Abstract
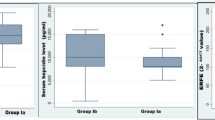
Iron overload is the main cause of morbidity and mortality in β-thalassemia major patients, and cardiac iron overload is the most common reason for death in these transfusion-dependent patients. Hepcidin, a liver-derived peptide hormone, plays a key role in plasma iron levels regulation by controlling two main stages, digestive iron absorption in enterocytes, and iron recycling in macrophages. Although hepcidin is mainly secreted from hepatocytes in the liver, it is also synthesized from mononuclear cells consisting of monocytes and lymphocytes. Binding of this molecule to ferroportin, a specific cellular exporter of iron, leads to degradation of the ligand-receptor complex, which reduces the iron overload by lowering the amounts of iron released into the plasma. Likewise, the same mechanism has been proved to be true for lymphocyte-drived hepcidin. The expression levels of hepcidin mRNA were evaluated using quantitative real time PCR (qRT-PCR) in 50 β-thalassemia major patients, as well as 25 healthy volunteers as the group of control. There was a significantly positive correlation between the cardiac iron concentration, showed by higher T2 values, and hepcidin levels in the patients (p = 0.028; r = 0.311). However, hepcidin expression levels did not significantly correlate with ferritin and liver iron concentrations. Hepcidin can act as a beneficial marker to determine iron overload degrees, particularly in the heart, in β-thalassemia major patients and be used as a logical therapeutic agent for treatment of β-thalassemia disorders.

Similar content being viewed by others
References
Higgs DR, Engel JD, Stamatoyannopoulos G (2012) Thalassaemia. Lancet 379(9813):373–383
De Sanctis V, Kattamis C, Canatan D, Soliman AT, Elsedfy H, Karimi M et al (2017) β-Thalassemia distribution in the old world: an ancient disease seen from a historical standpoint. Mediterr J Hematol Infect Dis 9(1):e2017018
Karimi M, Bonyadi M, reza Galehdari M, Zareifar S (2008) Termination of pregnancy due to thalassemia major, hemophilia, and down’s syndrome: the views of Iranian physicians. BMC Med Ethics 9(1):19
Ngim CF, Lai NM, Ibrahim H, Ratnasingam V (2013) Attitudes towards prenatal diagnosis and abortion in a multi-ethnic country: a survey among parents of children with thalassaemia major in Malaysia. J Community Genet 4(2):215–221
Rund D, Rachmilewitz E (2000) New trends in the treatment of β-thalassemia. Crit Rev Oncol Hematol 33(2):105–118
Ghotbi N, Tsukatani T (2005) Evaluation of the national health policy of thalassaemia screening in the Islamic Republic of Iran. EMHJ-East Mediterr Health J 11(3):308–318
Pennell DJ, Udelson JE, Arai AE, Bozkurt B, Cohen AR, Galanello R et al (2013) Cardiovascular function and treatment in β-thalassemia major: a consensus statement from the American Heart Association. Circulation 128(3):281–308
Krittayaphong R, Viprakasit V, Saiviroonporn P, Siritanaratkul N, Siripornpitak S, Meekaewkunchorn A et al (2017) Prevalence and predictors of cardiac and liver iron overload in patients with thalassemia: a multicenter study based on real-world data. Blood Cells Mol Dis 66:24–30
Kemna EH, Tjalsma H, Willems HL, Swinkels DW (2008) Hepcidin: from discovery to differential diagnosis. Haematologica 93(1):90–97
Nemeth E (2010) Hepcidin in β-thalassemia. Ann N Y Acad Sci 1202:31
Ganz T (2011) Hepcidin and iron regulation, 10 years later. Blood 117(17):4425–4433
Pratummo K, Jetsrisuparb A, Fucharoen S, Tripatara A (2014) Hepcidin expression from monocyte of splenectomized and non-splenectomized patients with HbE-β-thalassemia. Hematology 19(3):175–180
Pinto JP, Dias V, Zoller H, Porto G, Carmo H, Carvalho F et al (2010) Hepcidin messenger RNA expression in human lymphocytes. Immunology 130(2):217–230
Pak M, Lopez MA, Gabayan V, Ganz T, Rivera S (2006) Suppression of hepcidin during anemia requires erythropoietic activity. Blood 108(12):3730–3735
Nemeth E, Tuttle MS, Powelson J, Vaughn MB, Donovan A, Ward DM et al (2004) Hepcidin regulates cellular iron efflux by binding to ferroportin and inducing its internalization. Science 306(5704):2090–2093
Aschemeyer S, Qiao B, Stefanova D, Valore EV, Sek AC, Ruwe TA et al (2018) Structure-function analysis of ferroportin defines the binding site and an alternative mechanism of action of hepcidin. Blood 131(8):899–910
Evstatiev R, Gasche C (2012) Iron sensing and signalling. Gut 61(6):933–952
Pasricha S-R, Frazer DM, Bowden DK, Anderson GJ (2013) Transfusion suppresses erythropoiesis and increases hepcidin in adult patients with β-thalassemia major: a longitudinal study. Blood 122(1):124–133
Wrighting DM, Andrews NC (2006) Interleukin-6 induces hepcidin expression through STAT3. Blood 108(9):3204–3209
Zhao N, Zhang A-S, Enns CA (2013) Iron regulation by hepcidin. J Clin Investig 123(6):2337–2343
Kaddah AM, Abdel-Salam A, Farhan MS, Ragab R (2017) Serum hepcidin as a diagnostic marker of severe iron overload in beta-thalassemia major. Indian J Pediatr 84(10):745–750
Origa R, Galanello R, Ganz T, Giagu N, Maccioni L, Faa G et al (2007) Liver iron concentrations and urinary hepcidin in β-thalassemia. Haematologica 92(5):583–588
Kaddah NA, El-Gindi HD, Mostafa NO, El-Aziz A, Nevin M, Kamhawy AH (2011) Role of hepcidin in the pathogenesis of iron overload in children with b-thalassemia. Int J Acad Res 3(4):62
Chauhan R, Sharma S, Chandra J (2014) What regulates hepcidin in poly-transfused β-thalassemia major: erythroid drive or store drive? Indian J Pathol Microbiol 57(1):39
Camberlein E, Zanninelli G, Détivaud L, Lizzi AR, Sorrentino F, Vacquer S et al (2008) Anemia in β-thalassemia patients targets hepatic hepcidin transcript levels independently of iron metabolism genes controlling hepcidin expression. Haematologica 93(1):111–115
El Beshlawy A, Alaraby I, Abdel Kader MS, Ahmed DH, Abdelrahman HE (2012) Study of serum hepcidin in hereditary hemolytic anemias. Hemoglobin 36(6):555–570
Ravasi G, Pelucchi S, Trombini P, Mariani R, Tomosugi N, Modignani GL et al (2012) Hepcidin expression in iron overload diseases is variably modulated by circulating factors. PLoS ONE 7(5):e36425
Hendy O, Allam M, Allam A, Attia M, El ST, Eldin M et al (2010) Hepcidin levels and iron status in beta-thalassemia major patients with hepatitis C virus infection. Egypt J immunol 17(2):33–44
Aboul-Enein A, Amal E-B, Hamdy M, Shaheen I, El-Saadany Z, Samir A et al (2015) Peripheral expression of hepcidin gene in Egyptian β-thalassemia major. Gene 564(2):206–209
Khaled A, Ezzat DA, Salem HA, Seif HM, Rabee H (2019) Effective method of evaluating myocardial iron concentration in pediatric patients with thalassemia major. J Blood Med 10:227
Ansari S, Azarkeivan A, Miri-Aliabad G, Yousefian S, Rostami T (2017) Comparison of iron chelation effects of deferoxamine, deferasirox, and combination of deferoxamine and deferiprone on liver and cardiac T2* MRI in thalassemia maior. Casp J Intern Med 8(3):159
Modell B, Khan M, Darlison M (2000) Survival in β-thalassaemia major in the UK: data from the UK thalassaemia register. Lancet 355(9220):2051–2052
Nemeth E (2013) Hepcidin and β-thalassemia major. Blood J Am Soc Hematol 122(1):3–4
Longo F, Zecchina G, Sbaiz L, Fischer R, Piga A, Camaschella C (1999) The influence of hemochromatosis mutations on iron overload of thalassemia major. Haematologica 84(9):799–803
Sharma V, Panigrahi I, Dutta P, Tyagi S, Choudhry VP, Saxena R (2007) HFE mutation H63D predicts risk of iron over load in thalassemia intermedia irrespective of blood transfusions. Indian J Pathol Microbiol 50(1):82–85
Nemeth E, Ganz T (2006) Hepcidin and iron-loading anemias. Haematologica 91(6):727–732
Kearney SL, Nemeth E, Neufeld EJ, Thapa D, Ganz T, Weinstein DA et al (2007) Urinary hepcidin in congenital chronic anemias. Pediatr Blood Cancer 48(1):57–63
Kemna E, Tjalsma H, Laarakkers C, Nemeth E, Willems H, Swinkels D (2005) Novel urine hepcidin assay by mass spectrometry. Blood 106(9):3268–3270
Nicolas G, Chauvet C, Viatte L, Danan JL, Bigard X, Devaux I et al (2002) The gene encoding the iron regulatory peptide hepcidin is regulated by anemia, hypoxia, and inflammation. J Clin Investig 110(7):1037–1044
Kattamis A, Papassotiriou I, Palaiologou D, Apostolakou F, Galani A, Ladis V et al (2006) The effects of erythropoetic activity and iron burden on hepcidin expression in patients with thalassemia major. Haematologica 91(6):809–812
Pasricha S-R, Frazer DM, Bowden DK, Anderson GJ (2013) Transfusion suppresses erythropoiesis and increases hepcidin in adult patients with β-thalassemia major: a longitudinal study. Blood J Am Soc Hematol 122(1):124–133
Haghpanah S, Esmaeilzadeh M, Honar N, Hassani F, Dehbozorgian J, Rezaei N et al (2015) Relationship between serum hepcidin and ferritin levels in patients with thalassemia major and intermedia in Southern Iran. Iran Red Crescent Med J 17(7):e28343
Papanikolaou G, Tzilianos M, Christakis JI, Bogdanos D, Tsimirika K, MacFarlane J et al (2005) Hepcidin in iron overload disorders. Blood 105(10):4103–4105
Wish JB (2006) Assessing iron status: beyond serum ferritin and transferrin saturation. Clin J Am Soc Nephrol 1(Supplement 1):S4–S8
Tang MY, Chen TW, Zhang XM, Huang XH (2014) GRE T2-weighted MRI: principles and clinical applications. BioMed Res Int. https://doi.org/10.1155/2014/312142
Said Othman KM, Elshazly SA, Heiba NM (2014) Role of non-invasive assessment in prediction of preclinical cardiac affection in multi-transfused thalassaemia major patients. Hematology 19(7):380–387
Bartnikas TB, Fleming MD (2010) A tincture of hepcidin cures all: the potential for hepcidin therapeutics. J Clin Investig 120(12):4187–4190
Gardenghi S, Ramos P, Marongiu MF, Melchiori L, Breda L, Guy E et al (2010) Hepcidin as a therapeutic tool to limit iron overload and improve anemia in β-thalassemic mice. J Clin Investig 120(12):4466–4477
Ramos E, Ruchala P, Goodnough JB, Kautz L, Preza GC, Nemeth E et al (2012) Minihepcidins prevent iron overload in a hepcidin-deficient mouse model of severe hemochromatosis. Blood J Am Soc Hematol 120(18):3829–3836
Katsarou A, Pantopoulos K (2018) Hepcidin therapeutics. Pharmaceuticals 11(4):127
Corradini E, Schmidt PJ, Meynard D, Garuti C, Montosi G, Chen S et al (2010) BMP6 treatment compensates for the molecular defect and ameliorates hemochromatosis in Hfe knockout mice. Gastroenterology 139(5):1721–1729
Rivera S, Nemeth E, Gabayan V, Lopez MA, Farshidi D, Ganz T (2005) Synthetic hepcidin causes rapid dose-dependent hypoferremia and is concentrated in ferroportin-containing organs. Blood 106(6):2196–2199
Morán-Jiménez MJ, Méndez M, Santiago B, Rodríguez‐García ME, Moreno‐Carralero MI, Sánchez‐Lucío AC et al (2010) Hepcidin treatment in Hfe–/– mice diminishes plasma iron without affecting erythropoiesis. Eur J Clin Invest 40(6):511–517
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ayatollahi, H., Mousavi Nezhad, S.F., Talebpour, A. et al. Relation of hepcidin gene expression in blood mononuclear cells with iron overload severity among β-thalassemia major patients. Mol Biol Rep 47, 9353–9359 (2020). https://doi.org/10.1007/s11033-020-06012-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11033-020-06012-2