Abstract
Background
Preoperative chemoradiotherapy has long been accepted as a method to improve survival and lifetime quality of rectal cancer patients. However, physiologic effects of these therapies largely depend on the resistance of cells to the radiation, type of chemotherapeutic agents and individual responses. As one of the signaling cascades involved in chemo- or radiation- resistance, the present study focused on several proteins involved in pTEN/Akt/mTOR pathway to explore their prognostic significance.
Materials and methods
Samples from advanced stage rectal cancer patients were analyzed to detect expression levels of pTEN/Akt/mTOR pathway related proteins pTEN, mLST8, REDD1, BNIP3, SAG and NOXA, together with p53, by RT-qPCR. Kaplan–Meier analysis was used to assess expression-survival relation and correlations among all proteins and clinicopathological features were statistically analyzed.
Results.
Except p53, none of the proteins showed prognostic significance. High p53 expression presented clear impact on overall survival and disease free survival. It was also significantly related to pathologic complete response. p53 showed high correlation to local recurrence as well. On the other hand, strong correlation was observed with PTEN expression and tumor response, but not with survival. High associations were also observed between mLST8/REDD1, PTEN and NOXA, confirming their role in the same cascade.
Conclusion
The contentious role of p53 as a prognostic biomarker in colorectal cancer was further affirmed, while PTEN and REDD1 could be suggested as potential candidates. Additionally, NOXA emerges as a conjunctive element for different signaling pathways.


Similar content being viewed by others
References
Kulendran M, Stebbing JF, Marks CG, Rockall TA (2011) Predictive and prognostic factors in colorectal cancer: a personalized approach. Cancers 3:1622–1638. https://doi.org/10.3390/cancers3021622
Dayde D, Tanaka I, Jain R, Tai MC, Taguchi A (2017) Predictive and prognostic molecular biomarkers for response to neoadjuvant chemoradiation in rectal cancer. Int J Mol Sci 18:573. https://doi.org/10.3390/ijms18030573
Sartore-Bianchi A, Di Nicolantonio F, Nichelatti M, Molinari F, De Dosso S, Saletti P et al (2009) Multi-determinants analysis of molecular alterations for predicting clinical benefit to EGFR-targeted monoclonal antibodies in colorectal cancer. PLoS ONE 4:e7287. https://doi.org/10.1371/journal.pone.0007287
Sun Y, Tian H, Wang L (2015) Effects of PTEN on the proliferation and apoptosis of colorectal cancer cells via the phosphoinositol-3-kinase/Akt pathway. Oncol Rep 33:1828–1836. https://doi.org/10.3892/or.2015.3804
Sarbassov DD, Guertin DA, Ali SM, Sabatini DM (2005) Phosphorylation and regulation of Akt/PKB by the Rictor-mTOR complex. Science 307:1098–1101. https://doi.org/10.1126/science.1106148
Chan CH, Jo U, Kohrman A, Rezaeian AH, Chou PC, Logothetis C, Lin HK (2014) Posttranslational regulation of Akt in human cancer. Cell Biosci 4(1):59. https://doi.org/10.1186/2045-3701-4-59
Manning BD, Toker A (2017) AKT/PKB signaling: navigating the network. Cell 169:381–405. https://doi.org/10.1016/j.cell.2017.04.001
Ozden SA, Ozyurt H, Ozgen Z, Kilinc O, Oncel M, Gul AE, Karadayi N, Serakinci N, Kan B, Orun O (2011) Prognostic role of sensitive-to-apoptosis gene expression in rectal cancer. World J Gastroenterol 17:4905–4910. https://doi.org/10.3748/wjg.v17.i44.4905
Mega Tiber P, Baloglu L, Ozden S, Ozgen Z, Ozyurt H, Eren M, Orun O (2014) The association of apoptotic protein expressions sensitive to apoptosis gene, p73 and p53 with the prognosis of cervical carcinoma. Onco Targets Ther 7:2161–2168. https://doi.org/10.2147/OTT.S71448
Jia L, Yang J, Hao X, Zheng M, He H, Xiong X, Xu L, Sun Y (2010) Validation of SAG/RBX2/ROC2 E3 ubiquitin ligase as an anticancer and radiosensitizing target. Clin Cancer Res 20116:814–824. https://doi.org/10.1158/1078-0432.CCR-09-1592
Wei D, Sun Y (2010) Small ring finger proteins RBX1 and RBX2 of SCF E3 ubiquitin ligases: the role in cancer and as cancer targets. Genes Cancer 1:700–707. https://doi.org/10.1177/1947601910382776
Zhao Y, Xiong X, Sun Y (2011) DEPTOR, an mTOR inhibitor, is a physiological substrate of SCF (βTrCP) E3 ubiquitin ligase and regulates survival and autophagy. Mol Cell 44:304–316. https://doi.org/10.1016/j.molcel.2011.08.029
Gao D, Inuzuka H, Tan MK, Fukushima H, Locasale JW, Liu P et al (2011) mTOR drives its own activation via SCF(βTrCP)-dependent degradation of the mTOR inhibitor DEPTOR. Mol Cell 44:290–303. https://doi.org/10.1016/j.molcel.2011.08.030
Løes IM, Immervoll H, Sorbye H, Angelsen JH, Horn A, Knappskog S, Lønning PE (2016) Impact of KRAS, BRAF, PIK3CA, TP53 status and intraindividual mutation heterogeneity on outcome after liver resection for colorectal cancer metastases. Int J Cancer 139:647–656. https://doi.org/10.1002/ijc.30089
Tsilimigras DI, Ntanasis-Stathopoulos I, Bagante F, Moris D, Cloyd J, Spartalis E, Pawlik TM (2018) Clinical significance and prognostic relevance of KRAS, BRAF, PI3K and TP53 genetic mutation analysis for resectable and unresectable colorectal liver metastases: a systematic review of the current evidence. Surg Oncol 27:280–288. https://doi.org/10.1016/j.suronc.2018.05.012
Chen MB, Wu XY, Yu R, Li C, Wang LQ, Shen W, Lu PH (2012) P53 status as a predictive biomarker for patients receiving neoadjuvant radiation-based treatment: a meta-analysis in rectal cancer. PLoS ONE 7:e45388. https://doi.org/10.1371/journal.pone.0045388
Huh JW, Lee WY, Kim SH, Park YA, Cho YB, Yun SH et al (2015) Immunohistochemical detection of p53 expression in patients with preoperative chemoradiation for rectal cancer: association with prognosis. Yonsei Med J 56:82–88. https://doi.org/10.3349/ymj.2015.56.1.82
Lu Y, Gao J, Lu Y (2015) Down-expression pattern of Ku70 and p53 coexisted in colorectal cancer. Med Oncol 32:98. https://doi.org/10.1007/s12032-015-0519-9
Song MS, Salmena L, Pandolfi PP (2012) The functions and regulation of the PTEN tumour suppressor. Nat Rev Mol Cell Biol 13:283–296. https://doi.org/10.1038/nrm3330
Leslie NR, Downes CP (2004) PTEN function: how normal cells control it and tumour cells lose it. Biochem J 382:1–11. https://doi.org/10.1042/BJ20040825
Chalhoub N, Baker SJ (2009) PTEN and the PI3-kinase pathway in cancer. Annu Rev Pathol 4:127–150. https://doi.org/10.1146/annurev.pathol.4.110807.092311
Chow LM, Baker SJ (2006) PTEN function in normal and neoplastic growth. Cancer Lett 241:184–196. https://doi.org/10.1016/j.canlet.2005.11.042
Sawai H, Yasuda A, Ochi N, Ma J, Matsuo Y, Wakasugi T et al (2008) Loss of PTEN expression is associated with colorectal cancer liver metastasis and poor patient survival. BMC Gastroenterol 8:56. https://doi.org/10.1186/1471-230X-8-56
Eklöf V, Wikberg ML, Edin S, Dahlin AM, Jonsson BA, Öberg Å, Rutegård J, Palmqvist R (2013) The prognostic role of KRAS, BRAF, PIK3CA and PTEN in colorectal cancer. Br J Cancer 108:2153–2163. https://doi.org/10.1038/bjc.2013.212
Stambolic V, MacPherson D, Sas D, Lin Y, Snow B, Jang Y, Benchimol S, Mak TW (2001) Regulation of PTEN transcription by p53. Mol Cell 8:317–325. https://doi.org/10.1016/S1097-2765(01)00323-9
Hettinger K, Vikhanskaya F, Poh MK, Lee MK, de Belle I, Zhang JT, Reddy SA, Sabapathy K (2007) c-Jun promotes cellular survival by suppression of PTEN. Cell Death Differ 14:218–229. https://doi.org/10.1038/sj.cdd.4401946
Bermúdez Brito M, Goulielmaki E, Papakonstanti EA (2015) Focus on PTEN regulation. Front Oncol 5:166. https://doi.org/10.3389/fonc.2015.00166
Bohn BA, Mina S, Krohn A, Simon R, Kluth M, Harasimowicz S et al (2013) Altered PTEN function caused by deletion or gene disruption is associated with poor prognosis in rectal but not in colon cancer. Hum Pathol 4:1524–1533. https://doi.org/10.1016/j.humpath.2012.12.006
Wang X, Cao X, Sun R, Tang C, Tzankov A, Zhang J et al (2018) Clinical significance of PTEN deletion, mutation, and loss of PTEN expression in de novo diffuse large B-cell lymphoma. Neoplasia 20:574–593. https://doi.org/10.1016/j.neo.2018.03.002
Li S, Shen Y, Wang M, Yang J, Lv M, Li P, Chen Z, Yang J (2017) Loss of PTEN expression in breast cancer: association with clinicopathological characteristics and prognosis. Oncotarget 8:32043–32054. https://doi.org/10.18632/oncotarget.16761
Zhao J, Chen F, Zhou Q, Pan W, Wang X, Xu J, Ni L, Yang H (2016) Aberrant expression of microRNA-99a and its target gene mTOR associated with malignant progression and poor prognosis in patients with osteosarcoma. Onco Targets Ther 9:1589–1597. https://doi.org/10.2147/OTT.S102421
Khanna A, Bhushan B, Chauhan PS, Saxena S, Gupta DK, Siraj F (2018) High mTOR expression independently prognosticates poor clinical outcome to induction chemotherapy in acute lymphoblastic leukemia. Clin Exp Med 18:221–227. https://doi.org/10.1007/s10238-017-0478-x
Kaibori M, Shikata N, Sakaguchi T, Ishizaki M, Matsui K, Iida H et al (2015) Influence of rictor and raptor expression of mTOR signaling on long-term outcomes of patients with hepatocellular carcinoma. Dig Dis Sci 60:919–928. https://doi.org/10.1007/s10620-014-3417-7
Karlsson E, Pérez-Tenorio G, Amin R, Bostner J, Skoog L, Fornander T, Sgroi DC, Nordenskjöld B, Hallbeck AL, Stål O (2013) The mTOR effectors 4EBP1 and S6K2 are frequently coexpressed, and associated with a poor prognosis and endocrine resistance in breast cancer: a retrospective study including patients from the randomised Stockholm tamoxifen trials. Breast Cancer Res 15:R96. https://doi.org/10.1186/bcr3557
Kakumoto K, Ikeda J, Okada M, Morii E, Oneyama C (2015) mLST8 promotes mTOR-mediated tumor progression. PLoS ONE 10:e0119015. https://doi.org/10.1371/journal.pone.0119015
Ellisen LW, Ramsayer KD, Johannessen CM, Yang A, Beppu H, Minda K, Oliner JD, McKeon F, Haber DA (2002) REDD1, a developmentally regulated transcriptional target of p63 and p53, links p63 to regulation of reactive oxygen species. Mol Cell 10:995–1005. https://doi.org/10.1016/s1097-2765(02)00706-2
Shoshani T, Faerman A, Mett I, Zelin E, Tenne T, Gorodin S et al (2002) Identification of a novel hypoxia-inducible factor 1-responsive gene, RTP801, involved in apoptosis. Mol Cell Biol 22:2283–2293. https://doi.org/10.1128/MCB.22.7.2283-2293.2002
Katiyar S, Liu E, Knutzen CA, Lang ES, Lombardo CR, Sankar S, Toth JI, Petroski MD, Ronai Z, Chiang GG (2009) REDD1, an inhibitor of mTOR signalling, is regulated by the CUL4A-DDB1 ubiquitin ligase. EMBO Rep 10:866–872. https://doi.org/10.1038/embor.2009.93
Li Y, Wang Y, Kim E, Beemiller P, Wang CY, Swanson J, You M, Guan KL (2007) Bnip3 mediates the hypoxia-induced inhibition on mammalian target of rapamycin by interacting with Rheb. J Biol Chem 282:35803–35813. https://doi.org/10.1074/jbc.M705231200
Okami J, Simeone DM, Logsdon CD (2004) Silencing of the hypoxia-inducible cell death protein BNIP3 in pancreatic cancer. Cancer Res 64:5338–5346. https://doi.org/10.1158/0008-5472.CAN-04-0089
Murai M, Toyota M, Suzuki H, Satoh A, Sasaki Y, Akino K (2005) Aberrant methylation and silencing of the BNIP3 gene in colorectal and gastric cancer. Clin Cancer Res 11:1021–1027
Jia W, Chang B, Sun L, Zhu H, Pang L, Tao L et al (2014) REDD1 and p-AKT over-expression may predict poor prognosis in ovarian cancer. Int J Clin Exp Pathol 7:5940–5949
Feng Y, Song K, Shang W, Chen L, Wang C, Pang B, Wang N (2020) REDD1 overexpression in oral squamous cell carcinoma may predict poor prognosis and correlates with high microvessel density. Oncol Lett 19:431–441. https://doi.org/10.3892/ol.2019.11070
Chang B, Meng J, Zhu H, Du X, Sun L, Wang L, Li S, Yang G (2018) Overexpression of the recently identified oncogene REDD1 correlates with tumor progression and is an independent unfavorable prognostic factor for ovarian carcinoma. Diagn Pathol 13:87. https://doi.org/10.1186/s13000-018-0754-4
Koop EA, van Laar T, van Wichen DF, de Weger RA, Ev W, van Diest PJ (2009) Expression of BNIP3 in invasive breast cancer: correlations with the hypoxic response and clinicopathological features. BMC Cancer 9:175. https://doi.org/10.1186/1471-2407-9-175
Sun Y, Tan M, Duan H, Swaroop M (2001) SAG/ROC/Rbx/Hrt, a zinc RING finger gene family: molecular cloning, biochemical properties, and biological functions. Antioxid Redox Signal 3:635–650. https://doi.org/10.1089/15230860152542989
Chanalaris A, Sun Y, Latchman DS, Stephanou A (2003) SAG attenuates apoptotic cell death caused by simulated ischaemia/reoxygenation in rat cardiomyocytes. J Mol Cell Cardiol 35:257–264. https://doi.org/10.1016/s0022-2828(03)00003-8
Jia L, Sun Y (2011) SCF E3 ubiquitin ligases as anticancer targets. Curr Cancer Drug Targets 11:347–356. https://doi.org/10.2174/156800911794519734
Oda E, Ohki R, Murasawa H, Nemoto J, Shibue T, Yamashita T, Tokino T, Taniguchi T, Tanaka N (2000) Noxa, a BH3-only member of the Bcl-2 family and candidate mediator of p53-induced apoptosis. Science 288:1053–1058. https://doi.org/10.1126/science.288.5468.1053
Flinterman M, Guelen L, Ezzati-Nik S, Killick R, Melino G, Tominaga K, Mymryk JS, Gäken J, Tavassoli M (2005) E1A activates transcription of p73 and Noxa to induce apoptosis. J Biol Chem 280:5945–5959. https://doi.org/10.1074/jbc.M406661200
Acknowledgements
We thank Dr. Esra AKDENIZ for her valuable contribution on biostatistical evaluations.
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. SÖ, ZÖ and HÖ: material preparation and all clinical applications; PY, OK and PMT: all experimental, data collection and analyses; OO: conception, management of the project, preparation of the first draft of the manuscript all authors commented on previous versions of the manuscript, read and approved the final form.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of Marmara University School of Medicine Ethics Board; with Protocol Number: 09.2015.275; Date: 02.10.2015.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent to publish
This manuscript does not contain any individual person’s data in any form.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
11033_2022_7665_MOESM1_ESM.tif
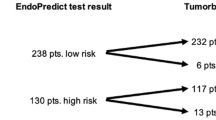
Supplementary file1 (TIF 803 KB) Supplementary Figure S1 Representative network of PTEN/mTOR axis proteins involved in this study: (a) mTOR is an element in growth factor induction, but also regulated by nutrient depletion, hypoxia and energy stresses. mTORC1 activity relies on GTP-loaded Rheb and this interaction could be inhibited during hypoxia by BNIP3 (b) Hypoxia also inhibits mTORC1 through REDD1/DDIT4 dependent TSC1/TSC2 complex activity as a GTPase (GAP) for Rheb (c) p53 downregulates mTOR pathway through induction of PTEN, TSC2 and REDD1. Akt-Mdm2-p53 forms a negative-loop for p53 regulation, while PTEN-Akt-Mdm2-p53 forms a positive feedback. (d) mLST8 is a scaffolding element for both complexes. It reduces mTORC2 mediated phosphorylation of Akt and inhibits 4E-BP1 phosphorylation in cancer cells. (e) SAG is a component of SCF E3 Ubq ligase, actively involved in DEPTOR degradation, as well as it shows anti-apoptotic effect through NOXA degradation. SAG expression is also induced by hypoxia through HIF-1. Kaplan-Meier analysis of p53 and 10-year overall survival, together with Spearman correlations represented in Figure 1 and Table 3 were also summarized at the right column
Rights and permissions
About this article
Cite this article
Orun, O., Özden, S., Kılınç, O. et al. The role of the PTEN/mTOR axis in clinical response of rectal cancer patients. Mol Biol Rep 49, 8461–8472 (2022). https://doi.org/10.1007/s11033-022-07665-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11033-022-07665-x