Abstract
Primary hyperparathyroidism is a common endocrine disorder. Interestingly, the majority (75%) of parathyroid tumors are localized to the inferior parathyroid glands. To date, the reason for this natural bias has not been investigated. We assessed the global gene expression profile of superior and inferior glands obtained from forensic autopsies. The genes with significant differential expression between superior and inferior parathyroids were further assessed by RT-PCR in 19 pairs. As an iterative approach, additional genes with an established role in parathyroid disorders, i.e., CASR, MAFB, PAX9, TBCE, TBX1, VDR, MEN1, CCND1, and CDC73 were also evaluated by RT-PCR in all 19 pairs of superior and inferior parathyroid glands. Seven homeobox genes, namely HOXA4, HOXA5, HOXBAS3, HOXB4, HOXB6, HOXB9, IRX1, and one encoding for ALDH1A2 showed a lower expression in the inferior parathyroid glands than in the superior. Conversely, SLC6A1 showed a higher expression in the inferior glands. Of the nine genes with significant differential mRNA expression among superior and inferior glands HOXB9, HOXB4 and IRX1 could be detected by western blotting/mass spectrometry. The study is the first to show the differential expression of nine genes HOXA4, HOXA5, HOXBAS3, HOXB4, HOXB6, HOXB9, IRX1, ALDH1A2, and SLC6A1 in inferior versus the superior parathyroid glands. This could have potential implications for the preferential localization of parathyroid tumors to the inferior parathyroid glands as observed in patients with primary hyperparathyroidism.



Similar content being viewed by others
Data availability
Some or all datasets generated during and/or analyzed during the current study are not publicly available but are available from the corresponding author upon reasonable request.
References
Bhadada SK, Arya AK, Mukhopadhyay S, Khadgawat R, Sukumar S, Lodha S, Singh DN, Sathya A, Singh P, Bhansali A (2018) Primary hyperparathyroidism: insights from the Indian PHPT registry. J Bone Miner Metab 36:238–245. https://doi.org/10.1007/s00774-017-0833-8
Brewer K, Costa-Guda J, Arnold A (2019) Molecular genetic insights into sporadic primary hyperparathyroidism. Endocr-Relat Cancer 26:R53–R72. https://doi.org/10.1530/ERC-18-0304
Marzouki HZ, Chavannes M, Tamilia M, Hier MP, Black MJ, Levental M, Payne RJ (2010) Location of parathyroid adenomas: 7-year experience. J Otolaryngol Head Neck Surg 39:551–554
Uludag M, Yazici P, Mihmanli M, Bozdag E, Aygun N (2015) Location of parathyroid adenomas in primary hyperparathyroidism: where to look? W J Endocr Surg 7:1–5. https://doi.org/10.5005/jp-journals-100021155
Jha S, Jayaraman M, Jha A, Jha R, Modi K, Kelwadee J (2016) Primary hyperparathyroidism: achanging scenario in India. Indian J Endocr Metab 20:80. https://doi.org/10.4103/2230-8210.172237
Koea JB, Shaw JHF (1999) Parathyroid cancer: biology and management. Surg Oncol 8:155–165. https://doi.org/10.1016/S0960-7404(99)00037-7
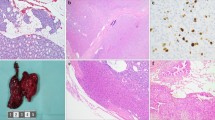
Agarwal S, Kardam S, Chatterjee P, Kumar C, Boruah M, Sharma MC, Tabin M, Ramakrishnan L (2022) CaSR expression in normal parathyroid and PHPT: new insights into pathogenesis from an autopsy-based study. J Endocrinol Invest 45:337–346. https://doi.org/10.1007/s40618-021-01646-w
Kar P, Millo T, Saha S, Mahtab S, Agarwal S, Goswami R (2021) Osteogenic mechanisms of basal ganglia calcification and its ex vivo model in the hypoparathyroid milieu. Endocrinology 162:bqab024. https://doi.org/10.1210/endocr/bqab024
Singh P, Chakraborty R, Marwal R, Radhakrishan VS, Bhaskar AK, Vashisht H, Dhar MS, Pradhan S, Ranjan G, Imran M, Raj A, Sharma U, Singh P, Lall H, Dutta M, Garg P, Ray A, Dash D, Sivasubbu S, Gogia H, Madan P, Kabra S, Singh SK, Agrawal A, Rakshit P, Kumar P, Sengupta S (2020) A rapid and sensitive method to detect SARS-CoV-2 virus using targeted-mass spectrometry. J Proteins Proteom 11:159–165. https://doi.org/10.1007/s42485-020-00044-9
Feng Y, Zhang T, Wang Y, Xie M, Ji X, Luo X, Huang W, Xia L (2021) Homeobox genes in cancers: from carcinogenesis to recent therapeutic intervention. Front Oncol 11:770428. https://doi.org/10.3389/fonc.2021.770428
Huang J-Z, Chen M, Chen D, Gao X-C, Zhu S, Huang H, Hu M, Zhu H, Yan G-R (2017) A Peptide encoded by a putative lncRNA HOXB-AS3 suppresses colon cancer growth. Mol Cell 68:171-184.e6. https://doi.org/10.1016/j.molcel.2017.09.015
Jung IH, Jung DE, Chung Y-Y, Kim K-S, Park SW (2019) Iroquois homeobox 1 acts as a true tumor suppressor in multiple organs by regulating cell cycle progression. Neoplasia 21:1003–1014. https://doi.org/10.1016/j.neo.2019.08.001
Brotto DB, Siena ÁD, de Barros II, Carvalho SD, Muys BR, Goedert L, Cardoso C, Plaça JR, Ramão A, Squire JA, Araujo LF (2020) Contributions of HOX genes to cancer hallmarks: enrichment pathway analysis and review. Tumour Biol 42:101042832091805. https://doi.org/10.1177/1010428320918050
Küster MM, Schneider MA, Richter AM, Richtmann S, Winter H, Kriegsmann M, Pullamsetti SS, Stiewe T, Savai R, Muley T, Dammann RH (2020) Epigenetic inactivation of the tumor suppressor IRX1 occurs frequently in lung adenocarcinoma and its silencing is associated with impaired prognosis. Cancers 12:3528. https://doi.org/10.3390/cancers12123528
Shen H-CJ, Rosen JE, Yang LM, Savage SA, Burns AL, Mateo CM, Agarwal SK, Chandrasekharappa SC, Spiegel AM, Collins FS, Marx SJ, Libutti SK (2008) Parathyroid tumor development involves deregulation of homeobox genes. Endocr Relat Cancer 15:267–275. https://doi.org/10.1677/ERC-07-0191
Wu S, Xue W, Huang X, Yu X, Luo M, Huang Y, Liu Y, Bi Z, Qiu X, Bai S (2015) Distinct prognostic values of ALDH1 isoenzymes in breast cancer. TumorBiol 36:2421–2426. https://doi.org/10.1007/s13277-014-2852-6
Choi J-A, Kwon H, Cho H, Chung J-Y, Hewitt SM, Kim J-H (2019) ALDH1A2 is a candidate tumor suppressor gene in ovarian cancer. Cancers 11:1553. https://doi.org/10.3390/cancers11101553
Maolakuerban N, Azhati B, Tusong H, Abula A, Yasheng A, Xireyazidan A (2018) MiR-200c-3p inhibits cell migration and invasion of clear cell renal cell carcinoma via regulating SLC6A1. Cancer Biol Ther 19:282–291. https://doi.org/10.1080/15384047.2017.1394551
Chen C, Cai Z, Zhuo Y, Xi M, Lin Z, Jiang F, Liu Z, Wan Y, Zheng Y, Li J, Zhou X, Zhu J, Zhong W (2020) Overexpression of SLC6A1 associates with drug resistance and poor prognosis in prostate cancer. BMC Cancer 20:289. https://doi.org/10.1186/s12885-020-06776-7
Wang Q, Wei Y, Luo L, Li X, Jiang W (2022) Integrated analysis of DNA repair genes identifies SLC6A1 as a new marker for the clinical outcome of patients with colorectal cancer. Dis Markers 2022:1–11. https://doi.org/10.1155/2022/4952812
Funding
This work was supported by the All India Institute of Medical Sciences, New Delhi (intramural Grant Number A-694).
Author information
Authors and Affiliations
Contributions
The study was designed by RG, SA; TM, CK, VS, MB, and SA, who were involved in procuring the autopsy tissues. SA, PK, MB, and SS carried out the experiments; SA helped with histopathological evaluation of the collected autopsy tissues; RG, SA, PK, and SS contributed to data analysis. All the authors contributed to the writing of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Conflict of interest
No conflicts were declared.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Agarwal, S., Kar, P., Boruah, M. et al. Innate differences in the molecular signature of normal inferior & superior human parathyroid glands: potential implications for parathyroid adenoma. Mol Cell Biochem 478, 2351–2359 (2023). https://doi.org/10.1007/s11010-023-04664-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11010-023-04664-9