Abstract
Background
Cardiovascular diseases (CVDs) are the most common and the first cause of death worldwide. While some studies have investigated the association of the Adenosine Deaminase (ADA) gene with CDVs, its roles on in-stent restenosis (ISR) has not been studied.
Methods and results
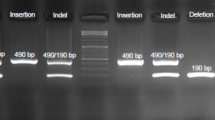
In this study, we investigated the role of ADA gene variants in both genetic and haplotype models on the risk of ISR. 91 samples were included in this study. The subjects were divided into two groups regarding having or not-having ISR (n = 40 ISR+ and n = 51 ISR−). The genotyping for G22A (rs73598374) and A4223C (rs452159) polymorphisms was performed using PCR–RFLP method. Statistical analysis was performed by SPSS v. 20 and Haploview 4.2 softwares. The basic demographic conditions in ISR groups were statistically similar. There was a significant association between A allele of rs452159 ISR groups after adjustment (allelic model: P value = 0.028, OR(95%CI) = 0.366(0.149–0.899)), while rs73598374 polymorphism shows no significant association with ISR. In haplotype analysis, the GA (G:rs73598374/A:rs452159) haplotype decreased the risk of ISR (P value = 00.025, OR(95%CI) = 0.382(0.161–0.907)).
Conclusions
This study suggests that A allele of ADA rs452159 polymorphism and GA (G:rs73598374/A:rs452159) haplotype may be related to decreased risk of ISR in CAD patients receiving drug-eluting stent and offers more observational studies on ADA variants in other populations to generate a potential haplotype panel for ISR risk assessment.


Similar content being viewed by others
References
Organization WH (2017) https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds)
Goff DC, Lloyd-Jones DM, Bennett G, Coady S, D’agostino RB, Gibbons R, Greenland P, Lackland DT, Levy D, O’donnell CJ (2014) 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. J Am Coll Cardiol 63(25 Part B):2935–59
Alraies MC, Darmoch F, Tummala R, Waksman R (2017) Diagnosis and management challenges of in-stent restenosis in coronary arteries. World J Cardiol 9(8):640
Alfonso F, Byrne RA, Rivero F, Kastrati A (2014) Current treatment of in-stent restenosis. J Am Coll Cardiol 63(24):2659–2673
Dangas GD, Claessen BE, Caixeta A, Sanidas EA, Mintz GS, Mehran R (2010) In-stent restenosis in the drug-eluting stent era. J Am Coll Cardiol 56(23):1897–1907
Hytönen J, Leppänen O, Braesen JH, Schunck WH, Mueller D, Jung F, Mrowietz C, Jastroch M, Von Bergwelt-Baildon M, Kappert K (2016) Activation of peroxisome proliferator–activated receptor-δ as novel therapeutic strategy to prevent in-stent restenosis and stent thrombosis. Arterioscler Thromb Vasc Biol 36(8):1534–1548
Lee KJ, Park SH, Lee JY, Joo HC, Jang EH, Youn Y-N, Ryu W (2014) Perivascular biodegradable microneedle cuff for reduction of neointima formation after vascular injury. J Control Release 192:174–181
Xuan C, Tian QW, Zhang SY, Li H, Tian TT, Zhao P, Yue K, Ling YY, He GW, Lun LM (2019) Serum adenosine deaminase activity and coronary artery disease: a retrospective case-control study based on 9929 participants. Ther Adv Chronic Dis. https://doi.org/10.1177/2040622319891539
Verdoia M, Tonon F, Gioscia R, Nardin M, Fierro N, Sagazio E, Negro F, Pergolini P, Rolla R, De Luca G (2020) Impact of the rs73598374 polymorphism of the adenosine deaminase gene on platelet reactivity and long-term outcomes among patients with acute coronary syndrome treated with ticagrelor. Thromb Res 196:231–237
Simard T, Jung RG, Di Santo P, Ramirez FD, Labinaz A, Gaudet C, Motazedian P, Parlow S, Joseph J, Moreland R (2021) Performance of plasma adenosine as a biomarker for predicting cardiovascular risk. Clin Transl Sci 14(1):354–361
Samuel CE (2020) Adenosine deaminases. In: Reference module in life sciences. Elsevier, Amsterdam
Reiss AB, Grossfeld D, Kasselman LJ, Renna HA, Vernice NA, Drewes W, Konig J, Carsons SE, DeLeon J (2019) Adenosine and the cardiovascular system. Am J Cardiovasc Drugs 19(5):449–464
Singh L, Kulshrestha R, Singh N, Jaggi AS (2018) Mechanisms involved in adenosine pharmacological preconditioning-induced cardioprotection. Korean J Physiol Pharmacol 22(3):225–234
Valdes F, Brown N, Morales-Bayuelo A, Prent-Peñaloza L, Gutierrez M (2019) Adenosine derivates as antioxidant agents: synthesis, characterization, in vitro activity, and theoretical insights. Antioxidants 8(10):468
Koupenova M, Johnston-Cox H, Ravid K (2012) Regulation of atherosclerosis and associated risk factors by adenosine and adenosine receptors. Curr Atheroscler Rep 14(5):460–468
Teng B, Tilley S, Ledent C, Mustafa S (2015) Effect of adenosine on coronary blood flow and cardiac function in vivo using adenosine receptor knockout mice. FASEB J 29(644):7
Paganelli F, Gaudry M, Ruf J, Guieu R (2021) Recent advances in the role of the adenosinergic system in coronary artery disease. Cardiovasc Res 117(5):1284–1294
Sousa JB, Diniz C (2017) The adenosinergic system as a therapeutic target in the vasculature: new ligands and challenges. Molecules 22(5):752
Chen J-F, Eltzschig HK, Fredholm BB (2013) Adenosine receptors as drug targets—what are the challenges? Nat Rev Drug Discov 12(4):265–286
Megaly M, Glogoza M, Xenogiannis I, Vemmou E, Nikolakopoulos I, Omer M, Willson L, Monyak DJ, Sullivan P, Stanberry L (2021) Outcomes with combined laser Atherectomy and intravascular brachytherapy in recurrent drug-eluting stent in-stent restenosis. Cardiovasc Revasc Med 22:29–33
Mehran R, Dangas G, Abizaid AS, Mintz GS, Lansky AJ, Satler LF, Pichard AD, Kent KM, Stone GW, Leon MB (1999) Angiographic patterns of in-stent restenosis: classification and implications for long-term outcome. Circulation 100(18):1872–1878
Association AD (2014) Diagnosis and classification of diabetes mellitus. Diabetes Care 37(Supplement 1):S81–S90
Expert Committee on the Diagnosis and Classification of Diabetes Mellitus (2003) Follow-up report on the diagnosis of diabetes mellitus. Diabetes care 26(11):3160–3167
Martin SS, Blumenthal RS (2014) Concepts and controversies: the 2013 American College of Cardiology/American Heart Association risk assessment and cholesterol treatment guidelines. American College of Physicians. Ann Intern Med 160(5):356–358
Pencina MJ, Navar-Boggan AM, D’Agostino RB Sr, Williams K, Neely B, Sniderman AD, Peterson ED (2014) Application of new cholesterol guidelines to a population-based sample. N Engl J Med 370:1422–1431
Kaur J (2014) A comprehensive review on metabolic syndrome. Cardiol Res Pract 2014:21. https://doi.org/10.1155/2014/943162
Grundy SM, Brewer HB Jr, Cleeman JI, Smith SC Jr, Lenfant C (2004) Definition of metabolic syndrome: report of the National Heart, Lung, and Blood Institute/American Heart Association conference on scientific issues related to definition. Circulation 109(3):433–438
Gholami M, Amoli MM, Sharifi F (2019) Letter to the editor: comments on “Association between the ICAM-1 gene polymorphism and coronary heart disease risk: a meta-analysis.” Biosci Rep. https://doi.org/10.1042/BSR20190554
Hershfield M (2006) Adenosine deaminase deficiency. GeneReviews® [Internet]. University of Washington, Seattle WA. 1993–2021. PMID: 20301656
Flinn AM, Gennery AR (2018) Adenosine deaminase deficiency: a review. Orphanet J Rare Dis 13(1):1–7
Cheema AN, Rosenthal SL, Kamboh I (2017) Proficiency of data interpretation: identification of signaling SNPs/specific loci for coronary artery disease. Database. https://doi.org/10.1093/database/bax078
Boyle AP, Hong EL, Hariharan M, Cheng Y, Schaub MA, Kasowski M, Karczewski KJ, Park J, Hitz BC, Weng S (2012) Annotation of functional variation in personal genomes using RegulomeDB. Genome Res 22(9):1790–1797
Dong S, Boyle P (2019) Predicting functional variants in enhancer and promoter elements using RegulomeDB. Hum Mutat 40(9):1292–1298
He H-R, Li Y-J, He G-H, Wang Y-J, Zhai Y-J, Xie J, Zhang W-P, Dong Y-L, Lu J (2014) The adenosine deaminase gene polymorphism is associated with chronic heart failure risk in Chinese. Int J Mol Sci 15(9):15259–15271
Khodadadi I (2014) Mini review from the molecular base to the diagnostic value of adenosine deaminase. Avicenna J Med Biochem 2(2):e24310
Riksen NP, Franke B, van den Broek P, Naber M, Smits P, Rongen GA (2008) The 22G> A polymorphism in the adenosine deaminase gene impairs catalytic function but does not affect reactive hyperaemia in humans in vivo. Pharmacogenet Genomics 18(10):843–846
Safranow K, Dziedziejko V, Rzeuski R, Czyżycka E, Bukowska H, Wojtarowicz A, Bińczak-Kuleta A, Jakubowska K, Olszewska M, Ciechanowicz A (2016) Inflammation markers are associated with metabolic syndrome and ventricular arrhythmia in patients with coronary artery disease. Adv Hyg Exp Med/Postepy Hig Med Dosw 70:56–66
Saccucci P, Binczak-Kuleta A, Banci M, Krzysztalowska M, Dofcaci A, Safranow K, Magrini A, Loniewska B, Kornacewicz-Jach Z, Chlubek D (2014) Coronary artery disease. A study of three polymorphic sites of adenosine deaminase gene. Acta Cardiol 69(1):39–44
Acknowledgements
Research reported in this publication was supported by Elite Researcher Grant Committee under Award Number [987686] from the National Institute for Medical Research Development (NIMAD), Tehran, Iran.
Funding
Research reported in this publication was supported by Elite Researcher Grant Committee under Award Number [987686] from the National Institute for Medical Research Development (NIMAD), Tehran, Iran.
Author information
Authors and Affiliations
Contributions
All authors (MG, SBD, MM, MMA) contributed to the study conception and design. MM and SBD provided clinical data about patients. MG and SBD carried out the experiment. The data collection and analysis were performed by MG and MMA. The first draft of the manuscript was written by MG with support from MMA and all authors commented on previous versions of the manuscript and discussed the results. MMA supervised the project and approved the final version. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare that are relevant to the content of this article.
Ethical approval
This study was approved by the institutional Ethical Review Boards of the National Institute for Medical Research Development (NIMAD).
Informed consent
Informed consent was obtained from all subjects. All authors are agree to publish this manuscript in your valuable journal.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gholami, M., Borhan Dayani, S., Mehrpooya, M. et al. ADA gene haplotype is associated with coronary-in-stent-restenosis. Mol Biol Rep 48, 6665–6671 (2021). https://doi.org/10.1007/s11033-021-06574-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11033-021-06574-9