Abstract
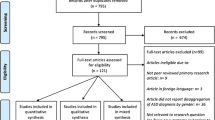
Although the etiology and pathology of autism spectrum disorder (ASD) is still poorly understood, a number of environmental, anthropological, neurobiological and genetic factors have been related to the pathophysiology of ASD, even the impact of oxidative stress response related to the environment and nutrition intake. Usual recommended dietary habits are based on the combination of behavioral and dietary or nutraceutical interventions together with pharmacotherapy. Investigations about a reliable relationship between diet and ASD are still lacking. The present study aimed at comparing dietary regimens and habits of normally developing apparently healthy children, without diagnosed ASD, with a pediatric population of individuals affected by autistic disorder. Assessments of nutritional and anthropometric data, in addition to biochemical evaluation for nutrient deficiencies, were performed. A total of 80 children with autistic disorder and 80 healthy, normally developing pediatric individuals were enrolled in the study. Parents were asked to complete the standardized questionnaire regarding the different types of food and the proportion of a serving for their children. Biochemical analysis of micro- and macronutrients were also done. Plotting on the Egyptian sex-specific anthropometric growth (auximetric) chart, absolute weights as well as weight-related for age classes, were significantly higher in cases than healthy controls. No differences between groups were observed in regard to total kilocalories (kcal), carbohydrates, and fat intake. A total of 23.8% of children with autistic disorder vs. 11.3% in the healthy control group had a nutrient intake with features below the Recommended Dietary Allowance (RDA) of protein. Children with autistic disorder showed low dietary intake of some micronutrients; calcium (Ca), magnesium (Mg), iron (Fe), selenium (Se) and sodium (Na), also they had significantly high intake of potassium (K) and vitamin C compared to healthy controls. Serum Mg, Fe, Ca, folate and vitamin B12 in children with autistic disorder were significantly low compared with healthy children. Significant positive correlations between serum Mg, Fe, Ca, vitamin B12 and folate and their levels in food were present. These results confirmed that different nutritional inadequacy was observed in Egyptian children with autistic disorder. The evidence reported in the present study should recommend screening of the nutritional status of ASD children for nutrient adequacy to reduce these deficiencies by dietary means or by administering appropriate vitamin and mineral supplements. Nutritional intervention plan should be tailored to address specific needs.






Similar content being viewed by others
References
Adams JB, Holloway C (2004) Pilot study of a moderate dose multivitamin/mineral supplement for children with autistic spectrum disorder. J Altern Complement Med 10:1033–1039
Al-Farsi YM, Waly MI, Al-Sharbati MM, Al-Shafaee MA, Al-Farsi OA, Al-Khaduri MM, Gupta I, Ouhtit A, Al-Adawi S, Al-Said MF, Deth RC (2013a) Levels of heavy metals and essential minerals in hair samples of children with autism in Oman: a case-control study. Biol Trace Elem Res 151:181–186
Al-Farsi YM, Waly MI, Deth RC, Al-Sharbati MM, Al-Shafaee M, Al-Farsi O, Al-Khaduri MM, Al-Adawi S, Hodgson NW, Gupta I, Ouhtit A (2013b) Impact of nutrition on serum levels of docosahexaenoic acid among Omani children with autism. Nutrition 29:1142–1146
Ali A, Waly MI, Al-Farsi YM, Essa MM, Al-Sharbati MM, Deth RC (2011) Hyperhomocysteinemia among Omani autistic children: a case-control study. Acta Biochim Pol 58:547–551
APA - American Psychiatric Association (2000) Diagnostic and statistical manual of mental disorders: DSM-IV-TR. American Psychiatric Association, Washington, DC
APA - American Psychiatric Association (2013) Diagnostic and statistical manual of mental disorders: DSM-5. American Psychiatric Association Publishing, Arlington
Atkinson SA (2011) The new dietary reference intakes from the Institute of Medicine for calcium and vitamin D (in French). Perspect Infirm 8:5
Bandini LG, Anderson SE, Curtin C, Cermak S, Evans EW, Scampini R, Maslin M, Must A (2010) Food selectivity in children with autism spectrum disorders and typically developing children. J Pediatr 157:259–264
Bertrand J, Mars A, Boyle C, Bove F, Yeargin-Allsopp M, Decoufle P (2001) Prevalence of autism in a United States population. Pediatrics 108:1155–1161
Bilgiç A, Gürkan K, Türkoğlu S, Akça AF, Kılıç BG, Uslu R (2010) Iron deficiency in preschool children with autistic spectrum disorders. Res Autism Spectr Disord 4:639–644
Bjørklund G (1998) Children with Asperger syndrome (in Norwegian). Tidsskr Nor Laegeforen 118:1567–1569
Bjørklund G (2013) The role of zinc and copper in autism spectrum disorders. Acta Neurobiol Exp 73:225–236
Bjørklund G, Chartrand M (2016) Nutritional and environmental influences on autism spectrum disorder. J Nutr Disorders The 6:e123. doi:10.4172/2161-0509.1000e123
Böckerman P, Bryson A, Viinikainen J, Viikari J, Lehtimäki T, Vuori E, Keltikangas-Järvinen L, Raitakari O, Pehkonen J (2015) The serum copper/zinc ratio in childhood and educational attainment: a population-based study. J Public Health (Oxf). doi:10.1093/pubmed/fdv187
Cermak SA, Curtin C, Bandini LG (2010) Food selectivity and sensory sensitivity in children with autism spectrum disorders. J Am Diet Assoc 110:238–246
Cornish E (1998) A balanced approach towards healthy eating in autism. J Hum Nutr Diet 11:501–509
Cornish J, Callon KE, King AR, Cooper GJ, Reid IR (1998) Systemic administration of amylin increases bone mass, linear growth, and adiposity in adult male mice. Am J Physiol 275:E694–E699
Crăciun EC, Bjørklund G, Tinkov AA, Urbina MA, Skalny AV, Rad F, Dronca E (2016) Evaluation of whole blood zinc and copper levels in children with autism spectrum disorder. Metab Brain Dis 31:887–890
de Onis M, Onyango AW, Van den Broeck J, Chumlea WC, Martorell R (2004) Measurement and standardization protocols for anthropometry used in the construction of a new international growth reference. Food Nutr Bull 25:S27–S36
Dosman CF, Drmic IE, Brian JA (2006) Ferritin as an indicator of suspected iron deficiency in children with autism spectrum disorder: prevalence of low serum ferritin concentration. Dev Med Child Neurol 48:1008–1009
Dosman CF, Brian JA, Drmic IE, Senthilselvan A, Harford MM, Smith RW, Sharieff W, Zlotkin SH, Moldofsky H, Roberts SW (2007) Children with autism: effect of iron supplementation on sleep and ferritin. Pediatr Neurol 36:152–158
Emond A, Emmett P, Steer C, Golding J (2010) Feeding symptoms, dietary patterns, and growth in young children with autism spectrum disorders. Pediatrics 126:e337–e342. doi:10.1542/peds.2009-2391
Endreffy I, Bjørklund G, Dicső F, Urbina MA, Endreffy E (2016) Acid glycosaminoglycan (aGAG) excretion is increased in children with autism spectrum disorder, and it can be controlled by diet. Metab Brain Dis 31:273–278
Faber S, Zinn GM, Kern JC 2nd, Kingston HM (2009) The plasma zinc/serum copper ratio as a biomarker in children with autism spectrum disorders. Biomarkers 14:171–180
FAO/WHO (2002) Human vitamin and mineral requirements: report of a joint FAO/WHO expert consultation Bangkok, Thailand. Food and Agriculture Organization of the United Nations, Rome
FAO/WHO/UNU (2004) Human energy requirements. Report of a joint FAO/WHO/UNU expert consultation. FAO food and nutrition technical report series, no. 1. Food and Agriculture Organization of the United Nations, Rome
Fulgoni VL 3rd (2007) Limitations of data on fluid intake. J Am Coll Nutr 26(5 Suppl):588S–591S
Graf-Myles J, Farmer C, Thurm A, Royster C, Kahn P, Soskey L, Rothschild L, Swedo S (2013) Dietary adequacy of children with autism compared with controls and the impact of restricted diet. J Dev Behav Pediatr 34:449–459
Han Y, Xi QQ, Dai W, Yang SH, Gao L, Su YY, Zhang X (2015) Abnormal transsulfuration metabolism and reduced antioxidant capacity in Chinese children with autism spectrum disorders. Int J Dev Neurosci 46:27–32
Herndon AC, DiGuiseppi C, Johnson SL, Leiferman J, Reynolds A (2009) Does nutritional intake differ between children with autism spectrum disorders and children with typical development? J Autism Dev Disord 39:212–222
Hjiej H, Doyen C, Couprie C, Kaye K, Contejean Y (2008) Substitutive and dietetic approaches in childhood autistic disorder: interests and limits. L'Encéphale 34(5):496–503
Horvath K, Perman JA (2002) Autism and gastrointestinal symptoms. Curr Gastroenterol Rep 4:251–258
Hyman SL, Stewart PA, Schmidt B, Cain U, Lemcke N, Foley JT, Peck R, Clemons T, Reynolds A, Johnson C, Handen B, James SJ, Courtney PM, Molloy C, Ng PK (2012) Nutrient intake from food in children with autism. Pediatrics 130:S145–S153
IOM - Institute of Medicine (US) Panel on Dietary Antioxidants and Related Compounds (2000) Dietary reference intakes for vitamin C, vitamin E, selenium, and carotenoids. National Academies Press, Washington
IOM - Institute of Medicine (US) Panel on Micronutrients (2001) Dietary reference intakes for vitamin a, vitamin K, arsenic, boron, chromium, copper, iodine, iron, manganese, molybdenum, nickel, silicon, vanadium, and zinc. National Academies Press, Washington
IOM - Institute of Medicine (US) Standing Committee on the Scientific Evaluation of Dietary Reference Intakes (1997) Dietary reference intakes for calcium, phosphorus, magnesium, vitamin D, and fluoride. National Academies Press, Washington
IOM - Institute of Medicine (US) Standing Committee on the Scientific Evaluation of Dietary Reference Intakes and its Panel on Folate, Other B Vitamins, and Choline (1998) Dietary reference intakes for thiamin, riboflavin, niacin, vitamin B6, folate, vitamin B12, pantothenic acid, biotin, and choline. National Academies Press, Washington
Johnson CR, Handen BL, Mayer-Costa M, Sacco K (2008) Eating habits and dietary status in young children with autism. J Dev Phys Disabil 20:437–448
Li SO, Wang JL, Bjørklund G, Zhao WN, Yin CH (2014) Serum copper and zinc levels in individuals with autism spectrum disorders. Neuroreport 25:1216–1220
Lindsay RL, Eugene Arnold L, Aman MG, Vitiello B, Posey DJ, McDougle CJ, Scahill L, Pachler M, McCracken JT, Tierney E, Bozzolo D (2006) Dietary status and impact of risperidone on nutritional balance in children with autism: a pilot study. J Intellect Develop Disabil 31:204–209
Lockner DW, Crowe TK, Skipper BJ (2008) Dietary intake and parents’ perception of mealtime behaviors in preschool-age children with autism spectrum disorder and in typically developing children. J Am Diet Assoc 108:1360–1363
Luna RA, Savidge TC, Williams KC (2016) The brain-gut-microbiome axis: what role does it play in autism spectrum disorder? Curr Dev Disord Rep 3:75–81
Macedoni-Lukšič M, Gosar D, Bjørklund G, Oražem J, Kodrič J, Lešnik-Musek P, Zupančič M, France-Štiglic A, Sešek-Briški A, Neubauer D, Osredkar J (2015) Levels of metals in the blood and specific porphyrins in the urine in children with autism spectrum disorders. Biol Trace Elem Res 163:2–10
Mandy W, Lai MC (2016) Annual research review: the role of the environment in the developmental psychopathology of autism spectrum condition. J Child Psychol Psychiatry 57:271–292
Marshall WA, Tanner JM (1969) Variations in pattern of pubertal changes in girls. Arch Dis Child 44:291–303
Marshall WA, Tanner JM (1970) Variations in the pattern of pubertal changes in boys. Arch Dis Child 45:13–23
Meguid NA, Hashish AF, Anwar M, Sidhom G (2010) Reduced serum levels of 25-hydroxy and 1,25-dihydroxy vitamin D in Egyptian children with autism. J Altern Complement Med 16:641–645
Meguid N, Anwar M, Zaki S, Kandeel W, Ahmed N, Tewfik I (2015) Dietary patterns of children with autism spectrum disorder: a study based in Egypt. Open Access Maced J Med Sci 3:262–267
Molloy CA, Manning-Courtney P (2003) Prevalence of chronic gastrointestinal symptoms in children with autism and autistic spectrum disorders. Autism 7:165–171
Palmieri L, Papaleo V, Porcelli V, Scarcia P, Gaita L, Sacco R, Hager J, Rousseau F, Curatolo P, Manzi B, Militerni R, Bravaccio C, Trillo S, Schneider C, Melmed R, Elia M, Lenti C, Saccani M, Pascucci T, Puglisi-Allegra S, Reichelt KL, Persico AM (2010) Altered calcium homeostasis in autism-spectrum disorders: evidence from biochemical and genetic studies of the mitochondrial aspartate/glutamate carrier AGC1. Mol Psychiatry 15:38–52
Rutter M, Le CA, Lord C (2003) Autism diagnostic interview-revised (ADI-R). Western Psychological Services, Los Angeles
Santocchi E, Guiducci L, Fulceri F, Billeci L, Buzzigoli E, Apicella F, Calderoni S, Grossi E, Morales MA, Muratori F (2016) Gut to brain interaction in autism spectrum disorders: a randomized controlled trial on the role of probiotics on clinical, biochemical and neurophysiological parameters. BMC Psychiatry 16:183–185
Schopler E, Reichler RJ, Rochen-Renner B (1998) The childhood autism rating scale (CARS). Western Psychological Services, Los Angeles
Shearer TR, Larson K, Neuschwander J, Gedney B (1982) Minerals in the hair and nutrient intake of autistic children. J Autism Dev Disord 12:25–34
Sidrak S, Yoong T, Woolfenden S (2014) Iron deficiency in children with global developmental delay and autism spectrum disorder. J Paediatr Child Health 50:356–361
Siu AL, Bibbins-Domingo K, Grossman DC, Baumann LC, Davidson KW, Ebell M, García FA, Gillman M, Herzstein J, Kemper AR, Krist AH, Kurth AE, Owens DK, Phillips WR, Phipps MG, Pignone MP (2016) Screening for autism Spectrum disorder in young children: US preventive services task force recommendation statement. JAMA 315:691–696
Skalny AV, Skalnaya MG, Bjørklund G, Nikonorov AA, Tinkov AA (2016) Mercury as a possible link between maternal obesity and autism spectrum disorder. Med Hypotheses 91:90–94
Soden SE, Garrison CB, Egan AM, Beckwith AM (2012) Nutrition, physical activity, and bone mineral density in youth with autistic spectrum disorders. J Dev Behav Pediatr 33:618–624
Stewart C, Latif A (2008) Symptomatic nutritional rickets in a teenager with autistic spectrum disorder. Child Care Health Dev 34:276–278
Strambi M, Longini M, Hayek J, Berni S, Macucci F, Scalacci E, Vezzosi P (2006) Magnesium profile in autism. Biol Trace Elem Res 109:97–104
Sun C, Xia W, Zhao Y, Li N, Zhao D, Wu L (2013) Nutritional status survey of children with autism and typically developing children aged 4-6 years in Heilongjiang Province, China. J Nutr Sci 2:e16. doi:10.1017/jns.2013.9
Whiteley P (2004) Developmental, behavioural and somatic factors in pervasive developmental disorders: preliminary analysis. Child Care Health Dev 30:5–11
WHO - World Health Organization (2008) Training course on child growth assessment, WHO child growth standards. B: measuring a child’s growth. World Health Organization, Geneva
WHO - World Health Organization (2009) WHO Anthro for personal computers, version 3.01: software for assessing growth and development of the world’s children. World Health Organization, Geneva
Xia W, Zhou Y, Sun C, Wang J, Wu L (2010) A preliminary study on nutritional status and intake in Chinese children with autism. Eur J Pediatr 169:1201–1206. doi:10.1007/s00431-010-1203-x
Zablotsky B, Black LI, Maenner MJ, Schieve LA, Blumberg SJ (2015) Estimated prevalence of autism and other developmental disabilities following questionnaire changes in the 2014 National Health Interview Survey. Natl Health Stat Rep 87:1–20
Zimmer MH, Hart LC, Manning-Courtney P, Murray DS, Bing NM, Summer S (2012) Food variety as a predictor of nutritional status among children with autism. J Autism Dev Disord 42:549–556
Acknowledgements
This research project was supported by the Science and Technology Development Fund in Egypt (STDF) for Dr. Nagwa Abdel Meguid, project number 5541.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no potential conflicts of interest with respect to the authorship, and/or publication of this article.
Ethical approval
All procedures performed were in accordance with the ethical standards of the institutional and/or national research committee, and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Rights and permissions
About this article
Cite this article
Meguid, N.A., Anwar, M., Bjørklund, G. et al. Dietary adequacy of Egyptian children with autism spectrum disorder compared to healthy developing children. Metab Brain Dis 32, 607–615 (2017). https://doi.org/10.1007/s11011-016-9948-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11011-016-9948-1