Abstract
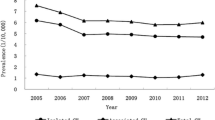
Congenital hydrocephalus (CH) was a major birth defect of the central nervous system besides neural tube defects (NTDs). Few studies have focused on both the prevalence and trend of isolated and complicated CH in China. Data were drawn from a population-based birth defects surveillance program in five rural counties in northern China from 2005 to 2015. All livebirths and pregnancy terminations at any gestational age affected with CH were recorded. The prevalence and trend of isolated and complicated CH were examined. During the 11-year period, a total of 176,223 births and 357 CH cases were recorded, resulting in a prevalence rate of 20.3 CH cases per 10,000 births. Of the CH cases, 146 were isolated CH, resulting in a prevalence rate of 8.3 per 10,000 births. The pre-perinatal prevalence (<28 gestational weeks) was higher than the perinatal prevalence for both isolated and total CH. The prevalence rates of total and isolated CH showed a similar downward trend during the 11–year period. This downward trend was statistically significant after 2009 (p < 0.05), when a massive folic acid supplementation program was introduced. Although it decreased over time, the prevalence of CH remains high in this population which has a high prevalence of neural tube defects.

Similar content being viewed by others
References
Adeloye A, Warkany J (1976) Experimental congenital hydrocephalus. A review with special consideration of hydrocephalus produced by zinc deficiency. Childs Brain 2:325–360
Cains S, Shepherd A, Nabiuni M, Owen-Lynch PJ, Miyan J (2009) Addressing a folate imbalance in fetal cerebrospinal fluid can decrease the incidence of congenital hydrocephalus. J Neuropathol Exp Neurol 68:404–416. https://doi.org/10.1097/NEN.0b013e31819e64a7
Dai L, Zhou GX, Miao L, Zhu J, Wang YP, Liang J (2006) Prevalence analysis on congenital hydrocephalus in Chinese perinatal from 1996 to 2004. Zhonghua Yu Fang Yi Xue Za Zhi 40:180–183
Dreha-Kulaczewski S, Joseph AA, Merboldt KD, Ludwig HC, Gartner J, Frahm J (2017) Identification of the Upward Movement of Human CSF In Vivo and its Relation to the Brain Venous System. J Neurosci 37:2395–2402. https://doi.org/10.1523/JNEUROSCI.2754-16.2017
Eke CB, Uche EO, Chinawa JM, Obi IE, Obu HA, Ibekwe RC (2016) Epidemiology of congenital anomalies of the central nervous system in children in Enugu, Nigeria: A retrospective study. Ann Afr Med 15:126–132. https://doi.org/10.4103/1596-3519.188892
Fan L, Gong T, Cao X, Du Y (2013) Epidemiologic characteristics of birth defects in the Hainan Province from 2000 to 2010, China. Birth Defects Res A Clin Mol Teratol 97:750–754. https://doi.org/10.1002/bdra.23148
Garne E, Loane M, Addor MC, Boyd PA, Barisic I, Dolk H (2010) Congenital hydrocephalus--prevalence, prenatal diagnosis and outcome of pregnancy in four European regions. Eur J Paediatr Neurol 14:150–155. https://doi.org/10.1016/j.ejpn.2009.03.005
Goh YI, Bollano E, Einarson TR, Koren G (2006) Prenatal multivitamin supplementation and rates of congenital anomalies: a meta-analysis. J Obstet Gynaecol Can 28:680–689
Gu X et al (2007) High prevalence of NTDs in Shanxi Province: a combined epidemiological approach. Birth Defects Res A Clin Mol Teratol 79:702–707. https://doi.org/10.1002/bdra.20397
Jeng S, Gupta N, Wrensch M, Zhao S, Wu YW (2011) Prevalence of congenital hydrocephalus in California, 1991-2000. Pediatr Neurol 45:67–71. https://doi.org/10.1016/j.pediatrneurol.2011.03.009
Jin L, Jin L, Yu J, Xu Y, Liu H, Ren A (2017) Prevalence of Neural Tube Defects and the Impact of Prenatal Diagnosis in Three Districts of Beijing, China. Paediatr Perinat Epidemiol. https://doi.org/10.1111/ppe.12354
Li Z et al (2006) Extremely high prevalence of neural tube defects in a 4-county area in Shanxi Province, China. Birth Defects Res A Clin Mol Teratol 76:237–240. https://doi.org/10.1002/bdra.20248
Lim H, Agopian AJ, Whitehead LW, Beasley CW, Langlois PH, Emery RJ, Waller DK (2015) Maternal occupational exposure to ionizing radiation and major structural birth defects. Birth Defects Res A Clin Mol Teratol 103:243–254. https://doi.org/10.1002/bdra.23340
Lindquist B, Persson EK, Fernell E, Uvebrant P (2011) Very long-term follow-up of cognitive function in adults treated in infancy for hydrocephalus. Childs Nerv Syst 27:597–601. https://doi.org/10.1007/s00381-010-1311-y
Liu J et al (2016a) Prevalence and trend of neural tube defects in five counties in Shanxi province of Northern China, 2000 to 2014. Birth Defects Res A Clin Mol Teratol 106:267–274. https://doi.org/10.1002/bdra.23486
Liu QG, Sun J, Xiao XW, Song GR (2016b) Birth defects data from surveillance hospitals in Dalian city, China, 2006-2010. J Matern Fetal Neonatal Med 29:3615–3621. https://doi.org/10.3109/14767058.2016.1140136
Ma R, Wang L (2017) Plasma folate levels and associated factors in women planning to become pregnant in a population with high prevalence of neural tube defects. Birth Defects Res A Clin Mol Teratol. https://doi.org/10.1002/bdr2.1040
Ministry of Health C (2012) China birth defects prevention report (2012). Available from: http://www.gov.cn/gzdt/2012-09/12/content_2223371.htm. Accessed 4 Dec 2017
Moritake K, Nagai H, Miyazaki T, Nagasako N, Yamasaki M, Tamakoshi A (2007) Nationwide survey of the etiology and associated conditions of prenatally and postnatally diagnosed congenital hydrocephalus in Japan. Neurol Med Chir (Tokyo) 47:448–452 discussion 452
Munch TN, Rostgaard K, Rasmussen ML, Wohlfahrt J, Juhler M, Melbye M (2012) Familial aggregation of congenital hydrocephalus in a nationwide cohort. Brain 135:2409–2415. https://doi.org/10.1093/brain/aws158
Naz N, Jimenez AR, Sanjuan-Vilaplana A, Gurney M, Miyan J (2016) Neonatal hydrocephalus is a result of a block in folate handling and metabolism involving 10-formyltetrahydrofolate dehydrogenase. J Neurochem 138:610–623. https://doi.org/10.1111/jnc.13686
O'Dell BL, Whitley JR, Hogan AG (1948) Relation of folic acid and vitamin A to incidence of hydrocephalus in infant rats. Proc Soc Exp Biol Med 69:272–275
Qian L et al (2017) Analysis of epidemiological trends in human papillomavirus infection among gynaecological outpatients in Hangzhou, China, 2011-2015. BMC Infect Dis 17:393. https://doi.org/10.1186/s12879-017-2498-2
Ren AG (2015) Prevention of neural tube defects with folic acid: The Chinese experience. World J Clin Pediatr 4:41–44. https://doi.org/10.5409/wjcp.v4.i3.41
Santos MM et al (2017) Infant hydrocephalus in sub-Saharan Africa: the reality on the Tanzanian side of the lake. J Neurosurg Pediatr 20:423–431. https://doi.org/10.3171/2017.5.peds1755
Sun G, Xu ZM, Liang JF, Li L, Tang DX (2011) Twelve-year prevalence of common neonatal congenital malformations in Zhejiang Province, China. World J Pediatr 7:331–336. https://doi.org/10.1007/s12519-011-0328-y
Walsh S, Donnan J, Morrissey A, Sikora L, Bowen S, Collins K, MacDonald D (2016) A systematic review of the risks factors associated with the onset and natural progression of hydrocephalus. Neurotoxicology. https://doi.org/10.1016/j.neuro.2016.03.012
Wilson RD et al (2007) Pre-conceptional vitamin/folic acid supplementation 2007: the use of folic acid in combination with a multivitamin supplement for the prevention of neural tube defects and other congenital anomalies. J Obstet Gynaecol Can 29:1003–1026
Woodard JC, Newberne PM (1966) Relation of vitamin B12 and one-carbon metabolism to hydrocephalus in the rat. J Nutr 88:375–381
Woodward JC, Newberne PM (1967) The pathogenesis of hydrocephalus in newborn rats deficient in vitamin B12. J Embryol Exp Morpholog 17:177–187
Xie D, Yang T, Liu Z, Wang H (2016) Epidemiology of Birth Defects Based on a Birth Defect Surveillance System from 2005 to 2014 in Hunan Province, China. PLoS One 11:e0147280. https://doi.org/10.1371/journal.pone.0147280
Yang W, Zeng L, Cheng Y, Chen Z, Wang X, Li X, Yan H (2012) The effects of periconceptional risk factor exposure and micronutrient supplementation on birth defects in Shaanxi Province in Western China. PLoS One 7:e53429. https://doi.org/10.1371/journal.pone.0053429
Zhang X et al (2012) Prevalence of birth defects and risk-factor analysis from a population-based survey in Inner Mongolia, China. BMC Pediatr 12:125. https://doi.org/10.1186/1471-2431-12-125
Zhang TN et al (2017) Time trends in the prevalence and epidemiological characteristics of neural tube defects in Liaoning Province, China, 2006-2015: A population-based study. Oncotarget 8:17092–17104. https://doi.org/10.18632/oncotarget.15060
Funding
This work was supported in part by the National Key Research and Development Program, Ministry of Science and Technology, P.R. China (grant No. 2016YFC1000500) and the National Natural Science Foundation of China (Grant Numbers: 81202265).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None declared.
Rights and permissions
About this article
Cite this article
Liu, J., Jin, L., Li, Z. et al. Prevalence and trend of isolated and complicated congenital hydrocephalus and preventive effect of folic acid in northern China, 2005–2015. Metab Brain Dis 33, 837–842 (2018). https://doi.org/10.1007/s11011-017-0172-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11011-017-0172-4