in compliance with the 1964 Helsinki declaration and was approved by the Ethics Committee of the Affiliated People’s Hospital of Jiangsu University (No. K-20180063-Y).
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chen, Q., Xu, Z., Lin, J. et al. The validation and clinical significance of LPCAT1 down-regulation in acute myeloid leukemia. Mol Biol Rep 50, 4955–4963 (2023). https://doi.org/10.1007/s11033-023-08449-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11033-023-08449-7