Abstract
Background
Shikonin is a natural multipotent anti-tumorigenic compound. We investigated potential synergy between shikonin and anti-diabetic metformin against tumorigenic properties of breast cancer cell line MCF-7.
Methods and results
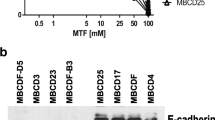
The IC50 of shikonin and metformin was determined after a single treatment of two cell lines MCF-7 and MDA-MB-231. We then measured optimal doses of each drug, used in combination, in MCF-7 cells. These sub-IC50 doses were co-applied for all subsequent combined treatments to evaluate their synergistic effects on MCF-7 tumorigenic properties. Next, we examined expression levels of the genes crucial for apoptosis, cell growth, and EMT using RT-PCR or real-time PCR and monitored CD44/CD24 ratios using flow cytometry. Binding energies between shikonin and growth molecules were measured by in silico simulation.
Shikonin caused significantly reduced cell survival that was accelerated by the synergizing presence of metformin. Drug combination induced apoptosis and ROS levels while fully blocking cell migration and reverting EMT. RT-PCR showed strong suppression of BCL-2 but induction of BAX and PTEN. Prolonged shikonin treatment caused a total loss of the nuclear membrane, whereas metformin prevented this damage while promoting apoptotic morphologies. Our real-time PCR detected reduced levels of EMT genes but increases in the anti-EMT gene CDH1. Combined treatment also reduced CD44/CD24 ratios in favor of chemosensitivity. Binding energies strongly favored shikonin interactions with growth-signaling molecules.
Conclusions
Shikonin and metformin synergize in inhibiting the tumorigenic activities of MCF-7 cells including their proliferation, invasiveness, and EMT with a potential to inhibit multidrug resistance.





Similar content being viewed by others
Data availability
Any materials and data are available from the corresponding author on reasonable request.
Code availability
Not applicable.
References
Breast Cancer Treatment. National Cancer Institute. Updated 8 Apr, 2021. https://www.cancer.gov/types/breast/patient/breast-treatment-pdq#_125. Accessed 5 Jan 2022
DeSantis CE, Fedewa SA, Goding Sauer A, Kramer JL, Smith RA, Jemal A (2016) Breast cancer statistics, 2015: convergence of incidence rates between black and white women. CA Cancer J Clin 66:31–42
U.S. Breast Cancer Statistics. https://www.breastcancer.org/symptoms/understand_bc/statistics. Accessed 5 Jan 2022
Burrell RA, Swanton C (2014) Tumour heterogeneity and the evolution of polyclonal drug resistance. Mol Oncol 8:1095–1111. https://doi.org/10.1016/j.molonc.2014.06.005
Vasan N, Baselga J, Hyman DM (2019) A view on drug resistance in cancer. Nature 575:299–309. https://doi.org/10.1038/s41586-019-1730-1
Ichihashi N, Kitajima Y (2001) Chemotherapy induces or increases expression of multidrug resistance-associated protein in malignant melanoma cells. Br J Dermatol 144:745–750. https://doi.org/10.1046/j.1365-2133.2001.04129.x
Shibue T, Weinberg RA (2017) EMT, CSCs, and drug resistance: the mechanistic link and clinical implications. Nat Rev Clin Oncol 14:611–629. https://doi.org/10.1038/nrclinonc.2017.44
Liu Y, Li Q, Zhou L et al (2016) Cancer drug resistance redox resetting renders a way. Oncotarget 7:42740–42761
Phi LTH, Sari IN, Yang Y-G et al (2018) Cancer Stem Cells (CSCs) in drug resistance and their therapeutic implications in cancer treatment. Stem Cells Int 2018:5416923. https://doi.org/10.1155/2018/5416923
Li S, LI Q, (2014) Cancer stem cells and tumor metastasis. Int J Oncol 44:1806–1812. https://doi.org/10.3892/ijo.2014.2362
Zhao Y, Bao Q, Renner A et al (2011) Cancer stem cells and angiogenesis. Int J Dev Biol 55:477–482. https://doi.org/10.1387/ijdb.103225yz
Basmadjian C, Zhao Q, Bentouhami E, Djehal A, Nebigil CG, Johnson RA, Serova M, de Gramont A, Faivre S, Raymond E, Désaubry LG (2014) Cancer wars: natural products strike back. Front Chem 2:20. https://doi.org/10.3389/fchem.2014.00020
Zhan T, Rindtorff N, Betge J et al (2019) CRISPR/Cas9 for cancer research and therapy. Semin Cancer Biol 55:106–119. https://doi.org/10.1016/j.semcancer.2018.04.001
Yuan R, Hou Y, Sun W et al (2017) Natural products to prevent drug resistance in cancer chemotherapy: a review. Ann N Y Acad Sci 1401:19–27. https://doi.org/10.1111/nyas.13387
Guo C, He J, Song X et al (2019) Pharmacological properties and derivatives of shikonin—A review in recent years. Pharmacol Res 149:104463. https://doi.org/10.1016/j.phrs.2019.104463
Dowling RJ, Goodwin PJ, Stambolic V (2011) Understanding the benefit of metformin use in cancer treatment. BMC Med 9:33. https://doi.org/10.1186/1741-7015-9-33
Kasibhatla S, Amarante-Mendes GP, Finucane D, Brunner T, Bossy-Wetzel E, Green DR (2006) Acridine Orange/ethidium bromide (AO/EB) staining to detect apoptosis. CSH Protoc. https://doi.org/10.1101/pdb.prot4493
Eruslanov E, Kusmartsev S (2010) Identification of ROS using oxidized DCFDA and flow-cytometry. Methods Mol Biol 594:57–72. https://doi.org/10.1007/978-1-60761-411-1_4
Gardaneh M, Gholami M, Maghsoudi N (2011) Synergy between glutathione peroxidase-1 and astrocytic growth factors suppresses free radical generation and protects dopaminergic neurons against 6-hydroxydopamine. Rejuvenation Res 14:195–204. https://doi.org/10.1089/rej.2010.1080
Livak KJ, Schmittgen TD (2001) Analysis of relative gene expression data using real-time quantitative PCR and the 2−ΔΔCT method. Methods 25:402–408. https://doi.org/10.1006/meth.2001.1262
Gardaneh M, Nayeri Z, Akbari P et al (2020) Molecular simulations identify target receptor kinases bound by astaxanthin to induce breast cancer cell apoptosis. Arch Breast Cancer. https://doi.org/10.32768/abc.20207272-82
Wang T, Narayanaswamy R, Ren H, Torchilin VP (2016) Combination therapy targeting both cancer stem-like cells and bulk tumor cells for improved efficacy of breast cancer treatment. Cancer Biol Ther 17:698–707. https://doi.org/10.1080/15384047.2016.1190488
Fiorillo M, Tóth F, Sotgia F, Lisanti MP (2019) Doxycycline, Azithromycin and Vitamin C (DAV): A potent combination therapy for targeting mitochondria and eradicating cancer stem cells (CSCs). Aging (Albany NY) 11:2202–2216
Li W, Liu J, Jackson K et al (2014) Sensitizing the therapeutic efficacy of taxol with shikonin in human breast cancer cells. PLoS ONE 9:e94079. https://doi.org/10.1371/journal.pone.0094079
Goldman RD, Shumaker DK, Erdos MR et al (2004) Accumulation of mutant lamin A causes progressive changes in nuclear architecture in Hutchinson-Gilford progeria syndrome. Proc Natl Acad Sci 101:8963–8968. https://doi.org/10.1073/pnas.0402943101
Lopez-Mejia IC, Vautrot V, De Toledo M et al (2011) A conserved splicing mechanism of the LMNA gene controls premature aging. Hum Mol Genet 20:4540–4555. https://doi.org/10.1093/hmg/ddr385
Egesipe AL, Blondel S, Lo Cicero A, Jaskowiak AL, Navarro C, Sandre-Giovannoli A, Levy N, Peschanski M, Nissan X (2016) Metformin decreases progerin expression and alleviates pathological defects of Hutchinson-Gilford progeria syndrome cells. NPJ Aging Mech Dis 2:16026. https://doi.org/10.1038/npjamd.2016.26
Yeh YC, Liu TJ, Lai HC (2015) Shikonin induces apoptosis, necrosis, and premature senescence of human A549 lung cancer cells through upregulation of p53 expression. Evid Based Complement Alternat Med 2015:620383. https://doi.org/10.1155/2015/620383
Wang F, Mayca Pozo F, Tian D et al (2020) Shikonin inhibits cancer through P21 upregulation and apoptosis induction. Front Pharmacol 11:861. https://doi.org/10.3389/fphar.2020.00861
Bao C, Liu T, Qian L et al (2021) Shikonin inhibits migration and invasion of triple-negative breast cancer cells by suppressing epithelial-mesenchymal transition via miR-17-5p/PTEN/Akt pathway. J Cancer 12:76–88. https://doi.org/10.7150/jca.47553
Wiench B, Eichhorn T, Paulsen M, Efferth T (2012) Shikonin directly targets mitochondria and causes mitochondrial dysfunction in cancer cells. Evidence-Based Complement Altern Med 2012:726025. https://doi.org/10.1155/2012/726025
Verma NK, Dourlat J, Davies AM et al (2009) STAT3-Stathmin interactions control microtubule dynamics in migrating t-cells. J Biol Chem 284:12349–12362. https://doi.org/10.1074/jbc.M807761200
Trinh SX, Nguyen HTB, Saimuang K et al (2017) Metformin inhibits migration and invasion of cholangiocarcinoma cells. Asian Pac J Cancer Prev 18:473–477
Cao HH, Liu DY, Lai YC, Chen YY, Yu LZ, Shao M, Liu JS (2020) Inhibition of the STAT3 signaling pathway contributes to the anti-melanoma activities of shikonin. Front Pharmacol 11:748. https://doi.org/10.3389/fphar.2020.00748
Schexnayder C, Broussard K, Onuaguluchi D, Poché A, Ismail M, McAtee L, Llopis S, Keizerweerd A, McFerrin H, Williams C (2018) Metformin inhibits migration and invasion by suppressing ROS production and COX2 expression in MDA-MB-231 breast cancer cells. Int J Mol Sci 19(11):3692. https://doi.org/10.3390/ijms19113692
Chang I-C, Huang Y-J, Chiang T-I et al (2010) Shikonin induces apoptosis through reactive oxygen species/extracellular signal-regulated kinase pathway in osteosarcoma cells. Biol Pharm Bull 33:816–824. https://doi.org/10.1248/bpb.33.816
Zhang Z, Zhang Z, Li Q et al (2017) Shikonin induces necroptosis by reactive oxygen species activation in nasopharyngeal carcinoma cell line CNE-2Z. J Bioenerg Biomembr 49:265–272. https://doi.org/10.1007/s10863-017-9714-z
Algire C, Moiseeva O, Deschênes-Simard X et al (2012) Metformin reduces endogenous reactive oxygen species and associated DNA damage. Cancer Prev Res 5:536–543. https://doi.org/10.1158/1940-6207.CAPR-11-0536
Marinello PC, Panis C, Silva TNX et al (2019) Metformin prevention of doxorubicin resistance in MCF-7 and MDA-MB-231 involves oxidative stress generation and modulation of cell adaptation genes. Sci Rep 9:5864. https://doi.org/10.1038/s41598-019-42357-w
Li W, Ma H, Zhang J, Zhu L, Wang C, Yang Y (2017) Unraveling the roles of CD44/CD24 and ALDH1 as cancer stem cell markers in tumorigenesis and metastasis. Sci Rep 7(1):13856. https://doi.org/10.1038/s41598-017-14364-2.Erratum.In:SciRep.2018Mar6;8(1):4276
Toole BP (2009) Hyaluronan-CD44 interactions in cancer: paradoxes and possibilities. Clin Cancer Res 15:7462–7468. https://doi.org/10.1158/1078-0432.CCR-09-0479
Misra S, Ghatak S, Toole BP (2005) Regulation of MDR1 expression and drug resistance by a positive feedback loop involving hyaluronan, phosphoinositide 3-kinase, and ErbB2. J Biol Chem 280:20310–20315. https://doi.org/10.1074/jbc.M500737200
Gilg AG, Tye SL, Tolliver LB et al (2008) Targeting Hyaluronan Interactions in Malignant Gliomas and Their Drug-Resistant Multipotent Progenitors. Clin Cancer Res 14:1804–1813. https://doi.org/10.1158/1078-0432.CCR-07-1228
Chen C, Zhao S, Karnad A, Freeman JW (2018) The biology and role of CD44 in cancer progression: therapeutic implications. J Hematol Oncol 11:64. https://doi.org/10.1186/s13045-018-0605-5
Han W, Li L, Qiu S et al (2007) Shikonin circumvents cancer drug resistance by induction of a necroptotic death. Mol Cancer Ther 6:1641–1649. https://doi.org/10.1158/1535-7163.MCT-06-0511
Wu H, Xie J, Pan Q et al (2013) Anticancer agent shikonin is an incompetent inducer of cancer drug resistance. PLoS ONE 8:e52706. https://doi.org/10.1371/journal.pone.0052706
Coyle C, Cafferty FH, Vale C, Langley RE (2016) Metformin as an adjuvant treatment for cancer: a systematic review and meta-analysis. Ann Oncol 27:2184–2195. https://doi.org/10.1093/annonc/mdw410
Funding
This study was financially supported by a grant from National Institute of Genetic Engineering and Biotechnology (NIGEB) (Grant 589).
Author information
Authors and Affiliations
Contributions
ART carried out most of the experiments. PG designed and implemented a part of experiments including invasion and cell co-staining plus molecular docking. FS contributed to the dose determination of shikonin and metformin as well as editing and reviewing the manuscript. MG was a grantee of the project, supervised the first author, and designed the whole structure of the manuscript in detail.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Tabari, A.R., Gavidel, P., Sabouni, F. et al. Synergy between sublethal doses of shikonin and metformin fully inhibits breast cancer cell migration and reverses epithelial-mesenchymal transition. Mol Biol Rep 49, 4307–4319 (2022). https://doi.org/10.1007/s11033-022-07265-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11033-022-07265-9