Abstract
Blunted motivation is a core symptom of Major Depressive Disorder (MDD). Although the empirical picture is mixed, cognitive processes that can be collectively referred to as reward processing have been found to be consistently muted in MDD; most notably, reward sensitivity and reinforcement learning. Works on the modulation of response vigor in individuals with MDD have examined various types of reward, but recent research has shown that in the general population, response vigor is not modulated by type of reward on tasks that are highly similar to those used in these experiments. The present study implemented a form of non-reward related reinforcement which has repeatedly been shown to modulate response vigor in the general population. It investigated whether modulation of response vigor by this type of reinforcement would be effective in individuals with MDD. Clinically depressed individuals (N = 121; 76 post-exclusion) engaged in a task in which their responses led to predictable and immediate sensorimotor effects, or no such effects. Response vigor increased when responses led to sensorimotor effects, which was comparable to the increase found in the general population. These findings support the utility of isolating the computations leading to different reinforcement types and suggest that motivational deficits in MDD may be specific to the type of reward (i.e., hedonically or otherwise explicitly desired stimuli). These results contribute to the literature by suggesting that the reinforcement from sensorimotor predictability stems from processes devolved to motor control, whereas reinforcement from rewards may depend on more general-purpose processes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Major depressive disorder
Major Depressive Disorder (MDD) is highly prevalent with a lifetime prevalence estimated at 13.5–21.2% of the general population (Kessler et al., 2005). Depression affects ~ 5% of the population globally, making it the leading cause of disability and ill-health worldwide (World Health Organization, 2017). MDD is characterized by impaired functioning and symptoms such as loss of energy, difficulties concentrating, fluctuations in weight, and feelings of worthlessness. Diminished interest or pleasure in daily activities is a key symptom of MDD, and is manifested by difficulties carrying out one’s daily routine (DSM-V; American Psychiatric Association, 2013).
Reward processing and motivated behavior
The motivational deficits observed in MDD are thought to be linked to the processes governing reward-seeking behaviors, including reward anticipation, attainment, and learning, which are collectively referred to as the Positive Valence System (PVS; National Institute of Mental Health, 2011; Olino, 2016). Another more detailed mechanistic parsing of motivational deficits was proposed by Husain and Roiser (2018), who suggested that a dysfunction in any one or more of the stages of effort-based decision-making to obtain a reward may underlie a-motivation in MDD and in other psychiatric and neurological conditions (Husain & Roiser, 2018). More broadly, the conceptualization of reward processing as a range, ensemble, or system has allowed for a more fine-grained characterization of the impairments in depression across various reward-related processes.
This differentiation of motivational deficits into sub-processes also helps reconcile the conflicting findings in the field. Although some studies have failed to provide robust evidence for reduced reward responsiveness and/or motivation in individuals with MDD (e.g., Moutoussis et al., 2018; Rothkirch et al., 2017; Winter et al., 2021), there is a growing consensus that MDD is linked to substantial impairment in some but not other facets of reward processing (e.g., Gradin et al., 2011; Huys et al., 2013; Pizzagalli et al., 2008; Proudfit, 2015).
Specifically, a recent meta-analysis by Halahakoon et al. (2020) drew two key conclusions that are directly related to the current study. The first is the substantial behavioral evidence supporting disrupted reward processing in MDD. The second is that this evidence varies substantially in strength across facets of reward processes. The strongest evidence points to less reward bias in MDD; i.e., a reduction in the adaptive preference for selecting more rewarding options. By contrast, there is scant evidence indicative of an association between MDD and impairments in response vigor, with the available evidence being extremely weak, if not altogether absent.
Different measures tap into the influence of different circuits of reinforcement
The Halahakoon et al. meta-analysis of 48 studies cited above included 12 studies that measured differences in response vigor, all of which involved monetary or social rewards and implemented variants on the Monetary Incentive Delay Task (Knutson et al., 2000). As noted in the overview, this measure of response vigor, when indexed by reaction time, captures response execution and not the decision to (and how to) act (Halahakoon et al., 2020).
Nevertheless, this presumed dissociation between intact reward processing at the response execution level and aberrant reward processing at the action selection level was challenged by a study showing that monetary value alone failed to consistently reduce reaction time in the general population when the action selection phase was held constant; in other words, when the action execution phase was isolated (Karsh et al., 2020). If rewards do not consistently increase the speed of response execution in general, it should come as no surprise that there is no convincing evidence for a reaction time difference between individuals with MDD and healthy controls in the rewarded versus unrewarded conditions on a response vigor task based on RT. Conversely, in the Karsh et al. (2020) study, the so-called pure effectiveness feedback, i.e., a response contingent but task-irrelevant perceptual change, did indeed consistently shorten response times in the general population.
Reinforcement as a function of desired outcomes and sensorimotor predictability
The finding that decision-uninformative feedback facilitates response execution is consistent with the theoretical and empirical differentiation between the well-documented modulation of behavior by desired outcomes (incentives or rewards) and another very rarely explored source of reinforcement from the confirmation of sensorimotor predictions (Bednark & Franz, 2014; Eitam et al., 2013; Hemed et al., 2020, Hemed et al., 2022; Karsh et al., 2016, 2020, 2021; Karsh & Eitam, 2015a; Penton et al., 2018; Tanaka et al., 2021; Wen et al., 2018; Wen & Imamizu, 2022). However, systematic experimentation supports the conclusion that control feedback reinforces behavior exclusively at the level of response execution, regardless of whether it is hedonically charged or valenced. Over 15 general population studies have shown that when responses are followed by an immediate and predictable own-response-contingent effect, response time is faster by about 40 ms than when no such feedback, or subtly lagged feedback, is delivered (Eitam et al., 2013; Karsh et al., 2016), or alternatively when (sensorially) the immediate feedback is unpredictable (Karsh et al., 2016).
Currently, the general assumption in the literature is that this facilitation reflects the workings of a modular reinforcement mechanism that is independent of the appetitive, valence, or hedonic value of a stimulus or abstract cognition. Rather, this mechanism is activated when an incoming sensation confirms a sensorimotor prediction. These predictions are generated by the system that controls motor movements and are produced unconsciously by mental processes that allow volitional movement whenever a voluntary movement is initiated (Eitam et al., 2013; Hemed et al., 2020, 2022; Karsh & Eitam, 2015a, 2015b; Karsh et al., 2016). The hypothesized mechanism, depicted in Fig. 1, is referred to as Reinforcement from Sensorimotor Predictability or RSP. The robust empirical effect of sensory feedback documented in the general population, and RSP theory that links it to the value-free reinforcement of response execution, enables a novel test of whether facilitation of response vigor, as a function of a non-reward related reinforcement, is aberrant in MDD.
RSP as a novel form of primary reinforcement that exclusively affects motor programing but not abstract response (action) representations. Note: Schematic illustration of the control-based response selection framework. The framework highlights the role of the Reinforcement from Sensorimotor Predictability (RSP) in reinforcing specific motor response parameters, as represented by the rhombuses (r1,…,rn). However, RSP does not influence the selection of abstract actions, denoted by the upper rectangles (R1,…,Rn), or the allocation of effort, both of which are decision-based processes. Dashed arrows indicate the flow of relevant information for explicit judgments of an action's effectiveness. Dotted arrows depict the generation of a forward model, which predicts the anticipated effect of a motor program on the environment and compares it to the perceived motor-program-related effect. Adapted from Karsh et al. (2016)
Is reinforcement by sensorimotor predictability intact in MDD?
The present study examined whether modulation of response vigor by a reinforcement process that is not driven by rewards is intact in MDD. To do so, we tested whether individuals with mild–moderate MDD would display a weaker modulation of response vigor due to confirmation of sensorimotor predictions (the RSP process) on the Effect Motivation Task. If MDD is associated with a lack of modulation of response vigor, individuals with MDD should be less sensitive to sensorimotor feedback than in the general population, and there should be no response time facilitation. Conversely, finding that sensorimotor feedback modulates response vigor in MDD would be strong evidence that action execution is sensitive to reinforcement in this condition, at least for this type of reinforcement. Since in our theoretical framework this type of reinforcement does not rely on reward sensitivity as manifested in action selection or decision-making (Karsh et al., 2016, 2020), we expected that individuals with MDD would exhibit a modulation of response vigor due to RSP. Specifically, the presence (vs. absence) of sensorimotor feedback was predicted to facilitate response time.
Method
Overview
Data were collected over a 3-year period (2016–2018), as part of the training and active phases of an ongoing randomized controlled trial involving supportive expressive therapy for depression (Zilcha-Mano et al., 2018, 2021). The experiment described below examined the trial, pre-treatment phase. Patients were recruited through advertisements offering free treatment at the Psychotherapy Research Lab’s Clinic. Applicants interested in participating attended two pretreatment assessments, after providing written informed consent. The present study was conducted during the second pretreatment assessment.Footnote 1
This assessment included the administration of the Hamilton Rating Scale for Depression (HRSD; Hamilton, 1960), the MINI—International Neuropsychiatric Interview (Sheehan et al., 1998), and the Beck Depression Inventory BDI-II (Beck et al., 1996). In addition, structured interviews were conducted, and the participants also completed a baseline battery of questionnaires covering demographic information, concurrent medication, and personality characteristics.
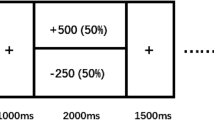
The Effect Motivation Task (EMT; see Fig. 2) was administered after this battery (approximately 1.5 h into the second pretreatment assessment). Participants then filled in a post-task questionnaire on their perceived control and effort during the task.
The Effect Motivation Task (EMT). Note: Participants are instructed to respond with a keypress, given an imperative cue (a colored circle moving down the screen on a designated path). In the Sensorimotor-Feedback condition (B), a valid keypress turns the colored circle white mid-fall for 100 ms and then vanishes. In the No-feedback condition (A), a keypress results in no perceivable change on the screen and the circle descends uninterrupted to the bottom of the screen (Color figure online)
Participants
The sample was composed of participants seeking treatment for depression as part of the training and active phase of an ongoing randomized controlled trial (N = 121, mean age = 30.69, SD = 8.47, range 19–59; 41% men). Only those who met the clinical criteria for depression were included in the analysis (see below), resulting in a final sample of 80 participants with MDD (mean age = 31.61, SD = 8.45, 39% men). Participants described themselves as being Jewish (n = 66; 82.5%), Christian (n = 8; 10%), Muslim (n = 3; 3.75%), or atheist (n = 2; 2.5%). Of the sample, 55.13% reported having a below-average income, 25.64% indicated an average income, and 19.23% an above-average income on the pre-treatment questionnaire. Most participants (63.75%) reported having 13–20 years of education; 32.5% had a high school education (12 years) and a small minority reported having fewer than 12 years or more than 20 years of education (3.75%), for an overall mean of 14.61 years of education (SD = 2.74, range 7–25). There were no significant differences between the experimental condition groups on any of the background variables (Table 1).
The participants were considered to have MDD if they met the following criteria: (a) a diagnosis based on the structured clinical interview (MINI), and (b) a score above 14 on the 17-item HRSD during the two pretreatment assessments, administered 1 week apart. If they met only one criterion [HRSD score < 14 (8 participants) or did not meet the MINI diagnostic criteria (33 participants)], they were excluded from the main analyses.Footnote 2 However, these participants constituted the sub-clinical comparison group (see Fig. 6). The sociodemographic information and additional analyses pertaining to the participants in this group appear in the Supplementary Information.
All participants took the EMT after being randomly assigned to one of two conditions: Sensorimotor-feedback (N = 61; post-exclusion N = 40) or No-feedback (N = 60; post exclusion N = 40). The task was administered before treatment began.Footnote 3
Given the considerable challenges involved in data collection for this population, the experiment ran for a period of 3 years to sample as many participants as possible. A sensitivity analysis was conducted after the pool of available participants was exhausted using G*Power V.3.1.9.2 (Faul et al., 2009). It indicated that a fixed-effect linear regression with 38 participants per group (N = 76) would be sensitive to effects of Cohen’s d = 0.65 with 80% power (α = 0.05, two-tailed). This means the current study could not reliably detect effects smaller than Cohen’s d = 0.65.
The effect motivation task
Participants were administered the EMT while seated in front of a computer screen with their fingers positioned on the standard PC keyboard keys of ‘D’, ‘F’, ‘J’, and ‘K’. Each trial began with the presentation of a response cue (a colored circle; 53 pixels in size) in the upper section of the game window (9.5 cm × 10 cm), in one of four possible horizontal locations. On appearance, the circle descended smoothly (“fell”) vertically to the bottom of the game window. Participants were instructed to ‘stamp’ the circle as quickly and accurately as possible by pressing the relevant key (spatially and color-coded). In the Sensorimotor-feedback condition, a valid keypress always resulted in the circle immediately flashing white for 100 ms (ms) and then disappearing. In the No-feedback condition, a valid keypress had no perceivable effect and the circle continued its descent until it disappeared when it reached the bottom of the screen. The descent gave participants 850 ms to respond (until the circle vanished from the game window). Importantly, the time between the appearance of one circle and the next (stimulus onset asynchrony, SOA) was kept constant at 1500 ms regardless of participants' reaction times. Participants completed 180 experimental trials; the approximate total duration of the task was ~ 7 min. Reaction time and the accuracy of the responses were recorded.
Post-task questionnaire
Immediately after the experimental procedure, all the participants filled in a computerized self-report questionnaire that assessed their perceived control, enjoyment, perceived effort, and self-reported motivation to perform the task and be effective (to succeed on the EMT, be quick, accurate, and “make the circle flash”) on a slider scale from 1 (not at all) to 100 (very much).
Measures
Behavioral measures
(1) Reaction Time (RT). RT served to test the main prediction that when sensorimotor predictions are confirmed by incoming sensations, the RTs should become consistently shorter, thus indexing increased vigor in response execution; (2) Accuracy: the proportion of correct responses out of the total number of responses. In previous experiments using this task, the percent correct has generally been very high. Studies have occasionally found a reduction in accuracy levels that has been attributed to speeding up (potentially due to an increased ‘urge’ to respond), but this pattern has not been consistent across experiments, with some studies (3 out of 8) reporting facilitation of RTs without a reduction in accuracy (see Fig. 6 for details of previous studies).
Depression levels
The primary measure of the level of depression was the HRSD, a 17-item clinically administered measure of severity of depression. Total scores range from 0 to 54, with higher scores indicating greater severity of depression. The inter-rater reliability, as assessed by intraclass correlations, was .97. We also assessed self-reported symptoms using the BDI-II. Analysis indicated that choice of measure used to diagnose MDD had no effect on the key results.
Ethical considerations
All participants provided written informed consent before any of the study procedures, in accordance with the requirements for the ethical conduct of human subject research. The study design, procedure, and informed consent form were approved by the University’s Ethics Committee (approval#:118/15). Participants received detailed information about the study procedure both orally and in writing. Participants received complete information about the implications of their participation, including potential risks, inconveniences, and benefits, their right to halt their participation at any time without adverse consequences, issues of confidentiality, etc. A detailed, comprehensive data management plan ensured careful handling of confidential data throughout all stages of the research process.
Results
All statistical analyses were performed using Stata 16 (StataCorp, 2019) and JASP 0.9 (JASP Team, 2018); plotting was produced with Stata’s bischofschemes package (Bischof, 2017) and Python's Seaborn package (Waskom, 2021).
Data preparation and screening
To enable comparison to previous studies using the EMT, before analyzing the data, we applied five filters based on previous studies using the EMT. We rejected data in the following cases: (i) below the accuracy threshold: participants with more than 50%Footnote 4 incorrect responses (1 participant, ~ 1% of the observations), (ii) aberrant response times for this task: responses that were either above 800 ms or below 200 ms (~ 2%), (iii) incorrect responses (~ 5%), (iv) trials that deviated from their condition’s mean by at least 2 standard deviations in mean reaction time (~ 4%), and (v) participants who deviated from their condition’s mean by at least 2 standard deviations in percent correct (3 participants, ~ 4%). After applying these filters, the number of participants in both conditions was identical (N = 38 in the No-feedback condition and N = 38 in the Sensorimotor-feedback condition).
Depression levels
The HRSD scores ranged from 14 to 31, whereas the BDI-II scores ranged from 11 to 59. The distribution of depression levels did not significantly differ between conditions (Fig. 3). The HRSD and BDI-II scores in the No-feedback condition were MHRSD = 20.21 (SD = 4.00) and MBDI-II = 27.18 (SD = 8.90), respectively. These scores were not significantly different from the scores in the Sensorimotor-feedback condition, which were MHRSD = 20.97 (SD = 4.63) and MBDI-II = 29.22 (SD = 7.34); see Supplementary Information for a detailed analysis.
Hamilton Rating Scale for Depression (HRSD) and Beck Depression Inventory-II (BDI-II) scores in the No-feedback and Sensorimotor-feedback conditions. Note: Red and blue dots are individual scores on the HRSD and BDI-II No-feedback and Sensorimotor-feedback conditions, respectively (Color figure online)
Behavioral measures
Reaction time
Given the relative ease of the task and generally very high accuracy of performance, reaction time (RT) is always taken as the key dependent measure on this task (Beierholm et al., 2013; Brown & Bowman, 1995; Griffiths & Beierholm, 2017; Haggard, 2008; Manohar et al., 2017; Pullman et al., 1988). A (fixed-effects) regression model was used to test the influence of sensorimotor feedback and depression level (and their interaction) on RT.Footnote 5 The first model included the HRSD score and Sensorimotor-feedback condition as predictors and was significant, explaining a substantial portion (25%) of the variance in RT (F(3,72) = 9.39, p < .001). Crucially, and fully replicating previous findings in the general population (Eitam et al., 2013; Hemed et al., 2020; Karsh et al., 2016, 2020; Karsh & Eitam, 2015a), there was a decisive main effect of sensorimotor feedback on RT (β = − .51, p < .001, BF = 2449.00Footnote 6). As shown in Fig. 4, responses were faster [Cohen's d = 1.16; 95% CI (.67, 1.64)] in the Sensorimotor-feedback condition (M = 469.83, SD = 52.73) than in the No-feedback condition (M = 540.87, SD = 69.10).
Reaction time (RT) as predicted by the Sensorimotor-feedback factor and depression level (HRSD) Note: In the scatter plot, individual dots represent participants' scores on the Hamilton Rating Scale for Depression (HRSD) and mean reaction time (RT). The bands on the plot represent the bootstrapped 95% confidence intervals of the slopes. Red indicates the No-feedback condition; blue indicates the Sensorimotor-feedback condition (Color figure online)
The apparent interaction in this model between sensorimotor feedback and HRSD was not significant when using the frequentist framework (β = − .22, p = .15, BF = .84). However, the Bayes factor for a model with two main effects as compared to one that also included the interaction term (i.e., a test of the strength of an interaction effect) showed that the data were in fact insensitive to an interaction effect. Further examination of the robustness of the interaction effect using the log-transformed RT and range-restricted data to better capture the actual range of observed data (and avoid the possible hyper-influence of a few extreme observations) and the inconsistency between the two measures of depression regarding the interaction (see below) suggested that additional data would be required to determine whether there was an interaction effect that could reflect the modulation of potential sensorimotor retardation by sensorimotor feedback.
We then tested a second fixed-effects linear regression model that included the participants' BDI score (instead of the HRSD score used in the first model) to index level of depression, with sensorimotor feedback (and the interaction) as predictors of reaction time. This yielded a similar pattern, explaining 24% of the variance in RT (F(3,72) = 8.86, p = < .001), where the Sensorimotor-feedback factor alone predicted RT (β = − .52, p < .001, BF = 2020.51). As shown in Fig. 5, neither the BDI scores nor their interaction with Sensorimotor-feedback condition were associated with RT [(β = .05, p = .71, BF = .52) and (β = .08, p = .55, BF = .47) respectively]. The model that was best supported by the data only contained sensorimotor feedback as a predictor of RT (see Supplementary Information).
Accuracy
Participants in the No-Feedback condition were significantly more accurate on average than participants in the Sensorimotor-feedback condition [t(74) = 4.35, p < .001, Cohen's d = 1.00; 95% CI (.52, 1.47), BF = 463.09]; see Table 2. Previous studies using a similar task in tests of the general population (Mean age = 22.98; SD = 4.38; 49% female) reported similar accuracy levels in both experimental conditions. As shown in Fig. 6c, d, the mean accuracy of 0.92 (SD = 0.06) in the No-feedback condition and a mean accuracy of 0.91 (SD = 0.05) in the Sensorimotor-feedback condition (Eitam et al., 2013, Experiments 1–3; Karsh et al., 2016, Experiments 1a, 2a, 2b; Karsh et al., 2020, Experiment 1b; Tanaka et al., 2021) were obtained.
The effect of sensorimotor feedback in MDD relative to the subclinical and general population samples Note: Mean reaction time [R and bootstrapped 95% confidence intervals (CI) for the Sensorimotor-feedback (light blue) and No-feedback (grey) conditions in Eitam et al., 2013, Experiments 1–3; Karsh et al., 2016, Experiments 1a, 2a, 2b; Karsh et al., 2020, Experiment 1b; and Tanaka et al., 2021, Experiment 1]. The results for the current study (clinical and sub-clinical samples) are represented in a darker hue (Box A). Across all studies, the mean RT was higher in the No-feedback condition. Box B shows the similarity in effect sizes between previous studies conducted on the general population and the current study involving individuals with MDD. Accuracy is shown in Box D, where the current findings exhibited relatively high accuracy overall, especially in the No-feedback condition. In particular, in the current study accuracy was significantly lower in the Sensorimotor-feedback condition than in the No-feedback condition. Box C presents a visual depiction of the variation in effect sizes for the differences in accuracy (Color figure online)
In addition, a fixed-effects linear regression model was employed to examine the influence of sensorimotor feedback, depression level (HRSD score), and the interaction on accuracy. The results indicated that sensorimotor feedback significantly affected accuracy (β = − .45, p < .001, BF = 513.01). Furthermore, the interaction between sensorimotor feedback and HRSD score also significantly affected accuracy (β = − .39, p = .01, BF = 5.26). Depression level (HRSD score) did not independently affect accuracy, but instead in some cases slightly improved it (β = .27, p = .08, BF = 2.8). Specifically, accuracy was lower for participants in the Sensorimotor-feedback condition (M = 0.90, SD = 0.06) compared to participants in the No-feedback condition [M = 0.95, SD = 0.03) Cohen's d = 0.99; 95% CI (0.52, 1.47)]. The interaction between sensorimotor feedback and depression was such that as severity of depression increased, participants' relative accuracy in the Sensorimotor-feedback condition decreased.
Self-reported control, motivation, and performance
In previous studies using this task (Eitam et al., 2013; Hemed et al., 2020; Karsh & Eitam, 2015a; Karsh et al., 2016, 2020), RT was not consistently correlated with any of the self-reported measures. In the present study there was a correlation between participants' self-reported perceived control over the circle (i.e., the sensory effect) and RT solely in the Sensorimotor-feedback condition (r = − .36, p = .03) as compared to the No-feedback condition (r = − .16, p = .35). No correlation was found between the other self-report measures and RT, such as wanting the sensorimotor feedback, perceived effort, or intention to perform well (see Supplementary Information).
Accuracy and self-reported control over the flashing circle were found to be negatively and moderately correlated (r = − .47, p < .001). There was also a weaker correlation between accuracy and three other self-reported measures; namely, enjoyment on the task (r = − .24, p = .04), participants' evaluation of the enjoyment others could experience when doing the same task (r = − .23, p = .04) and the urge to provoke the flashing circle (r = − .24, p = .04). However, when examining the correlations by condition, accuracy was not related to any of the self-reported variables.
Comparison of current results and previous research on the general population and a sub-clinical comparison group
Compared to our previous work, the findings in the present study suggest that the confirmation of sensorimotor predictions effectively reinforced the response execution of individuals diagnosed with MDD, and increased the vigor of their responses to a similar extent. Since this study did not include a non-MDD control group, in what follows, as a proxy, we contrast the findings to previous experiments in which we used the EMT on general (student) populations to obtain a benchmark. We also examine the performance of the participants who failed to meet the criteria for a diagnosis of MDD as a sub-clinical comparison group (see SI).
Mean RT and effect size
To better estimate the effect of sensorimotor feedback on RT in the general population and facilitate a comparison to individuals diagnosed with MDD, we conducted a meta-analysis incorporating all (8) previously published studies that have utilized the EMT in the general population. The effect sizes, represented by Cohen's d, indicated faster response times in the Sensorimotor-feedback condition than in the No-feedback condition (Fig. 6). The combined effect size and confidence interval across all eight studies [Cohen's d = 0.75; 95% CI (0.54, 0.96)] were comparable to the effect size observed in the present study in both the MDD and Subclinical groups. In fact, the effect size in the current study on MDD patients was somewhat larger [Cohen's d = 1.16; 95% CI (0.67, 1.64)]. This finding further supports the claim that confirming sensorimotor predictions (RSP) reinforces individuals with MDD by increasing their response vigor (execution speed), as effectively as in the general population (Fig. 6), if not more so.Footnote 7
Accuracy
The pattern of accuracy in the current study is consistent with previous studies that have implemented the EMT, where lower accuracy rates were found in the Sensorimotor-feedback condition (as shown in Fig. 6c, d) in 5 out of the 8 studies. While this pattern was not systematically examined in our study, the theoretical framework (Fig. 1) positing that RSP influences motor programming but not action selection suggests that this outcome was not the result of a speed-accuracy tradeoff arising from a decision process. Rather, it appears to indicate a manifestation of motor “impulsivity” attributable to an urge to respond (or the propositional learning of S–R associations; cf. Tanaka et al., 2021). Hence, our current working hypothesis is that it constitutes a second independent effect of sensorimotor feedback on responding (but see Supplementary Information).
Discussion
The current study investigated the impact of sensorimotor feedback on response vigor in individuals diagnosed with Major Depressive Disorder (MDD). Participants with MDD were asked to respond to cues using a specific keypress, where their responses either resulted in immediate and highly predictable (i.e., constant) sensorimotor feedback or no visible feedback.
As shown in this study, sensory feedback significantly boosted the speed of responding in individuals with MDD, indicating the sensitivity of response vigor to the confirmation of sensorimotor predictions. Since this effect was observed to be as strong in clinically depressed individuals as reported in the general population, our answer to the question we set out to answer is that MDD does not appear to adversely influence the modulation of response vigor in response to reinforcement, at least of the RSP type.
These findings are generally consistent with our working model (see Fig. 1; Hemed et al., 2020; Karsh et al., 2016; Karsh & Eitam, 2015a) in which RSP is based solely on the motor-system comparator model (Blakemore et al., 2001) and is not modulated by cognitions such as participants’ control-relevant knowledge or self-causal attributions (for further empirical support see Hemed et al., 2020; Karsh et al., 2016, 2020; see also, Haggard, 2005; Mir et al., 2011). The dissociation observed between cognition and reinforcement resulting from the confirmation of sensorimotor predictions may provide an explanation for the notable resilience of this particular type of reinforcement.
The present findings provide strong evidence that sensorimotor prediction remains intact in individuals with mild to moderate MDD. As such, this finding sheds light on the robustness of sensorimotor processes to damage occurring in other (reward-related) circuits of reinforcement and points to the need for future, more fine-grained studies on the interactions between reinforcement and different levels of response planning (notably, action selection and response execution) to better understand and address depressive symptoms and a-volition in general.
The nature of the motivational deficit in MDD
Building on the current understanding of the mechanism underlying the effect of confirming sensorimotor predictions as reinforcing (for the latest version of the working model, see Hemed et al., 2020), the current results localize the set of mechanisms involved in reward processing in a potentially larger system of reinforcement that does not necessarily involve rewards or desired outcomes.
Speculating further, if the brain uses a central system for reinforcing representations, then such a system may have different inputs or subsystems; for example, one that is involved in assessment of the current value of a reward/utility and an independent one that operates within the motor system (i.e., RSP). Elsewhere, we have argued that the mental representations targeted by these different inputs are also different, with the former (desired outcomes/utility) targeting choice among more abstract (action) representations and the latter targeting the choice of motor programs driving the execution of the action in a specific context and time (Hemed et al., 2020).
Based on this terminology, the current findings can be restated and integrated with the literature on disrupted reward processing which has suggested that in MDD, reinforcement leading to effective motor execution (RSP) is intact but that the ability to perform effective motor execution is underutilized or inert because the ‘upper floor’; i.e., selection between actions for maximizing the probability of obtaining desired outcomes, is damaged.
Another limitation of the current study has to do with the lack of a healthy control group. However, we do not see this as a significant issue since the current findings were considered in relation to all previous published experiments that have tested the EMT on the general population. Furthermore, the sample of sub-clinical individuals exhibited comparable effects. Although the majority of the participants in the general population samples were undergraduate students, this was not the case for the sub-clinical sample. Hence the current findings constitute a significant step toward a finer-grained description of a-volition in individuals with MDD.
Notes
This study was not preregistered; a demonstration of the task, the data and the analysis code are available at: https://osf.io/Task_demonstration_Data_and_Analysis_Code.
Although different cutoff scores on the HRSD have been used to establish the clinical level of depression (Cusin et al., 2009; Edelstein et al., 2007; Zimmerman et al., 2013) we adhered to the criteria preregistered for this randomized trial (Clinicaltrials.gov Identifier: NCT02728557). However, we also used another cutoff of HRSD > 7 for depression, based on the literature. These analyses are detailed in the Supplementary Information. Overall, the effect sizes and general patterns were insensitive to the specific cutoff chosen (see Supplementary Information).
Participants who were on medication (~ 15% of the participants) had been stable for at least three months before the start of the study and committed to maintaining that dosage for the duration of the treatment. The types and frequency of medications are detailed in the Supplementary Information.
The key results did not change when no filters were applied. See Supplementary Information for the same analyses of the unfiltered data.
In all models, all predictors were centered.
To quantify the strength of the evidence, we conducted a Bayesian linear regression using JASP (JASP Team, 2018) using the pre-set Cauchy prior (width = 0.707). Conventionally, Bayes factors between 3 and 10 are considered moderate evidence for the test hypothesis (null or alternative), and a Bayes factor of greater than 10 is considered strong evidence. When .3 < BF < 3, BF evidence is considered inconclusive (Jeffreys, 1961; Wagenmakers et al., 2018).
As shown in Fig. 6, the mean reaction time for each condition in the MDD sample (M = 470.83, SD = 52.73; M = 540.87, SD = 69.10) was higher (i.e., the responses were slower) than found in studies on the general population (M = 437.23, SD = 47.98; M = 480.48, SD = 64.57). However, there was no significant association between severity of depression, as measured by the HRSD score, and reaction time (β = 0.23, p = 0.14, BF = 0.3). Nevertheless, the Bayes factor in this analysis provides only anecdotal support for the null hypothesis of a lack of association, so that further data are needed to decisively determine whether severity of depression affects reaction time (for a review on the related topic of psycho-motor retardation, see Bennabi et al., 2013).
References
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). APA. https://doi.org/10.1176/appi.books.9780890425596
Beck, A. T., Steer, R. A., & Brown, G. K. (1996). Beck Depression Inventory (BDI-II): Manual and questionnaire. The Psychological Corporation.
Bednark, J. G., & Franz, E. A. (2014). Agency attribution: Event-related potentials and outcome monitoring. Experimental Brain Research, 232(4), 1117–1126.
Beierholm, U., Guitart-Masip, M., Economides, M., Chowdhury, R., Düzel, E., Dolan, R., & Dayan, P. (2013). Dopamine Modulates Reward-Related Vigor. Neuropsychopharmacology, 38(8), 1495–1503. https://doi.org/10.1038/npp.2013.48
Bennabi, D., Vandel, P., Papaxanthis, C., Pozzo, T., & Haffen, E. (2013). Psychomotor retardation in depression: A systematic review of diagnostic, pathophysiologic, and therapeutic implications. BioMed Research International, 2013, 158746. https://doi.org/10.1155/2013/158746
Bischof, D. (2017). New graphic schemes for Stata: Plotplain and plottig. Stata Journal, 17, 748–759.
Blakemore, S. J., Frith, C. D., & Wolpert, D. M. (2001). The cerebellum is involved in predicting the sensory consequences of action. NeuroReport, 12(9), 1879–1884.
Brown, V. J., & Bowman, E. M. (1995). Discriminative cues indicating reward magnitude continue to determine reaction time of rats following lesions of the nucleus accumbens. European Journal of Neuroscience, 7(12), 2479–2485.
Cusin, C., Yang, H., Yeung, A., & Fava, M. (2009). Rating scales for depression. In L. Baer & M. A. Blais (Eds.). Handbook of clinical rating scales and assessment in psychiatry and mental health (pp. 7–35). Humana. https://doi.org/10.1007/978-1-59745-387-5
Edelstein, B. A., Woodhead, E. L., Segal, D. L., Heisel, M. J., Bower, E. H., Lowery, A. J., & Stoner, S. A. (2007). Older adult psychological assessment: Current instrument status and related considerations. Clinical Gerontologist, 31(3), 1–35. https://doi.org/10.1080/07317110802072108
Eitam, B., Kennedy, P. M., & Higgins, E. T. (2013). Motivation from control. Experimental Brain Research, 229(3), 475–484. https://doi.org/10.1007/s00221-012-3370-7
Faul, F., Erdfelder, E., Buchner, A., & Lang, A. G. (2009). Statistical power analyses using G* Power 3.1: Tests for correlation and regression analyses. Behavior Research Methods, 41(4), 1149–1160.
Gradin, V. B., Kumar, P., Waiter, G., Ahearn, T., Stickle, C., Milders, M., Reid, I., Hall, J., & Steele, J. D. (2011). Expected value and prediction error abnormalities in depression and schizophrenia. Brain, 134(6), 1751–1764. https://doi.org/10.1093/brain/awr059
Griffiths, B., & Beierholm, U. R. (2017). Opposing effects of reward and punishment on human vigor. Scientific Reports, 7, 42287. https://doi.org/10.1038/srep42287
Haggard, P. (2005). Conscious intention and motor cognition. Trends in Cognitive Sciences, 9(6), 290–295.
Haggard, P. (2008). Human volition: Towards a neuroscience of will. Nature Reviews Neuroscience, 9(12), 934–946. https://doi.org/10.1038/nrn2497
Halahakoon, D. C., Kieslich, K., O’Driscoll, C., Nair, A., Lewis, G., & Roiser, J. P. (2020). Reward-processing behavior in depressed participants relative to healthy volunteers: A systematic review and meta-analysis. JAMA Psychiatry, 77(12), 1286–1295. https://doi.org/10.1001/jamapsychiatry.2020.2139
Hamilton, M. (1960). A rating scale for depression. Journal of Neurology, Neurosurgery, and Psychiatry, 23(1), 56.
Hemed, E., Bakbani-Elkayam, S., Teodorescu, A. R., Yona, L., & Eitam, B. (2020). Evaluation of an action’s effectiveness by the motor system in a dynamic environment [Clarification Notice: A clarification for this article was reported in Vol. 152(3) of Journal of Experimental Psychology: General (see record 2023-63989–001)]. Journal of Experimental Psychology: General, 149(5), 935.
Hemed, E., Karsh, N., Mark-Tavger, I., & Eitam, B. (2022). Motivation (s) from control: Response-effect contingency and confirmation of sensorimotor predictions reinforce different levels of selection. Experimental Brain Research, 240(5), 1471–1497.
Husain, M., & Roiser, J. P. (2018). Neuroscience of apathy and anhedonia: A transdiagnostic approach. Nature Reviews Neuroscience, 19(8), 470–484.
Huys, Q. J., Pizzagalli, D. A., Bogdan, R., & Dayan, P. (2013). Mapping anhedonia onto reinforcement learning: A behavioural meta-analysis. Biology of Mood and Anxiety Disorders, 3(1), 1–16. https://doi.org/10.1186/2045-5380-3-12
JASP Team. (2018). JASP (Version 0.8. 6). JASP Team.
Jeffreys, H. (1961). Theory of probability (3rd ed.). Oxford University Press.
Karsh, N., & Eitam, B. (2015a). I control therefore I do: Judgments of agency influence action selection. Cognition, 138, 122–131. https://doi.org/10.1016/j.cognition.2015.02.002
Karsh, N., & Eitam, B. (2015b). Motivation from control: A response selection framework. Oxford University Press.
Karsh, N., Eitam, B., Mark, I., & Higgins, E. T. (2016). Bootstrapping agency: How control-relevant information affects motivation. Journal of Experimental Psychology: General, 145(10), 1333.
Karsh, N., Haklay, I., Raijman, N., Lampel, A., & Custers, R. (2021). Control alters risk-taking: The motivating impact of action-effectiveness in different risk contexts. Motivation Science, 7(4), 475.
Karsh, N., Hemed, E., Nafcha, O., Elkayam, S. B., Custers, R., & Eitam, B. (2020). The differential impact of a response’s effectiveness and its monetary value on response-selection. Scientific Reports, 10(1), 1–12. https://doi.org/10.1038/s41598-020-60385-9
Kessler, R. C., Demler, O., Frank, R. G., Olfson, M., Pincus, H. A., Walters, E. E., Wang, P., Wells, K. B., & Zaslavsky, A. M. (2005). Prevalence and Treatment of Mental Disorders, 1990 to 2003. New England Journal of Medicine, 352(24), 2515-2523. https://doi.org/10.1056/NEJMsa043266
Knutson, B., Westdorp, A., Kaiser, E., & Hommer, D. (2000). FMRI visualization of brain activity during a monetary incentive delay task. NeuroImage, 12, 20–27. https://doi.org/10.1006/nimg.2000.0593
Manohar, S. G., Finzi, R. D., Drew, D., & Husain, M. (2017). Distinct Motivational Effects of Contingent and Noncontingent Rewards. Psychological Science, 28(7), 1016-1026. https://doi.org/10.1177/0956797617693326
Mir, P., Trender-Gerhard, I., Edwards, M. J., Schneider, S. A., Bhatia, K. P., & Jahanshahi, M. (2011). Motivation and movement: The effect of monetary incentive on performance speed. Experimental Brain Research, 209(4), 551–559.
Moutoussis, M., Rutledge, R. B., Prabhu, G., Hrynkiewicz, L., Lam, J., Ousdal, O. T., Guitart-Masip, M., Fonagy, P., & Dolan, R. J. (2018). Neural activity and fundamental learning, motivated by monetary loss and reward, are intact in mild to moderate major depressive disorder. PLoS ONE, 13(8), 1–20. https://doi.org/10.1371/journal.pone.0201451
National Institute of Mental Health. (2011). Definitions of the RDoC domains and constructs. National Institute of Mental Health. https://www.nimh.nih.gov/research/research-funded-by-nimh/rdoc/definitions-of-the-rdoc-domains-and-constructs
Olino, T. M. (2016). Future research directions in the positive valence systems: Measurement, development, and implications for youth unipolar depression. Journal of Clinical Child and Adolescent Psychology, 45(5), 681–705. https://doi.org/10.1080/15374416.2015.1118694
Penton, T., Wang, X., Coll, M. P., Catmur, C., & Bird, G. (2018). The influence of action-outcome contingency on motivation from control. Experimental Brain Research, 236(12), 3239–3249.
Pizzagalli, D. A., Iosifescu, D., Hallett, L. A., Ratner, K. G., & Fava, M. (2008). Reduced hedonic capacity in major depressive disorder: Evidence from a probabilistic reward task. Journal of Psychiatric Research, 43(1), 76–87. https://doi.org/10.1016/j.jpsychires.2008.03.001
Proudfit, G. H. (2015). The reward positivity: From basic research on reward to a biomarker for depression. Psychophysiology, 52(4), 449–459. https://doi.org/10.1111/psyp.12370
Pullman, S. L., Watts, R. L., Juncos, J. L., Chase, T. N., & Sanes, J. N. (1988). Dopaminergic effects on simple and choice reaction time performance in Parkinson’s disease. Neurology, 38(2), 249.
Rothkirch, M., Tonn, J., Köhler, S., & Sterzer, P. (2017). Neural mechanisms of reinforcement learning in unmedicated patients with major depressive disorder. Brain, 140(4), 1147–1157. https://doi.org/10.1093/brain/awx025
Sheehan, D. V., Lecrubier, Y., Sheehan, K. H., Amorim, P., Janavs, J., Weiller, E., Hergueta, T., Baker, R., & Dunbar, G. C. (1998). The Mini-International Neuropsychiatric Interview (MINI): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. Journal of Clinical Psychiatry, 59(20), 22–33.
StataCorp. (2019). Stata statistical software: Release 16. StataCorp LLC.
Tanaka, T., Watanabe, K., & Tanaka, K. (2021). Immediate action effects motivate actions based on the stimulus–response relationship. Experimental Brain Research, 239(1), 67–78.
Wagenmakers, E. J., Love, J., Marsman, M., Jamil, T., Ly, A., Verhagen, J., Selker, R., Gronau, Q. F., Dropmann, D., & Boutin, B. (2018). Bayesian inference for psychology. Part II: Example applications with JASP. Psychonomic Bulletin and Review, 25(1), 58–76.
Waskom, M. L. (2021). Seaborn: Statistical data visualization. Journal of Open Source Software, 6(60), 3021. https://doi.org/10.21105/joss.03021
Wen, W., & Imamizu, H. (2022). The sense of agency in perception, behaviour and human–machine interactions. Nature Reviews Psychology, 1, 1–12.
Wen, W., Minohara, R., Hamasaki, S., Maeda, T., An, Q., Tamura, Y., Yamakawa, H., Yamashita, A., & Asama, H. (2018). The readiness potential reflects the reliability of action consequence. Scientific Reports, 8(1), 1–5. https://doi.org/10.1038/s41598-018-30410-z
Winter, N. R., Leenings, R., Ernsting, J., Sarink, K., Fisch, L., Emden, D., Blanke, J., Goltermann, J., Opel, N., Barkhau, C., Meinert, S., Dohm, K., Repple, J., Mauritz, M., Gruber, M., Leehr, E. J., Grotegerd, D., Redlich, R., Jansen, A., …, Hahn, T. (2021). More alike than different: Quantifying deviations of brain structure and function in major depressive disorder across neuroimaging modalities. http://arxiv.org/abs/2112.10730
World Health Organization. (2017). Depression and other common mental disorders: Global health estimates. WHO. https://apps.who.int/iris/handle/10665/254610
Zilcha-Mano, S., Dolev, T., Leibovich, L., & Barber, J. P. (2018). Identifying the most suitable treatment for depression based on patients’ attachment: Study protocol for a randomized controlled trial of supportive–expressive vs. supportive treatments. BMC Psychiatry, 18, 1–9.
Zilcha-Mano, S., Goldstein, P., Dolev-Amit, T., Ben David-Sela, T., & Barber, J. P. (2021). A randomized controlled trial for identifying the most suitable treatment for depression based on patients’ attachment orientation. Journal of Consulting and Clinical Psychology, 89(12), 985.
Zimmerman, M., Martinez, J. H., Young, D., Chelminski, I., & Dalrymple, K. (2013). Severity classification on the Hamilton depression rating scale. Journal of Affective Disorders, 150(2), 384–388. https://doi.org/10.1016/j.jad.2013.04.028
Acknowledgements
This work was partially supported by the Israel Science Foundation (ISF Grant No. 118 15 to S. Zilcha-Mano; ISF Grant No. 339/16 to B. Eitam), The Bi-national Science Foundation (BSF Grant Number 2016299 to B. Eitam) and an Azrieli Foundation Award (to S. Bakbani-Elkayam).
Funding
Open access funding provided by University of Haifa.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
We have no known conflict of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bakbani-Elkayam, S., Dolev-Amit, T., Hemed, E. et al. Intact modulation of response vigor in major depressive disorder. Motiv Emot 48, 209–221 (2024). https://doi.org/10.1007/s11031-024-10059-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11031-024-10059-0