Abstract
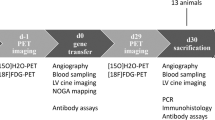
Despite advances in surgical and reperfusion therapy, there is no effective therapy currently exists to prevent the progressive decline in cardiac function following myocardial infarction. Hepatocyte growth factor has potent angiogenic and anti-apoptotic activities. The aim of this study was to investigate the therapeutic effect and dose–effect relationship on postinfarction heart failure with different doses of adenovirus-mediated human hepatocyte growth factor (Ad5-HGF) transference in swine models. Totally twenty swine were randomly divided into four groups: (a) control group (null- Ad5, 1 ml); (b) low-dose group (1 × 109 Pfu/ml Ad5-HGF, 1 ml); (c) medium-dose group (5 × 109 Pfu/ml Ad5-HGF, 1 ml); (d) high-dose group (1 × 1010 Pfu/ml Ad5-HGF, 1 ml). Four weeks after left anterior descending coronary artery (LAD) ligation, different doses of Ad5-HGF were transferred in three therapeutic groups via right coronary artery. Four and seven weeks after LAD ligation, gate cardiac perfusion imaging was performed to evaluate cardiac perfusion and left ventricular ejection fraction (LVEF). Seven weeks after surgery, the apoptotic index of cardiocyte was observed by TUNEL, the expression of Bcl-2, Bax, α-SMA and Factor VIII in the border zones were evaluated by immunohistochemistry, respectively. Four weeks after myocardial infarction, no significant difference was observed among four groups. Three weeks after Ad5-HGF transfer, the improvement of cardiac perfusion and LVEF was obviously observed, especially after 1 × 1010 Pfu Ad5-HGF transfer. TUNEL assay showed that 5 × 109 Pfu and 1 × 1010 Pfu Ad5-HGF treatment had a obvious reduction in the apoptotic index compared with the null-Ad5 group, especially after 1 × 1010 Pfu Ad5-HGF treatment. The expression of Bcl-2 protein was increased and the expression of Bax protein was inhibited in the 5 × 109 Pfu and 1 × 1010 Pfu Ad5-HGF groups compared with the null-Ad5 group. The vessel density of Factor VIII+ and α-SMA+ was increased in Ad5-HGF groups compared with the null-Ad5 group. There were no significant differences in angiogenesis, reducing apoptosis and ameliorating heart function between the 1 × 109 Pfu Ad5-HGF group and the null-Ad5 group. Although no statistical difference was observed between 1 × 1010 Pfu and 5 × 109 Pfu Ad5-HGF groups, the cardiac protective effects of 1 × 1010 Pfu Ad5-HGF treatment were greater than 5 × 109 Pfu Ad5-HGF treatment. Different doses of Ad5-HGF injected via noninfarct-related artery could induce angiogenesis, reduce apoptosis and ameliorate heart function, and the cardiac protective effects of 1 × 1010 Pfu Ad5-HGF is of most significance.



Similar content being viewed by others
References
Janasankar V, Woo YJ, Pirolli TJ et al (2005) Induction of angiogenesis and inhibition of apoptosis by hepatocyte growth factor effectively treats postischemic heart failure. J Card Surg 20(1):93–101
Hongkui Jin J, Wyss JM, Yang RH et al (2004) The therapeutic potential of hepatocyte growth factor for myocardial infarction and heart failure. Curr Pharm Des 10:2525–2533
Morishita R, Nakamura S, Hayashi S et al (1999) Therapeutic angiogenesis induced by human recombinant hepatocyte growth factor in rabbit hind limb ischemia model as cytokine supplement therapy. Hypertension 33:1379–1384
Xiaoqin HA, Bin Y, Yuanmin LI et al (2003) Gene therapy for pathological scar with hepatocyte growth factor mediated by recombinant adenovirus vector. Sci China 46(3):320–327
Wei W, Zhi-jian Y, Dong-chao MA et al (2006) Induction of collateral artery growth and improvement of post-infart heart function by hepatocyte growth factor gene transfer. Acta Pharmacol Sin 27(5):555–560
Cerqueira MD, Weissman NJ, Dilsizian V et al (2002) Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart: a statement for healthcare professionals from the Cardiac Imaging Committee of the Council on Clinical Cardiology of the American Heart Association [J]. Circulation 105(4):539–542
Poornima IG, Miller TD, Christian TF et al (2004) Utility of myocardial perfusion imaging in patients with low-risk treadmill scores. J Am Coll Cardiol 43:194–199
Li Y, Takemura G, Kosai K et al (2003) Postinfarction treatment with an adenoviral vector expressing hepatocyte growth factor relieves chronic left ventricular remodeling and dysfunction in mice. Circulation 107:2499–2506
Salam AM (2003) Selective aldosterone blockade with eplerenone in patients with congestive heart failure. Expert Opin Investig Drugs 12(8):1423–1427
Jayasankar V, Joseph Woo Y, Bish LT (2003) Gene transfer of hepatocyte growth factor attenuates postinfarction heart failure. Circulation 108:230–236
Yamaguchi T, Miyamoto Y, Takahashi T et al (2005) Therapeutic angiogenesis induced by injecting hepatocyte growth factor in ischemic canine hearts. Surg Today 35(10):855–860
Yang Z, Ma D, Wang W et al (2007) Neovascularization and cardiomyocytes regeneration in acute myocardial infarction after bone marrow stromal cell transplantation: comparison of infarct-relative and noninfarct-relative arterial approaches in swine. Clin Chim Acta 381(2):114–118
Yang Z, Ma D, Wang W et al (2006) Experimental study of bone marrow-derived mesenchymal stem cells combined with hepatocyte growth factor transplantation via noninfarct-relative artery in acute myocardial infarction. Gene Ther 13(22):1564–1568
Ma H, Calderon TM, Fallon JT et al (2002) Hepatocyte growth factor is a survival factor for endothelial cells and is expressed in human atherosclerotic plaques [J]. Atherosclerosis 64(1):79–87
Wu D, Zhang Y, Lao M et al (2004) Therapeutic induction of angiogenesis by direct myocardial administration of an adenovirus vector encoding human hepatocyte growth factor gene and its safety. Chin Sci Bull 49(14):1464–1469
Ono K, Matsumori A, Shioi T et al (1997) Enhanced expression of hepatocyte growth factor/c-Met by myocardial ischemia and reperfusion in a rat model. Circulation 95:2552
Sato T, Tani Y, Murao S et al (2001) Focal enhancement of expression of c-Met/hepatocyte growth factor receptor in the myocardium in human myocardial infarction. Cardiovasc Pathol 10(5):235–240
Acknowledgments
This work was financially supported by a project grant of “the key faculty of Medical Renaissance program of Jiangsu province”.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yang, Zj., Chen, B., Sheng, Z. et al. Improvement of heart function in postinfarct heart failure swine models after hepatocyte growth factor gene transfer: comparison of low-, medium- and high-dose groups. Mol Biol Rep 37, 2075–2081 (2010). https://doi.org/10.1007/s11033-009-9665-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11033-009-9665-5