Abstract
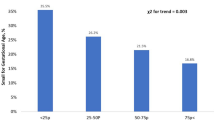
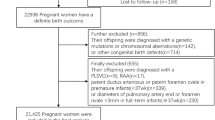
Maternal hypercholesterolemia (MHC) during pregnancy is associated with the risk of developing aortic lesions in fetuses. There is also a possibility of faster progression of atherosclerosis in offspring born to hypercholesterolemic mothers (HCM) during their adulthood. We investigated whether elevated maternal cholesterol levels during pregnancy influence the lipid levels in offspring. We analyzed the lipid profile of mothers during the three trimesters, cord blood (CB) at birth, and neonatal blood (NB) on Day 2 postpartum in the offspring. Cholesterol levels of HCM significantly increased throughout gestation when compared to normocholesterolemic mothers (NCM). CB lipid levels of newborns of HCM were similar to the newborns of NCM. While NB of offspring of HCM had elevated levels of triglycerides (TG) (p < 0.01) and very low-density lipoprotein (VLDL) (p < 0.01) when compared to the offspring of NCM. MHC also resulted in low newborn birthweight (p < 0.05) and low placental efficiency (ratio of newborn birth weight to placental weight) (p < 0.01) but no change was observed in umbilical cord length or placental weight. Immunohistochemical analysis revealed no significant changes in the protein expression of genes involved in TG metabolisms such as LDLR, VLDLR, CETP, and PPARG. We report that MHC in mothers decreases placental efficiency and newborn birthweight while increasing lipid levels in neonates on the second postpartum day. Given that TG levels modulate the circulating Low-Density lipoproteins, the increase in these levels in neonates gains importance. Whether these consistently high levels cause atherosclerosis in early adulthood warrants further investigation.




Similar content being viewed by others
Data availability
All data generated or analyzed during this study are included in this article. Raw files and additional information may be available by the corresponding author upon reasonable request.
Abbreviations
- MHC:
-
Maternal hypercholesterolemia
- NC:
-
Normocholesterolemia
- NCM:
-
Normocholesterolemic mother
- HCM:
-
Hypercholesterolemic mother
- TC:
-
Total cholesterol
- LDL:
-
Low-density lipoprotein
- HDL:
-
High-density lipoprotein
- TG:
-
Triglyceride
- VLDL:
-
Very low-density lipoprotein
- CB:
-
Cord blood
- NB:
-
Neonatal blood
- BW:
-
Birth weight
- PW:
-
Placental weight
- LUC:
-
Length of umbilical cord
- PE:
-
Placental efficiency
- LDLR:
-
Low-density lipoprotein receptor
- VLDLR:
-
Very low-density lipoprotein receptor
- CETP:
-
Cholesteryl ester transfer protein
- PPARG:
-
Peroxisome proliferator-activated receptor gamma
References
Napoli C, D’Armiento FP, Mancini FP et al (1997) Fatty streak formation occurs in human fetal aortas and is greatly enhanced by maternal hypercholesterolemia. Intimal accumulation of low density lipoprotein and its oxidation precede monocyte recruitment into early atherosclerotic lesions. J Clin Invest 100:2680–2690
Napoli C, Glass CK, Witztum JL et al (1999) Influence of maternal hypercholesterolaemia during pregnancy on progression of early atherosclerotic lesions in childhood: Fate of Early Lesions in Children (FELIC) study. The Lancet 354:1234–1241. https://doi.org/10.1016/S0140-6736(99)02131-5
Esfarjani SV, Iravani E, Azar MR (2013) Determination of the lipid profile of cord blood in neonates and its correlation with maternal age in Iran. J Compr Ped 4:72–76. https://doi.org/10.17795/compreped-6347
Aletayeb SMH, Dehdashtian M, Aminzadeh M et al (2013) Correlation between umbilical cord blood lipid profile and neonatal birth weight. Pediatr Pol 88:521–525. https://doi.org/10.1016/j.pepo.2013.08.004
Yh T, Anjum SK (2018) Cord blood lipid profile in late preterm and term neonates. Int J Contemp Pediatr 5:542–546
Pac-Kożuchowska E, Rakuś-Kwiatosz A, Krawiec P (2018) Cord blood lipid profile in healthy newborns: A prospective single-center study. Adv Clin Exp Med 27:343–349. https://doi.org/10.17219/acem/65854
Raabe M, Flynn LM, Zlot CH et al (1998) Knockout of the abetalipoproteinemia gene in mice: reduced lipoprotein secretion in heterozygotes and embryonic lethality in homozygotes. Proc Natl Acad Sci USA 95:8686–8691. https://doi.org/10.1073/pnas.95.15.8686
Ethier-Chiasson M, Duchesne A, Forest J-C et al (2007) Influence of maternal lipid profile on placental protein expression of LDLr and SR-BI. Biochem Biophys Res Commun 359:8–14. https://doi.org/10.1016/j.bbrc.2007.05.002
Marseille-Tremblay C, Ethier-Chiasson M, Forest J-C et al (2008) Impact of maternal circulating cholesterol and gestational diabetes mellitus on lipid metabolism in human term placenta. Mol Reprod Dev 75:1054–1062. https://doi.org/10.1002/mrd.20842
Zhang R, Dong S, Ma W-W et al (2017) Modulation of cholesterol transport by maternal hypercholesterolemia in human full-term placenta. PLoS ONE 12:e0171934. https://doi.org/10.1371/journal.pone.0171934
Talbert LM, Pearlman WH, Potter HD (1977) Maternal and fetal serum levels of total cortisol and cortisone, unbound cortisol, and corticosteroid-binding globulin in vaginal delivery and cesarean section. Am J Obstet Gynecol 129:781–786. https://doi.org/10.1016/0002-9378(77)90397-0
Tsang R, Glueck CJ, Evans G, Steiner PM (1974) Cord blood hypertriglyceridemia. Am J Dis Child 127:78–82. https://doi.org/10.1001/archpedi.1974.02110200080011
Hardell LI (1981) Serum lipids and lipoproteins at birth based on a study of 2815 newborn infants. Acta Paediatr 70:5–10. https://doi.org/10.1111/j.1651-2227.1981.tb15876.x
Wong W, Hachey D, Insull W et al (1993) Effect of dietary cholesterol on cholesterol synthesis in breast-fed and formula-fed infants. J Lipid Res 34:1403–1411. https://doi.org/10.1016/S0022-2275(20)36969-8
Fujita H, Okada T, Inami I et al (2008) Low-density lipoprotein profile changes during the neonatal period. J Perinatol 28:335–340. https://doi.org/10.1038/jp.2008.8
Segni M (2000) Neonatal Hyperthyroidism. In: Feingold KR, Anawalt B, Boyce A (eds) Endotext. MDText.com, Inc., South Dartmouth (MA)
Herrera E (2002) Lipid metabolism in pregnancy and its consequences in the fetus and newborn. Endocr 19:43–55. https://doi.org/10.1385/ENDO:19:1:43
Wiznitzer A, Mayer A, Novack V et al (2009) Association of lipid levels during gestation with preeclampsia and gestational diabetes mellitus: a population-based study. Am J Obstet Gynecol 201:482.e1-482.e8. https://doi.org/10.1016/j.ajog.2009.05.032
Mauricio R, Khera A (2022) Statin use in pregnancy: is it time for a paradigm shift? Circulation 145:496–498. https://doi.org/10.1161/CIRCULATIONAHA.121.058983
Research C for DE and (2021) FDA requests removal of strongest warning against using cholesterol-lowering statins during pregnancy; still advises most pregnant patients should stop taking statins. FDA. https://www.fda.gov/drugs/drug-safety-and-availability/fda-requests-removal-strongest-warning-against-usingcholesterol-lowering-tatins-during-pregnancy
Stefulj J, Panzenboeck U, Becker T et al (2009) Human endothelial cells of the placental barrier efficiently deliver cholesterol to the fetal circulation via ABCA1 and ABCG1. Circ Res 104:600–608. https://doi.org/10.1161/CIRCRESAHA.108.185066
Olaleye AA, Nwafor JI, Ebere IC et al (2019) The relationship between the weight of the placenta and birth weight of term neonate delivered in Alex Ekwueme Federal University Teaching Hospital Abakaliki, Nigeria. Adv Reprod Sci 7:82–93. https://doi.org/10.4236/arsci.2019.74010
Panti AA, Ekele BA, Nwobodo EI, Yakubu A (2012) The relationship between the weight of the placenta and birth weight of the neonate in a Nigerian Hospital. Niger Med J 53:80–84. https://doi.org/10.4103/0300-1652.103547
Janthanaphan M, Kor-Anantakul O, Geater A (2006) Placental weight and its ratio to birth weight in normal pregnancy at Songkhlanagarind Hospital. J Med Assoc Thai 89:130–137
Soysal C, Şişman Hİ, Bıyık İ et al (2021) The relationship between umbilical cord measurements and newborn outcomes. Perinatal J 29:225–230. https://doi.org/10.2399/prn.21.0293008
Balkawade NU, Shinde MA (2012) Study of length of umbilical cord and fetal outcome: a study of 1,000 deliveries. J Obstet Gynaecol India 62:520–525. https://doi.org/10.1007/s13224-012-0194-0
Krakowiak P, Smith EN, de Bruyn G, Lydon-Rochelle MT (2004) Risk factors and outcomes associated with a short umbilical cord. Obstet Gynecol 103:119–127. https://doi.org/10.1097/01.AOG.0000102706.84063.C7
Olaya-C M, Vargas W, Martinez RA et al (2020) Impact of umbilical cord length on fetal circulatory system by Doppler assessment. J Ultrasound 23:585–592. https://doi.org/10.1007/s40477-020-00495-2
Krishnan KD, Avabratha KS, D’Souza AJ (2017) Estimation of average birth weight in term newborns: a hospital-based study in coastal Karnataka. Int J Contemp Pediatr 1:156–159
Gupta R, Goyal A, Gupta M (2021) Study of cord blood lipid profile at birth and its relation to gestational maturity and birth weight. Asian J Med Sci 12:20–23. https://doi.org/10.3126/ajms.v12i1.30758
Hayward CE, Lean S, Sibley CP et al (2016) Placental adaptation: what can we learn from birthweight: placental weight ratio? Front Physiol 7:28
Fowden AL, Sferruzzi-Perri AN, Coan PM et al (2009) Placental efficiency and adaptation: endocrine regulation. J Physiol 587:3459–3472. https://doi.org/10.1113/jphysiol.2009.173013
Jellinger PS, Handelsman Y, Rosenblit PD et al (2017) American Association of Clinical Endocrinologists and American College of endocrinology guidelines for management of dyslipidemia and prevention of cardiovascular disease. Endocr Pract 23:1–87. https://doi.org/10.4158/EP171764.APPGL
Kumar A, Pandit K, Chatterjee P et al (2021) Lipid profile in infant. Indian J Endocrinol Metab 25:20–22. https://doi.org/10.4103/ijem.IJEM_396_20
Pirahanchi Y, Sinawe H, Dimri M (2022) Biochemistry, LDL Cholesterol. StatPearls. StatPearls Publishing, Treasure Island (FL)
Palinski W (2014) Effect of maternal cardiovascular conditions and risk factors on offspring cardiovascular disease. Circulation 129:2066–2077. https://doi.org/10.1161/CIRCULATIONAHA.113.001805
Acknowledgements
We acknowledge the volunteers who participated in the study. We thank the nurses and staff of the labor room and neonatal intensive care unit (NICU) of Kerala Institute of Medical Sciences.
Funding
This work was supported by the Indian Council of Medical Research (ICMR), Ministry of Health, Government of India (File No. 5/4/1-5/2019-NCD-II). Jayalekshmi VS was funded by INSPIRE Ph.D. fellowship from the Department of Science and Technology, Government of India (IF170711).
Author information
Authors and Affiliations
Contributions
JVS: performed the experiments, researched data, interpreted the data, and prepared the manuscript. JRS: collected and prepared the samples for analysis. SS: coded the recruits and curated the data. RP: recruited the subjects and provided the resources. VR: coordinated the study in KIMS hospital. SR: supervised the study, and reviewed and edited the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest. Authors also declare there are no financial interests exist.
Ethical approval
The study was approved by the Institutional Human Ethics Committee, Rajiv Gandhi Centre for Biotechnology (RGCB/IHEC/2019/10), and Institutional Human Ethics Committee, Kerala Institute of Medical Sciences (KIMS/IHEC/Hypercholesterolemia/NC/09/2019).
Consent to participate
Written informed consent was obtained from all recruited pregnant subjects for the study. Written informed consent was signed by the mothers for their neonates.
Consent for publication
Written informed consent to publish was individually obtained from all subjects. Consent to publish was obtained from the mothers of their neonates.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Jayalekshmi, V.S., Jagannath, R.S., Sreelekshmi, S. et al. Maternal hypercholesterolemia during gestation is associated with elevated lipid levels of two-day-old neonates. Mol Cell Biochem 479, 363–371 (2024). https://doi.org/10.1007/s11010-023-04739-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11010-023-04739-7