Abstract
Background
In some stent implanted patients, cardiovascular events (CE) may occur. Acetylsalicylic acid (ASA) is routinely administered to these patients in order to prevent the occurrence of CE. CE may be related to gene variations which cause ASA resistance (AR). Therefore, it was aimed to investigate the relationship between COX-1, COX-2, CYP2C9 and CYP2C19 variations with CE due to AR.
Materials and results
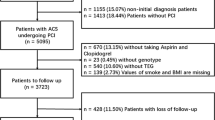
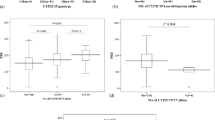
Seventy-four stent implanted patients, using 100 mg of ASA per day during five years were enrolled into the study. Following stent implantation, thirty-eight patients who had a CE within five years due to AR and 36 patients without CE were enrolled in patient and control group, respectively. AR was confirmed by platelet aggregation testing. After DNA isolation from blood; COX-1, COX-2, CYP2C19 and CYP2C9 variations were investigated with real-time polymerase chain reaction. At the end of this study, heterozygous genotype of COX-1 was found statistically high in patients whereas heterozygous genotype of CYP2C19*17 was found statistically high in controls. The presence of C and G allele in COX-1 and COX-2 were found statistically high in patients, respectively. The presence of T allele in CYP2C19*17 was found statistically high in controls. Heterozygous genotype of COX-1 variation was found statistically high in patients who have AR. Additionally heterozygous genotype of CYP2C19*17 was found statistically high in patients who have low thrombosis risk.
Conclusions
COX-1 and COX-2 gene mutations may increase the risk of CE due to AR whereas CYP2C19*17 may have a protective effect in this process.


Similar content being viewed by others
Data availability
Yes.
Code availability
Not applicable.
References
Cai G, Zhou W, Lu Y, Chen P, Lu Z, Fu Y (2015) Aspirin resistance and other aspirin-related concerns. Neurol Sci 37(2):181–189. https://doi.org/10.1007/s10072-015-2412-x
Hankey GJ, Eikelboom JW (2006) Aspirin resistance. Lancet 367(9510):606–617. https://doi.org/10.1016/S0140-6736(06)68040-9
Zhao L, Fang J, Zhou M, Zhou J, Yu L, Chen N, He L (2019) Interaction between COX-1 and COX-2 increases susceptibility to ischemic stroke in a Chinese population. BMC Neurol 19(1):1–12. https://doi.org/10.1186/s12883-019-1505-1
Ornelas A, Zacharias-Millward N, Menter DG, Davis JS, Lichtenberger L, Hawke D, Hawk E, Vilar E, Bhattacharya P, Millward S (2017) Beyond COX-1: the effects of aspirin on platelet biology and potential mechanisms of chemoprevention. Cancer Metastasis Rev 36(2):289–303. https://doi.org/10.1007/s10555-017-9675-z
Lazar A, Tomalik-Scharte D, Fuhr U (2004) Applications of genotyping and phenotyping for clinically-relevant polymorphisms of drug metabolizing enzymes and drug transporters. Drug monitoring and clinical chemistry, handbook of analytical separations, 1st edn. Elsevier, Amsterdam, pp 321–353
Botton MR, Lu X, Zhao G, Repnikova E, Seki Y, Gaedigk A, Schadt EE, Edelmann L, Scott SA (2019) Structural variation at the CYP2C locus: characterization of deletion and duplication alleles. Hum Mutat. https://doi.org/10.1002/humu.23855
Mourão AOM, Gomes KB, Reis EA, Souza RP, Campos EIF, Ribeiro DD, Rocha MOC, Martins MAP (2019) Algorithm for predicting low maintenance doses of warfarin using age and polymorphisms in genes CYP2C9 and VKORC1 in Brazilian subjects. Pharmacogenomics J. https://doi.org/10.1038/s41397-019-0091-3
Al-Eitan LN, Almasri AY, Khasawneh RH (2019) Effects of CYP2C9 and VKORC1 polymorphisms on warfarin sensitivity and responsiveness during the stabilization phase of therapy. Saudi Pharm J. https://doi.org/10.1016/j.jsps.2019.01.011
Kirac D, Erdem A, Avcilar T, Yesilcimen K, Guney AI, Emre A, Yazici S, Terzi S, Kaspar EC, Cetin SE, Isbir T (2016) Effects of genetic factors to stent thrombosis due to clopidogrel resistance after coronary stent placement. Cell Mol Biol 62(1):51–55
Li Z, Dong W, Yang D, Sun L, He X, Hu H, Zhang J, Wang C, Li Y, Zhao M, Kong Y, Wang Y (2020) Body weight, CYP2C19, and P2Y12 receptor polymorphisms relate to clopidogrel resistance in a cohort of Chinese ischemic stroke patients with aspirin intolerance. Eur J Clin Pharmacol 76(11):1517–1527. https://doi.org/10.1007/s00228-020-02946-5
Stys TP, Gedela M, Gowda SN, Bares V, Fanta L, Petrasko M, Hajek C, Larson E, Stys AT (2021) CYP2C19 genotype-directed P2Y12 inhibitor antiplatelet therapy normalizes risk for major adverse cardiovascular events after percutaneous coronary intervention. Indian Heart J 73(3):281–288. https://doi.org/10.1016/j.ihj.2021.03.004
Zhu WY, Zhao T, Xiong XY, Li J, Wang L, Zhou Y, Gong ZL, Cheng SY, Liu Y, Shuai J, Yang QW (2016) Association of CYP2C19 polymorphisms with the Clinical efficacy of clopidogrel therapy in patients undergoing carotid artery stenting in Asia. Sci Rep 6(1):25478. https://doi.org/10.1038/srep25478
Lewis JP, Stephens SH, Horenstein RB, O’Connell JR, Ryan K, Peer CJ, Figg WD, Spencer SD, Pacanowski MA, Mitchell BD, Shuldiner AR (2013) The CYP2C19*17 variant is not independently associated with clopidogrel response. J Thromb Haemost 11(9):1640–1646. https://doi.org/10.1007/s00228-020-02946-5.10.1111/jth.12342
Liu X, Xu H, Xu H, Geng Q, Mak WH, Ling F, Su Z, Yang F, Zhang T, Chen J, Yang H, Wang J, Zhang X, Xu X, Jia H, Zhang Z, Liu X, Zhong S (2021) New genetic variants associated with major adverse cardiovascular events in patients with acute coronary syndromes and treated with clopidogrel and aspirin. Pharmacogenomics J 21(6):664–672. https://doi.org/10.1038/s41397-021-00245-5
Han Y (2016) Aspirin resistance in coronary heart disease: current understandings and strategies. J Transl Int Med 4(1):7–10. https://doi.org/10.1515/jtim-2016-0002
Sisodia P, Bhatia R (2018) Aspirin resistance and stroke. J Stroke Med 1(1):19–27. https://doi.org/10.1177/2516608518777017
Cansu DU, Akay OM, Cantürk Z, Gul Z (2008) Aspirin resistance frequency in healthy males. Turk J Hematol 25:83–86
Townsend N, Nichols M, Scarborough P, Rayner M (2015) Cardiovascular disease in Europe—epidemiological update 2015. Eur Heart J 36(40):2696–2705
Cambria-Kiely JA, Gandhi PJ (2002) Aspirin resistance and genetic polymorphisms. J Thromb Thrombolysis 14(1):51–58. https://doi.org/10.1023/a:1022066305399
Gonzalez-Conejero R, Corral J, Guerrero JA, Iniesta JA, Rivera J, Arriba VV (2004) Genetic variants of the extra-large stimulatory Gs protein alpha-subunit and risk of thrombotic and haemorrhagic disorders. Br J Haematol 125(5):621–628. https://doi.org/10.1111/j.1365-2141.2004.04947.x
Clappers N, van Oijen MG, Sundaresan S, Brouwer MA, Morsche RHMT, Keuper W, Peters WHM, Drenth JPH, Verheugt FWA (2008) The C50T polymorphism of the cyclooxygenase-1 gene and the risk of thrombotic events during low-dose therapy with acetyl salicylic acid. Thromb Haemost 100(1):70–75. https://doi.org/10.1160/TH08-03-0172
Chakroun T, Addad F, Yacoub S, Abderrezak F, Gerotziafas GT, Abdelkafi D, Hassine M, Gamra G, Hatmi M, Elalamy I (2011) The cyclooxygenase-1 C50T polymorphism is not associated with aspirin responsiveness status in stable coronary artery disease in Tunisian patients. Genet Test Mol Biomark 15(7–8):513–516. https://doi.org/10.1089/gtmb.2010.0225
Cao L, Zhang Z, Sun W, Bai W, Sun E, Zhang Y, Wang X, Cai B, Xie X, Duan Z, Cai Q, Liu D, Xiong Y, Ma M, Liu X, Xu G (2014) Impacts of COX-1 gene polymorphisms on vascular outcomes in patients with ischemic stroke and treated with aspirin. Gene 546(2):172–176. https://doi.org/10.1016/j.gene.2014.06.023
Wang Z, Chen Y, Hu S, Liu R (2017) A meta-analysis of the association of COX-1 gene rs3842788 and rs1330344 polymorphism with aspirin resistance in Chinese. J Med Diagn Meth 6(4):1–4. https://doi.org/10.4172/2168-9784.1000255
Li XQ, Ma N, Li XG, Wang B, Sun SS, Gao F, Mo DP, Song LG, Sun X, Liu L, Zhao XQ, Wang LY, Wang YJ, Zhao ZG, Miao ZR (2016) Association of PON1, P2Y12 and COX1 with recurrent ischemic events in patients with extracranial or ıntracranial stenting. PLoS ONE 11(2):1–12. https://doi.org/10.1371/journal.pone.0148891
Fan L, Cao J, Liu L, Hu Y, Zhu B (2013) Frequency, risk factors, prognosis, and genetic polymorphism of the cyclooxygenase-1 gene for aspirin resistance in elderly Chinese patients with cardiovascular disease. Gerontology 59(2):122–131. https://doi.org/10.1159/000342489
Zhang MM, Xie X, Ma YT, Zheng YY, Yang YN, Li XM, Fu ZY, Liu F, Chen BD (2015) Association of COX-2 -765G>C genetic polymorphism with coronary artery disease: a meta-analysis. Int J Clin Exp Med 8(5):7412–7418
Sharma V, Kaul S, Al-Hazzani A, Jyothy A, Munshi A (2012) Association of COX-2 rs20417 with aspirin resistance. J Thromb Thrombolysis 35(1):95–99. https://doi.org/10.1007/s11239-012-0777-8
Yi X, Cheng W, Lin J, Zhou Q, Wang C (2016) Interaction between COX-1 and COX-2 variants associated with aspirin resistance in Chinese stroke patients. J Stroke Cerebrovasc Dis 25(9):2136–2144. https://doi.org/10.1016/j.jstrokecerebrovasdis.2016.05.039
Weng Z, Li X, Li Y, Peng F, Niu W (2013) The association of four common polymorphisms from four candidate genes (COX-1, COX-2, ITGA2B, ITGA2) with aspirin insensitivity: a meta-analysis. PLoS ONE 8(11):1–7. https://doi.org/10.1371/journal.pone.0078093
Ercan B, Ayaz L, Cicek D, Tamer L (2008) Role of CYP2C9 and CYP2C19 polymorphisms in patients with atherosclerosis. Cell Biochem Funct 26(3):309–313. https://doi.org/10.1002/cbf.1437
Yasar U, Bennet AM, Eliasson E, Lundgren S, Wiman B, Faire UD, Rane A (2003) Allelic variants of cytochromes P450 2C modify the risk for acute myocardial infarction. Pharmacogenetics 13(12):715–720. https://doi.org/10.1097/00008571-200312000-00002
Dai D, Zeldin DC, Blaisdell JA, Chanas B, Coulter SJ, Ghanayem BI, Goldstein JA (2001) Polymorphisms in human CYP2C8 decrease metabolism of the anticancer drug paclitaxel and arachidonic acid. Pharmacogenetics 11(7):597–607. https://doi.org/10.1097/00008571-200110000-00006
Visser LE, van Schaik RHN, van Vliet M, Trienekens PH, De Smet PAGM, Vulto AG, Hofman A, van Duijn CM, Stricker BHC (2004) The risk of bleeding complications in patients with cytochrome P450 CYP2C9*2 or CYP2C9*3 alleles on acenocoumarol or phenprocoumon. Thromb Haemost. https://doi.org/10.1160/TH03-12-0741
Fichtlscherer S (2004) Inhibition of cytochrome P450 2C9 improves endothelium-dependent, nitric oxide-mediated vasodilatation in patients with coronary artery disease. Circulation 109(2):178–183. https://doi.org/10.1161/01.CIR.0000105763.51286.7F
Liu T, Yin T, Li Y, Yu J, Si R, Zhang YM, He Y, Guo WY, Wang HC (2014) CYP2C19 polymorphisms and coronary heart disease risk factors synergistically impact clopidogrel response variety after percutaneous coronary intervention. Coron Artery Dis 25(5):412–420. https://doi.org/10.1097/MCA.0000000000000092
Yamamoto K, Hokimoto S, Chitose T, Morita K, Ono T, Kaikita K, Tsujita K, Abe T, Deguchi D, Miyagawa H, Saruwatari J, Sumida H, Sugiyama S, Nakagawa K, Ogawa H (2011) Impact of CYP2C19 polymorphism on residual platelet reactivity in patients with coronary heart disease during antiplatelet therapy. J Cardiol 57(2):194–201. https://doi.org/10.1016/j.jjcc.2010.10.007
Zou JJ, Xie HG, Chen SL, Tan J, Lin L, Zhao YY, Xu HM, Lin S, Zhang J, Wang GJ (2012) Influence of CYP2C19 loss-of-function variants on the antiplatelet effects and cardiovascular events in clopidogrel-treated Chinese patients undergoing percutaneous coronary intervention. Eur J Clin Pharmacol 69(4):771–777. https://doi.org/10.1007/s00228-012-1392-5
Bauer T, Bouman HJ, van Werkum JW, Ford NF, Berg JM, Taubert D (2011) Impact of CYP2C19 variant genotypes on clinical efficacy of antiplatelet treatment with clopidogrel: systematic review and meta-analysis. BMJ 343:1–18. https://doi.org/10.1136/bmj.d4588
Saydam F, Degirmenci I, Birdane A, Ozdemir M, Ulus T, Ozbayer C, Çolak E, Ata N, Gunes HV (2017) The CYP2C19*2 and CYP2C19*17 polymorphisms play a vital role in clopidogrel responsiveness after percutaneous coronary ıntervention: a pharmacogenomics study. Basic Clin Pharmacol Toxicol 121(1):29–36. https://doi.org/10.1111/bcpt.12763
Funding
The authors did not receive support from any organization for the submitted work.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by [DK, AEY, TD, MM and ECK]. The first draft of the manuscript was written by [DK and TD]. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All the authors declare no conflict of interest.
Ethical approval
Ethical approval was obtained from Ethics Committee of Yeditepe University (Approval number: 1054, Approval date: 27.06.2019).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kirac, D., Yaman, A.E., Doran, T. et al. COX-1, COX-2 and CYP2C19 variations may be related to cardiovascular events due to acetylsalicylic acid resistance. Mol Biol Rep 49, 3007–3014 (2022). https://doi.org/10.1007/s11033-022-07124-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11033-022-07124-7