Abstract
Liver cancer is the sixth most common cancer and the fourth leading cause of cancer deaths in the world. The most common type of liver cancers is hepatocellular carcinoma (HCC). Autophagy is the cellular digestion of harmful components by sequestering the waste products into autophagosomes followed by lysosomal degradation for the maintenance of cellular homeostasis. The impairment of autophagy is highly associated with the development and progression of HCC although autophagy may be involved in tumour-suppressing cellular events. In regards to its protecting role, autophagy also shelters the cells from anoikis- a programmed cell death in anchorage-dependent cells detached from the surrounding extracellular matrix which facilitates metastasis in HCC. Liver cancer stem cells (LCSCs) have the ability for self-renewal and differentiation and are associated with the development and progression of HCC by regulating stemness, resistance and angiogenesis. Interestingly, autophagy is also known to regulate normal stem cells by promoting cellular survival and differentiation and maintaining cellular homeostasis. In this review, we discuss the basal autophagic mechanisms and double-faceted roles of autophagy as both tumour suppressor and tumour promoter in HCC, as well as its association with and contribution to self-renewal and differentiation of LCSCs.




Similar content being viewed by others
Abbreviations
- HCC:
-
Hepatocellular carcinoma
- HBV:
-
Hepatitis B virus
- HCV:
-
Hepatitis C virus
- CSC:
-
Cancer stem cell
- PI3K:
-
Phosphatidylinositol 3-kinase
- VPS34:
-
Vacuolar protein sorting 34
- mTORC1:
-
Mammalian target of rapamycin complex
- ULK1:
-
Unc-51 like kinase 1
- ATG:
-
Autophagy related protein
- FIP200:
-
Focal adhesion kinase family-interacting protein 200 kDa
- AMPK:
-
5` Adenosine monophosphate-activated protein kinase
- PI3P:
-
Phosphatidylinositol triphosphate
- LC3:
-
Microtubule-associated protein 1A/1B-light chain 3
- PE:
-
Phosphatidylethanolamine
- SQSTM1/p62:
-
Sequestosome-1/ubiquitin-binding protein p62
- NIX:
-
BNIP3L/Receptor for mitochondrial protein
- OPTN:
-
Optineurin
- LAMP2:
-
Lysosome-associated membrane protein 2
- GRASP55:
-
Golgi reassembly-stacking protein 55
- EMS:
-
Eukaryotic endomembrane system
- ILVs:
-
Intraluminal vesicles
- MVBs:
-
Multivesicular bodies
- MDB:
-
Mallory-Denk bodies
- ATP:
-
Adenosine triphosphate
- ROS:
-
Reactive oxygen species
- RNS:
-
Reactive nitrogen species
- Nrf2-Keap1:
-
Nuclear factor erythroid 2-related factor 2-kelch-like ECH-associated protein 1
- HIF:
-
Hypoxia inducible factor
- BNIP3:
-
BCL2 and adenovirus E1B 19-kDa-interacting protein 3
- BNIP3L:
-
BCL2: adenovirus E1B 19-kDa-interacting protein 3-like
- COX2:
-
Cyclooxygenase-2
- PGE2:
-
Prostaglandin E(2)
- TNM:
-
Tumour, node, metastasis
- CTC:
-
Circulatory tumour cells
- EMT:
-
Epithelial-mesenchymal transition
- TGF-β:
-
Transforming growth factor β
- TRAF6:
-
Tumour necrosis factor receptor-associated factor-6
- TAK1:
-
TGF-β activated kinase 1
- DRAM1:
-
DNA damage modulator 1
- CREB:
-
CAMP response element binding
- HO-1:
-
ROS/heme oxygenase 1
- UPR:
-
Unfolded protein response
- HSP:
-
Heat shock protein
- 5-FU:
-
5-Fluorouracil
- TAE:
-
Transarterial embolization
- TACE:
-
Transarterial chemoembolization
- Egr-1:
-
Early growth response-1
- IR:
-
Ionizing radiation
- VEGFR:
-
Vascular endothelial growth factor receptor
- PDGFR-β:
-
Platelet-derived growth factor receptor β
- GSTM1:
-
Glutathione transferase Mu 1
- LCSC:
-
Liver cancer stem cells
- AFP:
-
Alpha fetoprotein
- FGFs:
-
Fibroblast growth factors
- ECM:
-
Extracellular matrix
- SIRT1 :
-
Gene encoding Sirtuin1 protein
- ALDH:
-
Aldehyde dehydrogenase
- ABC:
-
ATP-binding cassette
- 4-HNE:
-
4-Hydroxy-2-nonenal
- NAD:
-
Nicotinamide adenosine dinucleotide
- MEK:
-
Mitogen-activated protein kinase
- MRPS5:
-
Mitochondrial ribosomal protein S5
- AC:
-
Acetyl
- TCF/LEF:
-
T-cell factor/lymphoid enhancer factor
- CSL, CBF-1:
-
Suppressor hairless lag-1
- MAML:
-
Mastermind-like protein
- NICD:
-
Notch intracellular domain
- NECD:
-
Notch extracellular domain
- LSD1:
-
Lysine demethylase 1
- UPRmt:
-
Mitochondrial unfolded protein response
- HPC/LPC:
-
Hepatic/liver progenitor cells
- PINK1:
-
PTEN-induced putative kinase
- HGF:
-
Hepatocyte growth factor
- FGFR:
-
Fibroblast growth factor receptor
References
Mathew R, Karantza-Wadsworth V, White E (2007) Role of autophagy in cancer. Nat Rev Cancer 7:961–967. https://doi.org/10.1038/nrc2254
King JS (2012) Autophagy across the eukaryotes: is S. cerevisiae the odd one out? Autophagy 8:1159–1162. https://doi.org/10.4161/auto.20527
Tsukada M, Ohsumi Y (1993) Isolation and characterization of autophagy-defective mutants of Saccharomyces cerevisiae. FEBS Lett 333:169–174. https://doi.org/10.1016/0014-5793(93)80398-e
Abounit K, Scarabelli TM, McCauley RB (2012) Autophagy in mammalian cells. World J Biol Chem 3:1–6. https://doi.org/10.4331/wjbc.v3.i1.1
Weidberg H, Shvets E, Elazar Z (2011) Biogenesis and cargo selectivity of autophagosomes. Annu Rev Biochem 80:125–156. https://doi.org/10.1146/annurev-biochem-052709-094552
Lee MS (2014) Role of islet β cell autophagy in the pathogenesis of diabetes. Trends Endocrinol Metab 25:620–627. https://doi.org/10.1016/j.tem.2014.08.005
Yun CW, Lee SH (2018) The roles of autophagy in cancer. Int J Mol Sci 19:3466. https://doi.org/10.3390/ijms19113466
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68:394–424. https://doi.org/10.3322/caac.21492
Raihan R, Azzeri A, Shabaruddin FH, Mohamed R (2018) Hepatocellular carcinoma in Malaysia and its changing trend. Euroasian J Hepatogastroenterol 8:54–56. https://doi.org/10.5005/jp-journals-10018-1259
Montella M, Crispo A, Giudice A (2011) HCC, diet, and metabolic factors. Hepat Mon 11:159–162
Bartosch B (2010) Hepatitis B and C viruses and hepatocellular carcinoma. Viruses 2:1504–1509. https://doi.org/10.3390/v2081504
Chisari FV, Isogawa M, Wieland SF (2010) Pathogenesis of hepatitis B virus infection. Parodontol 58:258–266. https://doi.org/10.1016/j.patbio.2009.11.001
Irshad M, Mankotia DS, Irshad K (2013) An insight into the diagnosis and pathogenesis of hepatitis C virus infection. World J Gastroenterol 19:7896–7909. https://doi.org/10.3748/wjg.v19.i44.7896
El-Serag HB, Rudolph KL (2007) Hepatocellular carcinoma: Epidemiology and molecular carcinogenesis. Gastroenterology 132:2557–2576. https://doi.org/10.1053/j.gastro.2007.04.061
Heidelbaugh JJ, Bruderly M (2006) Cirrhosis and chronic liver failure: Part I. Diagnosis and evaluation. Am Fam Physician 74:756–762
Sengupta S, Parikh ND (2017) Biomarker development for hepatocellular carcinoma early detection: current and future perspectives. Hepatic Oncol 4:111–122. https://doi.org/10.2217/hep-2017-0019
Llovet JM, Zucman-Rossi J, Pikarsky E, Sangro B, Schwartz M, Sherman M, Gores G (2016) Hepatocellular carcinoma. Nat Rev Dis Prim 2:16018. https://doi.org/10.1038/nrdp.2016.18
Llovet JM, Fuster BJ (2004) The Barcelona approach: diagnosis, staging, and treatment of hepatocellular carcinoma. Liver Transplant 10:S115-120. https://doi.org/10.1002/lt.20034
Santopaolo F, Lenci I, Milana M, Manzia TM, Baiocchi L (2019) Liver transplantation for hepatocellular carcinoma: Where do we stand? World J Gastroenterol 25:2591–2602. https://doi.org/10.3748/wjg.v25.i21.2591
Di Fazio P, Matrood S (2018) Targeting autophagy in liver cancer. Transl Gastroenterol Hepatol 3:39. https://doi.org/https://doi.org/10.21037/tgh.2018.06.09
White E, Karp C, Strohecker AM, Guo Y, Mathew R (2010) Role of autophagy in suppression of inflammation and cancer. Curr Opin Cell Biol 22:212–217. https://doi.org/10.1016/j.ceb.2009.12.008
Akkoç Y, Gözüaçık D (2018) Autophagy and liver cancer. Turkish J Gastroenterol 29:270–282. https://doi.org/10.5152/tjg.2018.150318
Sheng J, Qin H, Zhang K, Li B, Zhang X (2018) Targeting autophagy in chemotherapy-resistant of hepatocellular carcinoma. Am J Cancer Res 8:354–365
Huang F, Wang BR, Wang YG (2018) Role of autophagy in tumorigenesis, metastasis, targeted therapy and drug resistance of hepatocellular carcinoma. World J Gastroenterol 24:4643–4651. https://doi.org/10.3748/wjg.v24.i41.4643
Ayob AZ, Ramasamy TS (2018) Cancer stem cells as key drivers of tumour progression. J Biomed Sci 25:20. https://doi.org/10.1186/s12929-018-0426-4
Desai A, Yan Y, Gerson SL (2019) Concise reviews: cancer stem cell targeted therapies: toward clinical success. Stem Cells Transl Med 8:75–81. https://doi.org/10.1002/sctm.18-0123
Ji J, Wang XW (2012) Clinical implications of cancer stem cell biology in hepatocellular carcinoma. Semin Oncol 39:461–472. https://doi.org/10.1053/j.seminoncol.2012.05.011
Wang N, Wang S, Li MY, Hu BG, Liu LP, Yang SL, Yang S, Gong Z, Lai PBS, Chen GG (2018) Cancer stem cells in hepatocellular carcinoma: An overview and promising therapeutic strategies. Ther Adv Med Oncol 10:1758835918816287. https://doi.org/10.1177/1758835918816287
Visvader JE, Lindeman GJ (2012) Cancer stem cells: current status and evolving complexities. Cell Stem Cell 10:717–728. https://doi.org/10.1016/j.stem.2012.05.007
Wang K, Sun D (2018) Cancer stem cells of hepatocellular carcinoma. Prim Liver Cancer Challenges Perspect 9:23306–23314
Zhang H (2020) CCND1 silencing suppresses liver cancer stem cell differentiation through inhibiting autophagy. Hum Cell 33:140–147. https://doi.org/10.1007/s13577-019-00295-9
Deter RL, De Duve C (1967) Influence of glucagon, an inducer of cellular autophagy, on some physical properties of rat liver lysosomes. J Cell Biol 33:437–449. https://doi.org/10.1083/jcb.33.2.437
De Duve C, Wattiaux R (1966) FUNCTIONS OF LYSOSOMES. Annu Rev Physiol 28:435–492. https://doi.org/10.1146/annurev.ph.28.030166.002251
Ohsumi Y (2014) Historical landmarks of autophagy research. Cell Res 24:9–23. https://doi.org/10.1038/cr.2013.169
Das G, Shravage BV, Baehrecke EH (2012) Regulation and function of autophagy during cell survival and cell death. Cold Spring Harb Perspect Biol 4:1–14. https://doi.org/10.1101/cshperspect.a008813
Filomeni G, De Zio D, Cecconi F (2015) Oxidative stress and autophagy: the clash between damage and metabolic needs. Cell Death Differ 22:377–388. https://doi.org/10.1038/cdd.2014.150
Backer JM (2008) The regulation and function of Class III PI3Ks: novel roles for Vps34. Biochem J 410:1–17. https://doi.org/10.1042/BJ20071427
Ganley IG, Lam DH, Wang J, Ding X, Chen S, Jiang X (2009) ULK1·ATG13·FIP200 complex mediates mTOR signaling and is essential for autophagy. J Biol Chem 284:12297–12305. https://doi.org/10.1074/jbc.M900573200
Shang L, Chen S, Du F, Li S, Zhao L, Wang X (2011) Nutrient starvation elicits an acute autophagic response mediated by Ulk1 dephosphorylation and its subsequent dissociation from AMPK. Proc Natl Acad Sci U S A 108:4788–4793. https://doi.org/10.1073/pnas.1100844108
Kroemer G, Mariño G, Levine B (2010) Autophagy and the integrated stress response. Mol Cell 40:280–293. https://doi.org/10.1016/j.molcel.2010.09.023
Yang Z, Klionsky DJ (2010) Mammalian autophagy: Core molecular machinery and signaling regulation. Curr Opin Cell Biol 22:124–131. https://doi.org/10.1016/j.ceb.2009.11.014
Axe EL, Walker SA, Manifava M, Chandra P, Roderick HL, Habermann A, Griffiths G, Ktistakis NT (2008) Autophagosome formation from membrane compartments enriched in phosphatidylinositol 3-phosphate and dynamically connected to the endoplasmic reticulum. J Cell Biol 182:685–701. https://doi.org/10.1083/jcb.200803137
Noda NN, Fujioka Y, Hanada T, Ohsumi Y, Inagaki F (2013) Structure of the Atg12-Atg5 conjugate reveals a platform for stimulating Atg8-PE conjugation. EMBO Rep 14:206–211. https://doi.org/10.1038/embor.2012.208
Walczak M, Martens S (2013) Dissecting the role of the Atg12-Atg5-Atg16 complex during autophagosome formation. Autophagy 9:424–425. https://doi.org/10.4161/auto.22931
Tanida I, Ueno T, Kominami E (2004) LC3 conjugation system in mammalian autophagy. Int J Biochem Cell Biol 36:2503–2518. https://doi.org/10.1016/j.biocel.2004.05.009
Müller AJ, Proikas-Cezanne T (2015) Function of human WIPI proteins in autophagosomal rejuvenation of endomembranes? FEBS Lett 589:1546–1551. https://doi.org/10.1016/j.febslet.2015.05.008
Feng Y, Klionsky DJ (2017) Autophagic membrane delivery through ATG9. Cell Res 27:161–162. https://doi.org/10.1038/cr.2017.4
Ying H, Yue BYJT (2016) Optineurin: the autophagy connection. Exp Eye Res 144:73–80. https://doi.org/10.1016/j.exer.2015.06.029
Viret C, Rozières A, Faure M (2018) Novel insights into NDP52 autophagy receptor functioning. Trends Cell Biol 28:255–257. https://doi.org/10.1016/j.tcb.2018.01.003
Zhang X, Wang Y (2018) GRASP55 facilitates autophagosome maturation under glucose deprivation. Mol Cell Oncol 5:e1494948. https://doi.org/10.1080/23723556.2018.1494948
Zhao YG, Zhang H (2019) Autophagosome maturation: an epic journey from the ER to lysosomes. J Cell Biol 218:757–770. https://doi.org/10.1083/jcb.201810099
Tong J, Yan X, Yu L (2010) The late stage of autophagy: cellular events and molecular regulation. Protein Cell 1:907–915. https://doi.org/10.1007/s13238-010-0121-z
Yu L, McPhee CK, Zheng L, Mardones GA, Rong Y, Peng J, Mi N, Zhao Y, Liu Z, Wan F, Hailey DW, Oorschot V, Klumperman J, Baehrecke EH, Lenardo MJ (2010) Autophagy termination and lysosome reformation regulated by mTOR. Nature 465:942–946. https://doi.org/10.1038/nature09076
Berg TO, Fengsrud M, Strømhaug PE, Berg T, Seglen PO (1998) Isolation and characterization of rat liver amphisomes: evidence for fusion of autophagosomes with both early and late endosomes. J Biol Chem 273:21883–21892. https://doi.org/10.1074/jbc.273.34.21883
Nakamura S, Yoshimori T (2017) New insights into autophagosome-lysosome fusion. J Cell Sci 130:1209–1216. https://doi.org/10.1242/jcs.196352
Mitra V, Metcalf J (2012) Metabolic functions of the liver. Anaesth Intensive Care Med 13:54–55. https://doi.org/10.1016/j.mpaic.2011.11.006
Lavallard VJ, Gual P (2014) Autophagy and non-alcoholic fatty liver disease. Biomed Res Int 2014:120179. https://doi.org/10.1155/2014/120179
Madrigal-Matute J, Cuervo AM (2016) Regulation of liver metabolism by autophagy. Gastroenterology 150:328–339. https://doi.org/10.1053/j.gastro.2015.09.042
Ezaki J, Matsumoto N, Takeda-Ezaki M, Komatsu M, Takahashi K, Hiraoka Y, Taka H, Fujimura T, Takehana K, Yoshida M, Iwata J, Tanida I, Furuya N, Zheng DM, Tada N, Tanaka K, Kominami E, Ueno T (2011) Liver autophagy contributes to the maintenance of blood glucose and amino acid levels. Autophagy 7:727–736. https://doi.org/10.4161/auto.7.7.15371
Singh R, Kaushik S, Wang Y, Xiang Y, Novak I, Komatsu M, Tanaka K, Cuervo AM, Czaja MJ (2009) Autophagy regulates lipid metabolism. Nature 458:1131–1135. https://doi.org/10.1038/nature07976
Akman HO, Raghavan A, Craigen WJ (2011) Animal models of glycogen storage disorders. Prog Mol Biol Transl Sci 100:369–388. https://doi.org/10.1016/B978-0-12-384878-9.00009-1
Ke PY (2019) Diverse functions of autophagy in liver physiology and liver diseases. Int J Mol Sci 20:300. https://doi.org/10.3390/ijms20020300
Afifiyan N, Tillman B, French BA, Sweeny O, Masouminia M, Samadzadeh S, French SW (2017) The role of Tec kinase signaling pathways in the development of Mallory Denk bodies in balloon cells in alcoholic hepatitis. Exp Mol Pathol 103:191–199. https://doi.org/10.1016/j.yexmp.2017.09.001
Ni HM, Woolbright BL, Williams J, Copple B, Cui W, Luyendyk JP, Jaeschke H, Ding WX (2014) Nrf2 promotes the development of fibrosis and tumorigenesis in mice with defective hepatic autophagy. J Hepatol 61:617–625. https://doi.org/10.1016/j.jhep.2014.04.043
Galluzzi L, Pietrocola F, Bravo‐San Pedro JM, Amaravadi RK, Baehrecke EH, Cecconi F, Codogno P, Debnath J, Gewirtz DA, Karantza V, Kimmelman A, Kumar S, Levine B, Maiuri MC, Martin SJ, Penninger J, Piacentini M, Rubinsztein DC, Simon HU, Simonsen A, Thorburn AM, Velasco G, Ryan KM, Kroemer G (2015) Autophagy in malignant transformation and cancer progression. EMBO J 34: 856-880. https://doi.org/https://doi.org/10.15252/embj.201490784
Fu Y, Chung FL (2018) Oxidative stress and hepatocarcinogenesis. Hepatoma Res 4:39. https://doi.org/https://doi.org/10.20517/2394-5079.2018.29
Ciccarone F, Castelli S, Ciriolo MR (2019) Oxidative stress-driven autophagy across onset and therapeutic outcome in hepatocellular carcinoma. Oxid Med Cell Longev 2019:6050123. https://doi.org/10.1155/2019/6050123
Jin SM, Youle RJ (2012) PINK1-and Parkin-mediated mitophagy at a glance. J Cell Sci 125:795–799. https://doi.org/10.1242/jcs.093849
Zhang T, Xue L, Li L, Tang C, Wan Z, Wang R, Tan J, Tan Y, Han H, Tian R, Billiar TR, Tao WA, Zhang Z (2016) BNIP3 protein suppresses PINK1 kinase proteolytic cleavage to promote mitophagy. J Biol Chem 291:21616–21629. https://doi.org/10.1074/jbc.M116.733410
Fujiwara M, Marusawa H, Wang HQ, Iwai A, Ikeuchi K, Imai Y, Kataoka A, Nukina N, Takahashi R, Chiba T (2008) Parkin as a tumor suppressor gene for hepatocellular carcinoma. Oncogene 27:6002–6011. https://doi.org/10.1038/onc.2008.199
Takamura A, Komatsu M, Hara T, Sakamoto A, Kishi C, Waguri S, Eishi Y, Hino O, Tanaka K, Mizushima N (2011) Autophagy-deficient mice develop multiple liver tumors. Genes Dev 25:795–800. https://doi.org/10.1101/gad.2016211
Mathew R, Karp CM, Beaudoin B, Vuong N, Chen G, Chen HY, Bray K, Reddy A, Bhanot G, Gelinas C, DiPaola RS, Karantza-Wadsworth V, White E (2009) Autophagy suppresses tumorigenesis through elimination of p62. Cell 137:1062–1075. https://doi.org/10.1016/j.cell.2009.03.048
Inami Y, Waguri S, Sakamoto A, Kouno T, Nakada K, Hino O, Watanabe S, Ando J, Iwadate M, Yamamoto M, Lee MS, Tanaka K, Komatsu M (2011) Persistent activation of Nrf2 through p62 in hepatocellular carcinoma cells. J Cell Biol 193:275–284. https://doi.org/10.1083/jcb.201102031
Jaramillo MC, Zhang DD (2013) The emerging role of the Nrf2-Keap1 signaling pathway in cancer. Genes Dev 27:2179–2191. https://doi.org/10.1101/gad.225680.113
Yazdani H, Huang H, Tsung A (2019) Autophagy: Dual response in the development of hepatocellular carcinoma. Cells 8:91. https://doi.org/10.3390/cells8020091
Chen C, Lou T (2017) Hypoxia inducible factors in hepatocellular carcinoma. Oncotarget 8:46691–46703. https://doi.org/https://doi.org/10.18632/oncotarget.17358
Bellot G, Garcia-Medina R, Gounon P, Chiche J, Roux D, Pouysségur J, Mazure NM (2009) Hypoxia-induced autophagy is mediated through hypoxia-inducible factor induction of BNIP3 and BNIP3L via their BH3 domains. Mol Cell Biol 29:2570–2581. https://doi.org/10.1128/MCB.00166-09
Zhang J, Ney PA (2009) Role of BNIP3 and NIX in cell death, autophagy, and mitophagy. Cell Death Differ 16:939–946. https://doi.org/10.1038/cdd.2009.16
Decuypere JP, Parys JB, Bultynck G (2012) Regulation of the autophagic Bcl-2/Beclin 1 interaction. Cells 1:284–312. https://doi.org/10.3390/cells1030284
Sun L, Li T, Wei Q, Zhang Y, Jia X, Wan Z, Han L (2014) Upregulation of BNIP3 mediated by ERK/HIF-1α pathway induces autophagy and contributes to anoikis resistance of hepatocellular carcinoma cells. Future Oncol 10:1387–1398. https://doi.org/10.2217/fon.14.70
Keith B, Johnson RS, Simon MC (2011) HIF1α and HIF2α: Sibling rivalry in hypoxic tumor growth and progression. Nat Rev Cancer 12:9–22. https://doi.org/10.1038/nrc3183
Menrad H, Werno C, Schmid T, Copanaki E, Deller T, Dehne N, Brüne B (2010) Roles of hypoxia-inducible factor-1α (HIF-1α) versus HIF-2α in the survival of hepatocellular tumor spheroids. Hepatology 51:2183–2192. https://doi.org/10.1002/hep.23597
Mazure NM, Pouysségur J (2009) Atypical BH3-domains of BNIP3 and BNIP3L lead to autophagy in hypoxia. Autophagy 5:868–869. https://doi.org/10.4161/auto.9042
Leber B, Lin J, Andrews DW (2007) Embedded together: The life and death consequences of interaction of the Bcl-2 Family with membranes. Apoptosis 12:897–911. https://doi.org/10.1007/s10495-007-0746-4
Dong XF, Liu TQ, Zhi XT, Zou J, Zhong JT, Li T, Mo XL, Zhou W, Guo WW, Liu X, Chen YY, Li MY, Zhong XG, Han YM, Wang ZH, Dong ZR (2018) COX-2/PGE2 axis regulates HIF2a activity to promote hepatocellular carcinoma hypoxic response and reduce the sensitivity of sorafenib treatment. Clin Cancer Res 24:3204–3216. https://doi.org/10.1158/1078-0432.CCR-17-2725
Wu DH, Jia CC, Chen J, Lin ZX, Ruan DY, Li X, Lin Q, Min-Dong MXK, Wan XB, Cheng N, Chen ZH, Xing YF, Wu XY, Wen JY (2014) Autophagic LC3B overexpression correlates with malignant progression and predicts a poor prognosis in hepatocellular carcinoma. Tumour Biol 35:12225–12233. https://doi.org/10.1007/s13277-014-2531-7
Lazova R, Camp RL, Klump V, Siddiqui SF, Amaravadi RK, Pawelek JM (2012) Punctate LC3B expression is a common feature of solid tumors and associated with proliferation, metastasis and poor outcome. Clin Cancer Res 18:370–379. https://doi.org/10.1158/1078-0432.CCR-11-1282
Langley RR, Fidler IJ (2011) The seed and soil hypothesis revisited - the role of tumor-stroma interactions in metastasis to different organs. Int J Cancer 128:2527–2535. https://doi.org/10.1002/ijc.26031
Seyfried TN, Huysentruyt LC (2013) On the origin of cancer metastasis. Crit Rev Oncog 18:43–73. https://doi.org/10.1615/critrevoncog.v18.i1-2.40
Kim YN, Koo KH, Sung JY, Yun UJ, Kim H (2012) Anoikis resistance: an essential prerequisite for tumor metastasis. Int J Cell Biol 2012:306879. https://doi.org/10.1155/2012/306879
Paoli P, Giannoni E, Chiarugi P (2013) Anoikis molecular pathways and its role in cancer progression. Biochim Biophys Acta 1833:3481–3498. https://doi.org/10.1016/j.bbamcr.2013.06.026
Yang J, Zheng Z, Yan X, Li X, Liu Z, Ma Z (2013) Integration of autophagy and anoikis resistance in solid tumors. Anat Rec 296:1501–1508. https://doi.org/10.1002/ar.22769
Avivar-Valderas A, Salas E, Bobrovnikova-Marjon E, Diehl JA, Nagi C, Debnath J, Aguirre-Ghiso JA (2011) PERK integrates autophagy and oxidative stress responses to promote survival during extracellular matrix detachment. Mol Cell Biol 31:3616–3629. https://doi.org/10.1128/MCB.05164-11
Peng YF, Shi YH, Ding ZB, Ke AW, Gu CY, Hui B, Zhou J, Qiu SJ, Dai Z, Fan J (2013) Autophagy inhibition suppresses pulmonary metastasis of HCC in mice via impairing anoikis resistance and colonization of HCC cells. Autophagy 9:2056–2068. https://doi.org/10.4161/auto.26398
Kubiczkova L, Sedlarikova L, Hajek R, Sevcikova S (2012) TGF-β - an excellent servant but a bad master. J Transl Med 10:183. https://doi.org/10.1186/1479-5876-10-183
Scandura JM, Boccuni P, Massagué J, Nimer SD (2004) Transforming growth factor β-induced cell cycle arrest of human hematopoietic cells requires p57KIP2 up-regulation. Proc Natl Acad Sci U S A 101:15231–15236. https://doi.org/10.1073/pnas.0406771101
Inman GJ (2011) Switching TGFβ from a tumor suppressor to a tumor promoter. Curr Opin Genet Dev 21:93–99. https://doi.org/10.1016/j.gde.2010.12.004
Tong H, Yin H, Hossain MA, Wang Y, Wu F, Dong X, Gao S, Zhan K, He W (2019) Starvation-induced autophagy promotes the invasion and migration of human bladder cancer cells via TGF-β1/Smad3-mediated epithelial-mesenchymal transition activation. J Cell Biochem 120:5118–5127. https://doi.org/10.1002/jcb.27788
Li J, Yang B, Zhou Q, Wu Y, Shang D, Guo Y, Song Z, Zheng Q, Xiong J (2013) Autophagy promotes hepatocellular carcinoma cell invasion through activation of epithelial-mesenchymal transition. Carcinogenesis 34:1343–1351. https://doi.org/10.1093/carcin/bgt063
Roche J (2018) The epithelial-to-mesenchymal transition in cancer. Cancers (Basel) 10:52. https://doi.org/10.3390/cancers10020052
Wang J, Chen L, Li Y, Guan XY (2011) Overexpression of cathepsin Z contributes to tumor metastasis by inducing epithelial-mesenchymal transition in hepatocellular carcinoma. PLoS ONE 6:e24967. https://doi.org/10.1371/journal.pone.0024967
Chen HT, Liu H, Mao MJ, Tan Y, Mo XQ, Meng XJ, Cao MT, Zhong CY, Liu Y, Shan H, Jiang GM (2019) Crosstalk between autophagy and epithelial-mesenchymal transition and its application in cancer therapy. Mol Cancer 18:101. https://doi.org/10.1186/s12943-019-1030-2
Chen C, Liang QY, Chen HK, Wu PF, Feng ZY, Ma XM, Wu HR, Zhou GQ (2018) DRAM1 regulates the migration and invasion of hepatoblastoma cells via autophagy-EMT pathway. Oncol Lett 16:2427–2433. https://doi.org/10.3892/ol.2018.8937
Hu S, Wang L, Zhang X, Wu Y, Yang J, Li J (2018) Autophagy induces transforming growth factor-β-dependent epithelial-mesenchymal transition in hepatocarcinoma cells through cAMP response element binding signalling. J Cell Mol Med 22:5518–5532. https://doi.org/10.1111/jcmm.13825
Wang Y, Xiong H, Liu D, Hill C, Ertay A, Li J, Zou Y, Miller P, White E, Downward J, Goldin RD, Yuan X, Lu X (2019) Autophagy inhibition specifically promotes epithelial-mesenchymal transition and invasion in RAS-mutated cancer cells. Autophagy 15:886–899. https://doi.org/10.1080/15548627.2019.1569912
Zhao Z, Zhao J, Xue J, Zhao X, Liu P (2016) Autophagy inhibition promotes epithelial-mesenchymal transition through ROS/HO-1 pathway in ovarian cancer cells. Am J Cancer Res 6:2162–2177
Shaaban S, Negm A, Ibrahim EE, Elrazak AA (2014) Chemotherapeutic agents for the treatment of hepatocellular carcinoma: efficacy and mode of action. Oncol Rev 8:246. https://doi.org/10.4081/oncol.2014.246
Riddell IA, Lippard SJ (2018) Cisplatin and oxaliplatin: Our current understanding of their actions. In: Sigel A, Sigel H, Freisinger E, Sigel RKO (ed) Metallo-drugs: Development and action of anticancer agents, De Gruyter, Berlin Munich Boston, pp 1–42. https://doi.org/https://doi.org/10.1515/9783110470734-001
Chen R, Dai RY, Duan CY, Liu YP, Chen SK, Yan DM, Chen CN, Wei M, Li H (2011) Unfolded protein response suppresses cisplatin-induced apoptosis via autophagy regulation in human hepatocellular carcinoma cells. Folia Biol (Praha) 57:87–95
Du H, Yang W, Chen L, Shi M, Seewoo V, Wang J, Lin A, Liu Z, Qiu W (2012) Role of autophagy in resistance to oxaliplatin in hepatocellular carcinoma cells. Oncol Rep 27:143–150. https://doi.org/10.3892/or.2011.1464
Nitiss JL (2009) Targeting DNA topoisomerase II in cancer chemotherapy. Nat Rev Cancer 9:338–350. https://doi.org/10.1038/nrc2607
Zhou Y, Chen E, Tang Y, Mao J, Shen J, Zheng X, Xie S, Zhang S, Wu Y, Liu H, Zhi X, Ma T, Ni H, Chen J, Chai K, Chen W (2019) miR-223 overexpression inhibits doxorubicin-induced autophagy by targeting FOXO3a and reverses chemoresistance in hepatocellular carcinoma cells. Cell Death Dis 10:843. https://doi.org/10.1038/s41419-019-2053-8
Jin J, Huang M, Wei HL, Liu GT (2002) Mechanism of 5-fluorouracil required resistance in human hepatocellular carcinoma cell line Bel7402. World J Gastroenterol 8:1029–1034. https://doi.org/10.3748/wjg.v8.i6.1029
Guo XL, Hu F, Zhang SS, Zhao QD, Zong C, Ye F, Guo SW, Zhang JW, Li R, Wu MC, Wei LX (2014) Inhibition of p53 increases chemosensitivity to 5-FU in nutrient-deprived hepatocarcinoma cells by suppressing autophagy. Cancer Lett 346:278–284. https://doi.org/10.1016/j.canlet.2014.01.011
Llovet JM, Ricci S, Mazzaferro V, Hilgard P, Gane E, Blanc JF, de Oliveira AC, Santoro A, Raoul JL, Forner A, Schwartz M, Porta C, Zeuzem S, Bolondi L, Greten TF, Galle PR, Seitz JF, Borbath I, Häussinger D, Giannaris T, Shan M, Moscovici M, Voliotis D, Bruix J, SHARP Investigators Study Group (2008) Sorafenib in advanced hepatocellular carcinoma. N Engl J Med 359:378–390. https://doi.org/10.1056/NEJMoa0708857
Fu XT, Song K, Zhou J, Shi YH, Liu WR, Tian MX, Jin L, Shi GM, Gao Q, Ding ZB, Fan J (2018) Autophagy activation contributes to glutathione transferase Mu 1-mediated chemoresistance in hepatocellular carcinoma. Oncol Lett 16:346–352. https://doi.org/10.3892/ol.2018.8667
Zhai B, Hu F, Jiang X, Xu J, Zhao D, Liu B, Pan S, Dong X, Tan G, Wei Z, Qiao H, Jiang H, Sun X (2014) Inhibition of Akt reverses the acquired resistance to sorafenib by switching protective autophagy to autophagic cell death in hepatocellular carcinoma. Mol Cancer Ther 13:1589–1598. https://doi.org/10.1158/1535-7163.MCT-13-1043
Zhao D, Zhai B, He C, Tan G, Jiang X, Pan S, Dong X, Wei Z, Ma L, Qiao H, Jiang H, Sun X (2014) Upregulation of HIF-2α induced by sorafenib contributes to the resistance by activating the TGF-α/EGFR pathway in hepatocellular carcinoma cells. Cell Signal 26:1030–1039. https://doi.org/10.1016/j.cellsig.2014.01.026
Liang Y, Zheng T, Song R, Wang J, Yin D, Wang L, Liu H, Tian L, Fang X, Meng X, Jiang H, Liu J, Liu L (2013) Hypoxia-mediated sorafenib resistance can be overcome by EF24 through Von Hippel-Lindau tumor suppressor-dependent HIF-1α inhibition in hepatocellular carcinoma. Hepatology 57:1847–1857. https://doi.org/10.1002/hep.26224
Tang W, Chen Z, Zhang W, Cheng Y, Zhang B, Wu F, Wang Q, Wang S, Rong D, Reiter FP, De Toni EN, Wang X (2020) The mechanisms of sorafenib resistance in hepatocellular carcinoma: theoretical basis and therapeutic aspects. Signal Transduct Target Ther 5:87. https://doi.org/10.1038/s41392-020-0187-x
Peng WX, Xiong EM, Ge L, Wan YY, Zhang CL, Du FY, Xu M, Bhat RA, Jin J, Gong AH (2016) Egr-1 promotes hypoxia-induced autophagy to enhance chemo-resistance of hepatocellular carcinoma cells. Exp Cell Res 340:62–70. https://doi.org/10.1016/j.yexcr.2015.12.006
Xu Y, An Y, Wang Y, Zhang C, Zhang H, Huang C, Jiang H, Wang X, Li X (2013) miR-101 inhibits autophagy and enhances cisplatin-induced apoptosis in hepatocellular carcinoma cells. Oncol Rep 29:2019–2024. https://doi.org/10.3892/or.2013.2338
Lanza E, Donadon M, Poretti D, Pedicini V, Tramarin M, Roncalli M, Rhee H, Park YN, Torzilli G (2017) Transarterial therapies for hepatocellular carcinoma. Liver Cancer 6:27–33. https://doi.org/10.1159/000449347
Pleguezuelo M, Marelli L, Misseri M, Germani G, Calvaruso V, Xiruochakis E, Manousou P, Burroughs AK (2008) TACE versus TAE as therapy for hepatocellular carcinoma. Expert Rev Anticancer Ther 8:1623–1641. https://doi.org/10.1586/14737140.8.10.1623
Rammohan A, Sathyanesan J, Ramaswami S, Lakshmanan A, Senthil-Kumar P, Srinivasan UP, Ramasamy R, Ravichandran P (2012) Embolization of liver tumors: past, present and future. World J Radiol 4:405–412. https://doi.org/10.4329/wjr.v4.i9.405
Gade TPF, Tucker E, Nakazawa MS, Hunt SJ, Wong W, Krock B, Weber CN, Nadolski GJ, Clark TWI, Soulen MC, Furth EE, Winkler JD, Amaravadi RK, Simon MC (2017) Ischemia induces quiescence and autophagy dependence in hepatocellular carcinoma. Radiology 283:702–710. https://doi.org/10.1148/radiol.2017160728
Tao W, Shi JF, Zhang Q, Xue B, Sun YJ, Li CJ (2013) Egr-1 enhances drug resistance of breast cancer by modulating MDR1 expression in a GGPPS-independent manner. Biomed Pharmacother 67:197–202. https://doi.org/10.1016/j.biopha.2013.01.001
Peng WX, Wan YY, Gong AH, Ge L, Jin J, Xu M, Wu CY (2017) Egr-1 regulates irradiation-induced autophagy through Atg4B to promote radioresistance in hepatocellular carcinoma cells. Oncogenesis 6:e292. https://doi.org/10.1038/oncsis.2016.91
Yang Z, Wilkie-Grantham RP, Yanagi T, Shu CW, Matsuzawa SI, Reed JC (2015) ATG4B (Autophagin-1) phosphorylation modulates autophagy. J Biol Chem 290:26549–26561. https://doi.org/10.1074/jbc.M115.658088
Wang Z, Han W, Sui X, Fang Y, Pan H (2014) Autophagy: a novel therapeutic target for hepatocarcinoma (Review). Oncol Lett 7:1345–1351. https://doi.org/10.3892/ol.2014.1916
Sun T, Liu H, Ming L (2017) Multiple roles of autophagy in the sorafenib resistance of hepatocellular carcinoma. Cell Physiol Biochem 44:716–727. https://doi.org/10.1159/000485285
Shi YH, Ding ZB, Zhou J, Hui B, Shi GM, Ke AW, Wang XY, Dai Z, Peng YF, Gu CY, Qiu SJ, Fan J (2011) Targeting autophagy enhances sorafenib lethality for hepatocellular carcinoma via ER stress-related apoptosis. Autophagy 7:1159–1172. https://doi.org/10.4161/auto.7.10.16818
Prieto-Vila M, Takahashi RU, Usuba W, Kohama I, Ochiya T (2017) Drug resistance driven by cancer stem cells and their niche. Int J Mol Sci 18:2574. https://doi.org/10.3390/ijms18122574
Nio K, Yamashita T, Kaneko S (2017) The evolving concept of liver cancer stem cells. Mol Cancer 16:4. https://doi.org/10.1186/s12943-016-0572-9
Yamashita T, Wang XW (2013) Cancer stem cells in the development of liver cancer. J Clin Invest 123:1911–1918. https://doi.org/10.1172/JCI66024
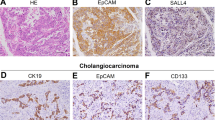
Yamashita T, Ji J, Budhu A, Forgues M, Yang W, Wang HY, Jia H, Ye Q, Qin LX, Wauthier E, Reid LM, Minato H, Honda M, Kaneko S, Tang ZY, Wang XW (2009) EpCAM-positive hepatocellular carcinoma cells are tumor initiating cells with stem/progenitor cell features. Gastroenterology 136:1012–1024. https://doi.org/10.1053/j.gastro.2008.12.004
Terris B, Cavard C, Perret C (2010) EpCAM, a new marker for cancer stem cells in hepatocellular carcinoma. J Hepatol 52:280–281. https://doi.org/10.1016/j.jhep.2009.10.026
Ma S, Chan KW, Hu L, Lee TKW, Wo JYH, Ng IOL, Zheng BJ, Guan XY (2007) Identification and characterization of tumorigenic liver cancer stem/progenitor cells. Gastroenterology 132:2542–2556. https://doi.org/10.1053/j.gastro.2007.04.025
Zhu Z, Hao X, Yan M, Yao M, Ge C, Gu J, Li J (2010) Cancer stem/progenitor cells are highly enriched in CD133 +CD44+ population in hepatocellular carcinoma. Int J Cancer 126:2067–2078. https://doi.org/10.1002/ijc.24868
Yang FZ, Ngai P, Ho DW, Yu WC, Ng MNP, Lau CK, Li MLY, Tam KH, Lam CT, Poon RTP, Fan ST (2008) Identification of local and circulating cancer stem cells in human liver cancer. Hepatology 47:919–928. https://doi.org/10.1002/hep.22082
Haraguchi N, Ishii H, Mimori K, Tanaka F, Ohkuma M, Kim HM, Akita H, Takiuchi D, Hatano H, Nagano H, Barnard GF, Doki Y, Mori M (2010) CD13 is a therapeutic target in human liver cancer stem cells. J Clin Invest 120:3326–3339. https://doi.org/10.1172/JCI42550
Qiu L, Li H, Fu S, Chen X, Lu L (2018) Surface markers of liver cancer stem cells and innovative targeted-therapy strategies for HCC. Oncol lett 15:2039–2048. https://doi.org/10.3892/ol.2017.7568
Govaere O, Komuta M, Berkers J, Spee B, Janssen C, de Luca F, Katoonizadeh A, Wouters J, van Kempen LC, Durnez A, Verslype C, De Kock J, Rogiers V, van Grunsven LA, Topal B, Pirenne J, Vankelecom H, Nevens F, van den Oord J, Pinzani M, Roskams T (2014) Keratin 19: a key role player in the invasion of human hepatocellular carcinomas. Gut 63:674–685. https://doi.org/10.1136/gutjnl-2012-304351
Zheng H, Pomyen Y, Hernandez MO, Li C, Livak F, Tang W, Dang H, Greten TF, Davis JL, Zhao Y, Mehta M, Levin Y, Shetty J, Tran B, Budhu A, Wang XW (2018) Single cell analysis reveals cancer stem cell heterogeneity in hepatocellular carcinoma. Hepatalogy 68:127–140. https://doi.org/10.1002/hep.29778
Magee JA, Piskounova E, Morrison SJ (2012) Cancer stem cells: Impact, heterogeneity, and uncertainty. Cancer Cell 21:283–296. https://doi.org/10.1016/j.ccr.2012.03.003
Reya T, Clevers H (2005) Wnt signalling in stem cells and cancer. Nature 434:843–850. https://doi.org/10.1038/nature03319
Weinmaster G, Kopan R (2016) A garden of Notch-ly delights. Development 133:3277–3282. https://doi.org/10.1242/dev.02515
Gotoh N (2009) Control of stemness by fibroblast growth factor signaling in stem cells and cancer stem cells. Curr Stem Cell Res Ther 4:9–15. https://doi.org/10.2174/157488809787169048
Derynck R, Zhang YE (2003) Smad-dependent and Smad-independent pathways in TGF-β family signalling. Nature 425:577–584. https://doi.org/10.1038/nature02006
Sell S (2010) On the stem cell origin of cancer. Am J Pathol 176:2584–2594. https://doi.org/10.2353/ajpath.2010.091064
Lau EYT, Ho NPY, Lee TKW (2017) Cancer stem cells and their microenvironment: biology and therapeutic implications. Stem Cells Int 2017:3714190. https://doi.org/10.1155/2017/3714190
Gao Y, Ruan B, Liu W, Wang J, Yang X, Zhang Z, Li X, Duan J, Zhang F, Ding R, Tao K, Dou K (2015) Knockdown of CD44 inhibits the invasion and metastasis of hepatocellular carcinoma both in vitro and in vivo by reversing epithelial-mesenchymal transition. Oncotarget 6:7828–7837. https://doi.org/10.18632/oncotarget.3488
van Zijl F, Zulehner G, Petz M, Schneller D, Kornauth C, Hau M, Machat G, Grubinger M, Huber H, Mikulits W (2009) Epithelial-mesenchymal transition in hepatocellular carcinoma. Futur Oncol 5:1169–1179. https://doi.org/10.2217/fon.09.91
Cazet AS, Hui MN, Elsworth BL, Wu SZ, Roden D, Chan CL, Skhinas JN, Collot R, Yang J, Harvey K, Johan MZ, Cooper C, Nair R, Herrmann D, McFarland A, Deng N, Ruiz-Borrego M, Rojo F, Trigo JM, Bezares S, Caballero R, Lim E, Timpson P, O’Toole S, Watkins DN, Cox TR, Samuel MS, Martín M, Swarbrick A (2018) Targeting stromal remodeling and cancer stem cell plasticity overcomes chemoresistance in triple negative breast cancer. Nat Commun 9:2897. https://doi.org/10.1038/s41467-018-05220-6
Dai XM, Yang SL, Zheng XM, Chen GG, Chen J, Zhang T (2018) CD133 expression and α-fetoprotein levels define novel prognostic subtypes of HBV-associated hepatocellular carcinoma: A long-term follow-up analysis. Oncol Lett 15:2985–2991. https://doi.org/10.3892/ol.2017.7704
Yamanaka C, Wada H, Eguchi H, Hatano H, Gotoh K, Noda T, Yamada D, Asaoka T, Kawamoto K, Nagano H, Doki Y, Mori M (2018) Clinical significance of CD13 and epithelial mesenchymal transition (EMT) markers in hepatocellular carcinoma. Jpn J Clin Oncol 48:52–60. https://doi.org/10.1093/jjco/hyx157
Batlle E, Clevers H (2017) Cancer stem cells revisited. Nat Med 23:1124–1134. https://doi.org/10.1038/nm.4409
Trédan O, Galmarini CM, Patel K, Tannock IF (2007) Drug resistance and the solid tumor microenvironment. J Natl Cancer Inst 99:1441–1454. https://doi.org/10.1093/jnci/djm135
Baumann M, Krause M, Hill R (2008) Exploring the role of cancer stem cells in radioresistance. Nat Rev Cancer 8:545–554. https://doi.org/10.1038/nrc2419
Bai X, Ni J, Beretov J, Graham P, Li Y (2018) Cancer stem cell in breast cancer therapeutic resistance. Cancer Treat Rev 69:152–163. https://doi.org/10.1016/j.ctrv.2018.07.004
Sun YL, Patel A, Kumar P, Chen ZS (2012) Role of ABC transporters in cancer chemotherapy. Chin J Cancer 31:51–57. https://doi.org/10.5732/cjc.011.10466
Zhang G, Wang Z, Luo W, Jiao H, Wu J, Jiang C (2013) Expression of potential cancer stem cell marker ABCG2 is associated with malignant behaviors of hepatocellular carcinoma. Gastroenterol Res Pract 2013:782581. https://doi.org/10.1155/2013/782581
Jia Q, Zhang X, Deng T, Gao J (2013) Positive correlation of Oct4 and ABCG2 to chemotherapeutic resistance in CD90+CD133+ liver cancer stem cells. Cell Reprogram 15:143–150. https://doi.org/10.1089/cell.2012.0048
Ranji P, T. Salmani Kesejini T, Saeedikhoo S, Alizadeh AM, (2016) Targeting cancer stem cell-specific markers and/or associated signaling pathways for overcoming cancer drug resistance. Tumor Biol 37:13059–13075. https://doi.org/10.1007/s13277-016-5294-5
Vassalli G (2019) Aldehyde dehydrogenases: Not just markers, but functional regulators of stem cells. Stem Cells Int 2019:3904645. https://doi.org/10.1155/2019/3904645
Carnero A, Garcia-Mayea Y, Mir C, Lorente J, RubioLLeonart ITME (2016) The cancer stem-cell signaling network and resistance to therapy. Cancer Treat Rev 49:25–36. https://doi.org/10.1016/j.ctrv.2016.07.001
Tsai LL, Yu CC, Lo JF, Sung WW, Lee H, Chen SL, Chou MY (2012) Enhanced cisplatin resistance in oral-cancer stem-like cells is correlated with upregulation of excision-repair cross-complementation group 1. J Dent Sci 7:111–117. https://doi.org/10.1016/j.jds.2012.03.006
Kim NH, Kim HS, Li XY, Lee I, Choi HS, Kang SE, Cha SY, Ryu JK, Yoon D, Fearon ER, Rowe RG, Lee S, Maher CA, Weiss SJ, Yook JI (2011) A p53/miRNA-34 axis regulates Snail1-dependent cancer cell epithelial-mesenchymal transition. J Cell Biol 195:417–433. https://doi.org/10.1083/jcb.201103097
Carafa V, Rotili D, Forgione M, Cuomo F, Serretiello E, Hailu GS, Jarho E, Lahtela-Kakkonen M, Mai A, Altucci L (2016) Sirtuin functions and modulation: from chemistry to the clinic. Clin Epigenetics 8:61. https://doi.org/10.1186/s13148-016-0224-3
Michan S, Sinclair D (2007) Sirtuins in mammals: Insights into their biological function. Biochem J 404:1–13. https://doi.org/10.1042/BJ20070140
Ong ALC, Ramasamy TS (2018) Role of Sirtuin1-p53 regulatory axis in aging, cancer and cellular reprogramming. Ageing Res Rev 43:64–80. https://doi.org/10.1016/j.arr.2018.02.004
O’Callaghan C, Vassilopoulos A (2017) Sirtuins at the crossroads of stemness, aging, and cancer. Aging Cell 16:1208–1218. https://doi.org/10.1111/acel.12685
Liu T, Liu PY, Marshall GM (2009) The critical role of the class III histone deacetylase SIRT1 in cancer. Cancer Res 69:1702–1705. https://doi.org/10.1158/0008-5472.CAN-08-3365
Wang RH, Sengupta K, Li C, Kim HS, Cao L, Xiao C, Kim S, Xu X, Zheng Y, Chilton B, Jia R, Zheng ZM, Appella E, Wang XW, Reid T, Deng CX (2008) Impaired DNA damage response, genome instability, and tumorigenesis in SIRT1 mutant mice. Cancer Cell 14:312–323. https://doi.org/10.1016/j.ccr.2008.09.001
Farcas M, Gavrea AA, Gulei D, Ionescu C, Irimie A, Catana CS, Berindan-Neagoe I (2019) SIRT1 in the development and treatment of hepatocellular carcinoma. Front Nutr 6:148. https://doi.org/10.3389/fnut.2019.00148
Chen X, Huan H, Liu C, Luo Y, Shen J, Zhuo Y, Zhang Z, Qian C (2019) Deacetylation of β-catenin by SIRT1 regulates self-renewal and oncogenesis of liver cancer stem cells. Cancer Lett 463:1–10. https://doi.org/10.1016/j.canlet.2019.07.021
Kopan R (2012) Notch signaling. Cold Spring Harb Perspect Biol 4:a011213. https://doi.org/10.1101/cshperspect.a011213
Qi R, An H, Yu Y, Zhang M, Liu S, Xu H, Guo Z, Cheng T, Cao X (2003) Notch1 signaling inhibits growth of human hepatocellular carcinoma through induction of cell cycle arrest and apoptosis. Cancer Res 63:8323–8329
Ning L, Wentworth L, Chen H, Weber SM (2009) Down-regulation of Notch1 signaling inhibits tumor growth in human hepatocellular carcinoma. Am J Transl Res 1:358–366
Liu L, Liu C, Zhang Q, Shen J, Zhang H, Shan J, Duan G, Guo D, Chen X, Cheng J, Xu Y, Yang Z, Yao C, Lai M, Qian C (2016) SIRT1-mediated transcriptional regulation of SOX2 is important for self-renewal of liver cancer stem cells. Hepatology 64:814–827. https://doi.org/10.1002/hep.28690
Zhang S, Xiong X, Sun Y (2020) Functional characterization of SOX2 as an anticancer target. Sig Transduct Target Ther 5:135. https://doi.org/10.1038/s41392-020-00242-3
Kim HJ, Maiti P, Barrientos A (2017) Mitochondrial ribosomes in cancer. Semin Cancer Biol 47:67–81. https://doi.org/10.1016/j.semcancer.2017.04.004
Cheng J, Liu C, Liu L, Chen X, Shan J, Shen J, Zhu W, Qian C (2016) MEK1 signaling promotes self-renewal and tumorigenicity of liver cancer stem cells via maintaining SIRT1 protein stabilization. Oncotarget 7:20597–20611. https://doi.org/10.18632/oncotarget.7972
Pearson G, Robinson F, Gibson TB, Xu BE, Karandikar M, Berman K, Cobb MH (2001) Mitogen-activated protein (MAP) kinase pathways: Regulation and physiological functions. Endocr Rev 22:153–183. https://doi.org/10.1210/edrv.22.2.0428
Mortensen M, Simon AK (2010) Nonredundant role of Atg7 in mitochondrial clearance during erythroid development. Autophagy 6:423–425. https://doi.org/10.4161/auto.6.3.11528
Miyajima A, Tanaka M, Itoh T (2014) Stem/progenitor cells in liver development, homeostasis, regeneration, and reprogramming. Cell Stem Cell 14:561–574. https://doi.org/10.1016/j.stem.2014.04.010
Cheng Y, Wang B, Zhou H, Dang S, Jin M, Shi Y, Hao L, Yang Z, Zhang Y (2015) Autophagy is required for the maintenance of liver progenitor cell functionality. Cell Physiol Biochem 36:1163–1174. https://doi.org/10.1159/000430287
Xue F, Hu L, Ge R, Yang L, Liu K, Li Y, Sun Y, Wang K (2016) Autophagy-deficiency in hepatic progenitor cells leads to the defects of stemness and enhances susceptibility to neoplastic transformation. Cancer Lett 371:38–47. https://doi.org/10.1016/j.canlet.2015.11.022
Bu Y, Cao D (2012) The origin of cancer stem cells. Front Biosci (Schol Ed) 4:819–830. https://doi.org/10.2741/s302
Zender L, Spector MS, Xue W, Flemming P, Cordon-Cardo C, Silke J, Fan ST, Luk JM, Wigler M, Hannon GJ, Mu D, Lucito R, Powers S, Lowe SW (2006) Identification and validation of oncogenes in liver cancer using an integrative oncogenomic approach. Cell 125:1253–1267. https://doi.org/10.1016/j.cell.2006.05.030
Tang Y, Kitisin K, Jogunoori W, Li C, Deng CX, Mueller SC, Ressom HW, Rashid A, He AR, Mendelson JS, Jessup JM, Shetty K, Zasloff M, Mishra B, Reddy EP, Johnson L, Mishra L (2008) Progenitor/stem cells give rise to liver cancer due to aberrant TGF-beta and IL-6 signaling. Proc Natl Acad Sci U S A 105:2445–2450. https://doi.org/10.1073/pnas.0705395105
Liu K, Lee J, Kim JY, Wang L, Tian Y, Chan ST, Cho C, Machida K, Chen D, Ou JHJ (2017) Mitophagy controls the activities of tumor suppressor p53 to regulate hepatic cancer stem cells. Mol Cell 68:281-292.e5. https://doi.org/10.1016/j.molcel.2017.09.022
Li J, Hu SB, Wang LY, Zhang X, Zhou X, Yang B, Li JH, Xiong J, Liu N, Li Y, Wu YZ, Zheng QC (2017) Autophagy-dependent generation of Axin2+ cancer stem-like cells promotes hepatocarcinogenesis in liver cirrhosis. Oncogene 36:6725–6737. https://doi.org/10.1038/onc.2017.272
Song YJ, Zhang SS, Guo XL, Sun K, Han ZP, Li R, Zhao QD, Deng WJ, Xie XQ, Zhang JW, Wu MC, Wei LX (2013) Autophagy contributes to the survival of CD133+ liver cancer stem cells in the hypoxic and nutrient-deprived tumor microenvironment. Cancer Lett 339:70–81. https://doi.org/10.1016/j.canlet.2013.07.021
Li Z, Jiao X, Di Sante G, Ertel A, Casimiro MC, Wang M, Katiyar S, Ju X, Klopfenstein DV, Tozeren A, Dampier W, Chepelev I, Jeltsch A, Pestell RG (2019) Cyclin D1 integrates G9a-mediated histone methylation. Oncogene 38:4232–4249. https://doi.org/10.1038/s41388-019-0723-8
Zheng N, Wei W, Wang Z (2016) Emerging roles of FGF signaling in hepatocellular carcinoma. Transl Cancer Res 5:1–6
Ocker M (2020) Fibroblast growth factor signaling in non-alcoholic fatty liver disease and non-alcoholic steatohepatitis: paving the way to hepatocellular carcinoma. World J Gastroenterol 26:279–290. https://doi.org/10.3748/wjg.v26.i3.279
Gauglhofer C, Sagmeister S, Schrottmaier W, Fischer C, Rodgarkia-Dara C, Mohr T, Stättner S, Bichler C, Kandioler D, Wrba F, Schulte-Hermann R, Holzmann K, Grusch M, Marian B, Berger W, Grasl-Kraupp B (2011) Up-regulation of the fibroblast growth factor 8 subfamily in human hepatocellular carcinoma for cell survival and neoangiogenesis. Hepatology 53:854–864. https://doi.org/10.1002/hep.24099
Sawey ET, Chanrion M, Cai C, Wu G, Zhang J, Zender L, Zhao A, Busuttil RW, Yee H, Stein L, French DM, Finn RS, Lowe SW, Powers S (2011) Identification of a therapeutic strategy targeting amplified FGF19 in liver cancer by oncogenomic screening. Cancer Cell 19:347–358. https://doi.org/10.1016/j.ccr.2011.01.040
Hagel M, Miduturu C, Sheets M, Rubin N, Weng W, Stransky N, Bifulco N, Kim JL, Hodous B, Brooijmans N, Shutes A, Winter C, Lengauer C, Kohl NE, Guzi T (2015) First selective small molecule inhibitor of FGFR4 for the treatment of hepatocellular carcinomas with an activated FGFR4 signaling pathway. Cancer Discov 5:424–437. https://doi.org/10.1158/2159-8290.CD-14-1029
French DM, Lin BC, Wang M, Adams C, Shek T, Hötzel K, Bolon B, Ferrando R, Blackmore C, Schroeder K, Rodriguez LA, Hristopoulos M, Venook R, Ashkenazi A, Desnoyers LR (2012) Targeting FGFR4 inhibits hepatocellular carcinoma in preclinical mouse models. PLoS ONE 7:e36713. https://doi.org/10.1371/journal.pone.0036713
Mavila N, James D, Utley S, Cu N, Coblens O, Mak K, Rountree CB, Kahn M, Wang KS (2012) Fibroblast growth factor receptor-mediated activation of AKT-β-catenin-CBP pathway regulates survival and proliferation of murine hepatoblasts and hepatic tumor initiating stem cells. PLoS ONE 7:e50401. https://doi.org/10.1371/journal.pone.0050401
Zhang J, Liu J, Liu L, McKeehan WL, Wang F (2012) The fibroblast growth factor signaling axis controls cardiac stem cell differentiation through regulating autophagy. Autophagy 8:690–691. https://doi.org/10.4161/auto.19290
Cinque L, Forrester A, Bartolomeo R, Svelto M, Venditti R, Montefusco S, Polishchuk E, Nusco E, Rossi A, Medina DL, Polishchuk R, De Matteis MA, Settembre C (2015) FGF signalling regulates bone growth through autophagy. Nature 528:272–275. https://doi.org/10.1038/nature16063
Yuan H, Li ZM, Shao J, Ji WX, Xia W, Lu S (2017) FGF2/FGFR1 regulates autophagy in FGFR1-amplified non-small cell lung cancer cells. J Exp Clin Cancer Res 36:72. https://doi.org/10.1186/s13046-017-0534-0
Kiyono K, Suzuki HI, Matsuyama H, Morishita Y, Komuro A, Kano MR, Sugimoto K, Miyazono K (2009) Autophagy is activated by TGF-β and potentiates TGF-β-mediated growth inhibition in human hepatocellular carcinoma cells. Cancer Res 69:8844–8852. https://doi.org/10.1158/0008-5472.CAN-08-4401
Ma CL, Qiao S, Li YC, Wang XF, Sun RJ, Zhang X, Qian RK, Song SD (2017) TGF-β1 promotes human hepatic carcinoma HepG2 cells invasion by upregulating autophagy. Eur Rev Med Pharmacol Sci 21:2604–2610
Zong Y, Panikkar A, Xu J, Antoniou A, Raynaud P, Lemaigre F, Stanger BZ (2009) Notch signaling controls liver development by regulating biliary differentiation. Development 136:1727–1739. https://doi.org/10.1242/dev.029140
Zeng J, Jing Y, Shi R, Pan X, Lai F, Liu W, Li R, Gao L, Hou X, Wu M, Wei L (2016) Autophagy regulates biliary differentiation of hepatic progenitor cells through Notch1 signaling pathway. Cell Cycle 15:1602–1610. https://doi.org/10.1080/15384101.2016.1181234
Wu X, Fleming A, Ricketts T, Pavel M, Virgin H, Menzies FM, Rubinsztein DC (2016) Autophagy regulates Notch degradation and modulates stem cell development and neurogenesis. Nat Commun 7:10533. https://doi.org/10.1038/ncomms10533
Vujovic F, Hunter N, Farahani RM (2019) Notch pathway: a bistable inducer of biological noise? Cell Commun Signal 17:133. https://doi.org/10.1186/s12964-019-0453-0
Wang M, Xue L, Cao Q, Lin Y, Ding Y, Yang P, Che L (2009) Expression of Notch1, Jagged1 and beta-catenin and their clinicopathological significance in hepatocellular carcinoma. Neoplasma 56:533–541. https://doi.org/10.4149/neo_2009_06_533
Croquelois A, Blindenbacher A, Terracciano L, Wang X, Langer I, Radtke F, Heim MH (2005) Inducible inactivation of Notch1 causes nodular regenerative hyperplasia in mice. Hepatology 41:487–496. https://doi.org/10.1002/hep.20571
Khalaf AM, Fuentes D, Morshid AI, Burke MR, Kaseb AO, Hassan M, Hazle JD, Elsayes KM (2018) Role of Wnt/β-catenin signaling in hepatocellular carcinoma, pathogenesis, and clinical significance. J Hepatocell Carcinoma 5:61–73. https://doi.org/10.2147/JHC.S156701
Turcios L, Chacon E, Garcia C, Eman P, Cornea V, Jiang J, Spear B, Liu C, Watt DS, Marti F, Gedaly R (2019) Autophagic flux modulation by Wnt/β-catenin pathway inhibition in hepatocellular carcinoma. PLoS One 14:e0212538. https://doi.org/10.1371/journal.pone.0212538
Petherick KJ, Williams AC, Lane JD, Ordóñez-Morán P, Huelsken J, Collard TJ, Smartt HJM, Batson J, Malik K, Paraskeva C, Greenhough A (2013) Autolysosomal β-catenin degradation regulates Wnt-autophagy-p62 crosstalk. EMBO J 32:1903–1916. https://doi.org/10.1038/emboj.2013.123
Fan Q, Yang L, Zhang X, Ma Y, Li Y, Dong L, Zong Z, Hua X, Su D, Li H, Liu J (2018) Autophagy promotes metastasis and glycolysis by upregulating MCT1 expression and Wnt/β-catenin signaling pathway activation in hepatocellular carcinoma cells. J Exp Clin Cancer Res 37:9. https://doi.org/10.1186/s13046-018-0673-y
Ma Z, Li F, Chen L, Gu T, Zhang Q, Qu Y, Xu M, Cai X, Lu L (2019) Autophagy promotes hepatic differentiation of hepatic progenitor cells by regulating the Wnt/β-catenin signaling pathway. J Mol Histol 50:75–90. https://doi.org/10.1007/s10735-018-9808-x
Kim JY, Lee HY, Park KK, Choi YK, Nam JS, Hong IS (2016) CWP232228 targets liver cancer stem cells through Wnt/β-catenin signaling: A novel therapeutic approach for liver cancer treatment. Oncotarget 7:20395–20409. https://doi.org/10.18632/oncotarget.7954
Bhat P, Kriel J, Shubha Priya B, Basappa SNS, Loos B (2018) Modulating autophagy in cancer therapy: advancements and challenges for cancer cell death sensitization. Biochem Pharmacol 147:170–182. https://doi.org/10.1016/j.bcp.2017.11.021
Galluzzi L, Bravo-San Pedro JM, Levine B, Green DR, Kroemer G (2017) Pharmacological modulation of autophagy: Therapeutic potential and persisting obstacles. Nat Rev Drug Discov 16:487–511. https://doi.org/10.1038/nrd.2017.22
Acknowledgements
We would like to thank Sunway University Postgraduate Degree by Research Scholarship for supporting M. M-.T.W. and H-.Y.C. This work was partly funded by Ministry of Higher Education Malaysia (FRGS/1/2019/SKK08/SYUC/02/1); and Sunway Medical Centre Research Funds (SRC/002/2017/FR and SRC/003/ 2017/FR).
Author information
Authors and Affiliations
Contributions
SYT, TSR and SCP conceived and designed the analysis, MMTW and HYC wrote the paper, JJB, NAA, ESC and SA reviewed and edited the paper. All authors have read and agreed to the manuscript submission.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wong, M.MT., Chan, HY., Aziz, N.A. et al. Interplay of autophagy and cancer stem cells in hepatocellular carcinoma. Mol Biol Rep 48, 3695–3717 (2021). https://doi.org/10.1007/s11033-021-06334-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11033-021-06334-9