Abstract
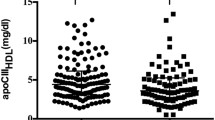
Impaired high-density lipoprotein (HDL) functions are associated with development of coronary artery disease. In this study, we explored the quantitative differences in HDL (i.e. HDL proteome and fatty acid profile of HDL phospholipids) underlying the functional deficits associated with acute coronary syndrome (ACS). The relationship between HDL function and composition was assessed in 65 consecutive ACS patients and 40 healthy controls. Cholesterol efflux capacity (CEC) of HDL and lecithin cholesterol acyl transferase (LCAT) activity were significantly lower in patients with ACS compared to controls. In HDL proteome analysis, HDL isolated from ACS individuals was enriched in apolipoprotein C2 (inhibitor of LCAT), apolipoprotein C4 and serum amyloid A proteins and was deficient in apolipoprotein A-I and A-II. The fatty acid profile of HDL phospholipids analyzed using gas chromatography showed significantly lower percentages of stearic acid (17.4 ± 2.4 vs 15.8 ± 2.8, p = 0.004) and omega-3 fatty acids [eicosapentaenoic acid (1.0 (0.6–1.4) vs 0.7 (0.4–1.0), p = 0.009) and docosahexaenoic acid (1.5 ± 0.7 vs 1.3 ± 0.5, p = 0.03)] in ACS patients compared to controls. Lower percentages of these fatty acids in HDL were associated with higher odds of developing ACS. Our results suggest that distinct phospholipid fatty acid profiles found in HDL from ACS patients could be one of the contributing factors to the deranged HDL functions in these patients apart from the protein content and the inflammatory conditions.


Similar content being viewed by others
Data availability
The list of HDL associated proteins identified using mass spectrometry (ESM_1) and the normalised abundance values of the curated HDL associated proteins (ESM_2) used for analysis is included in the article as supplementary information. The raw mass spectrometry proteomics data have been deposited to the Proteome Xchange Consortium via the PRIDE partner repository with the data set identifier PXD014411.
References
Wilson PW, Abbott RD, Castelli WP (1988) High density lipoprotein cholesterol and mortality. Framingham Heart Study Arterioscler 8:737–741
Dodani S, Grice DG, Joshi S (2009) Is HDL function as important as HDL quantity in the coronary artery disease risk assessment? J Clin Lipidol 3:70–77. https://doi.org/10.1016/j.jacl.2009.02.001
Barter PJ, Nicholls S, Rye K-A, Anantharamaiah GM, Navab M, Fogelman AM (2004) Antiinflammatory properties of HDL. Circ Res 95:764–772. https://doi.org/10.1161/01.RES.0000146094.59640.13
Negre-Salvayre A, Dousset N, Ferretti G, Bacchetti T, Curatola G, Salvayre R (2006) Antioxidant and cytoprotective properties of high-density lipoproteins in vascular cells. Free Radic Biol Med 41:1031–1040. https://doi.org/10.1016/j.freeradbiomed.2006.07.006
Annema W, von Eckardstein A (2013) High-density lipoproteins. Multifunctional but vulnerable protections from atherosclerosis. Circ J 77:2432–2448
Vickers KC, Remaley AT (2014) HDL and cholesterol: life after the divorce? J Lipid Res 55:4–12. https://doi.org/10.1194/jlr.R035964
Navab M, Reddy ST, Van Lenten BJ, Fogelman AM (2011) HDL and cardiovascular disease: atherogenic and atheroprotective mechanisms. Nat Rev Cardiol 8:222–232. https://doi.org/10.1038/nrcardio.2010.222
Shah AS, Tan L, Long JL, Davidson WS (2013) Proteomic diversity of high density lipoproteins: our emerging understanding of its importance in lipid transport and beyond1. J Lipid Res 54:2575–2585. https://doi.org/10.1194/jlr.R035725
Haapasalo K, van Kessel K, Nissilä E, Metso J, Johansson T, Miettinen S et al (2015) Complement factor H binds to human serum apolipoprotein e and mediates complement regulation on high density lipoprotein particles. J Biol Chem 290:28977–28987. https://doi.org/10.1074/jbc.M115.669226
de la Llera-Moya M, Drazul-Schrader D, Asztalos BF, Cuchel M, Rader DJ, Rothblat GH (2010) The ability to promote efflux via ABCA1 determines the capacity of serum specimens with similar high-density lipoprotein cholesterol to remove cholesterol from macrophages. Arterioscler Thromb Vasc Biol 30:796–801. https://doi.org/10.1161/ATVBAHA.109.199158
Kajani S, Curley S, McGillicuddy FC (2018) Unravelling HDL-looking beyond the cholesterol surface to the quality within. Int J Mol Sci. https://doi.org/10.3390/ijms19071971
Meikle PJ, Formosa MF, Mellett NA, Jayawardana KS, Giles C, Bertovic DA et al (2019) HDL phospholipids, but not cholesterol distinguish acute coronary syndrome from stable coronary artery disease. J Am Heart Assoc. https://doi.org/10.1161/JAHA.118.011792
Guha M, Gantz DL, Gursky O (2008) Effects of acyl chain length, unsaturation, and pH on thermal stability of model discoidal HDLs. J Lipid Res 49:1752–1761. https://doi.org/10.1194/jlr.M800106-JLR200
Parks JS, Huggins KW, Gebre AK, Burleson ER (2000) Phosphatidylcholine fluidity and structure affect lecithin:cholesterol acyltransferase activity. J Lipid Res 41:546–553
Fernández-Castillejo S, Rubió L, Hernáez Á, Catalán Ú, Pedret A, Valls R-M et al (2017) Determinants of HDL cholesterol efflux capacity after virgin olive oil ingestion: interrelationships with fluidity of HDL monolayer. Mol Nutr Food Res. https://doi.org/10.1002/mnfr.201700445
Thakkar H, Vincent V, Roy A, Singh S, Ramakrishnan L, Kalaivani M et al (2020) HDL functions and their interaction in patients with ST elevation myocardial infarction: a case control study. Lipids Health Dis 19:75. https://doi.org/10.1186/s12944-020-01260-4
Patel AP, Wang M, Kartoun U, Ng K, Khera AV (2021) Quantifying and understanding the higher risk of atherosclerotic cardiovascular disease among south Asian individuals: results from the UK biobank prospective cohort study. Circulation. https://doi.org/10.1161/CIRCULATIONAHA.120.052430
Hirano T, Nohtomi K, Koba S, Muroi A, Ito Y (2008) A simple and precise method for measuring HDL-cholesterol subfractions by a single precipitation followed by homogenous HDL-cholesterol assay. J Lipid Res 49:1130–1136. https://doi.org/10.1194/jlr.D700027-JLR200
Sankaranarayanan S, Kellner-Weibel G, de la Llera-Moya M, Phillips MC, Asztalos BF, Bittman R et al (2011) A sensitive assay for ABCA1-mediated cholesterol efflux using BODIPY-cholesterol. J Lipid Res 52:2332–2340. https://doi.org/10.1194/jlr.D018051
Perez-Riverol Y, Csordas A, Bai J, Bernal-Llinares M, Hewapathirana S, Kundu DJ et al (2019) The PRIDE database and related tools and resources in 2019: improving support for quantification data. Nucleic Acids Res 47:D442–D450. https://doi.org/10.1093/nar/gky1106
Folch J, Lees M, Sloane Stanley GH (1957) A simple method for the isolation and purification of total lipides from animal tissues. J Biol Chem 226:497–509
Lepage G, Roy CC (1986) Direct transesterification of all classes of lipids in a one-step reaction. J Lipid Res 27:114–120
Tram L, Krogh Venø S, Dahm C, Thomsen BH, Berg Johansen M, Overvad K et al (2018) Adipose tissue lipophilic index and risk of ischemic stroke-a Danish case-cohort study. Nutrients. https://doi.org/10.3390/nu10111570
Toledo E, Campos H, Ding EL, Wu H, Hu FB, Sun Q et al (2013) A novel fatty acid profile index–the lipophilic index–and risk of myocardial infarction. Am J Epidemiol 178:392–400. https://doi.org/10.1093/aje/kws476
LipidBank (2020) http://www.lipidbank.jp/. Accessed 29 Jun 2020
Mecham BH, Nelson PS, Storey JD (2010) Supervised normalization of microarrays. Bioinformatics 26:1308–1315. https://doi.org/10.1093/bioinformatics/btq118
Leek JT, Storey JD (2007) Capturing heterogeneity in gene expression studies by surrogate variable analysis. PLoS Genet 3:1724–1735. https://doi.org/10.1371/journal.pgen.0030161
Jonas A (2000) Lecithin cholesterol acyltransferase. Biochim Biophys Acta 1529:245–256
Prabhakaran D, Jeemon P, Roy A (2016) Cardiovascular diseases in India: current epidemiology and future directions. Circulation 133:1605–1620. https://doi.org/10.1161/CIRCULATIONAHA.114.008729
Alwaili K, Bailey D, Awan Z, Bailey SD, Ruel I, Hafiane A et al (2012) The HDL proteome in acute coronary syndromes shifts to an inflammatory profile. Biochem Biophys Acta 1821:405–415. https://doi.org/10.1016/j.bbalip.2011.07.013
Gordon SM, Chung JH, Playford MP, Dey AK, Sviridov D, Seifuddin F et al (2018) High density lipoprotein proteome is associated with cardiovascular risk factors and atherosclerosis burden as evaluated by coronary CT angiography. Atherosclerosis 278:278–285. https://doi.org/10.1016/j.atherosclerosis.2018.09.032
Birjmohun RS, Dallinga-Thie GM, Kuivenhoven JA, Stroes ESG, Otvos JD, Wareham NJ et al (2007) Apolipoprotein A-II is inversely associated with risk of future coronary artery disease. Circulation 116:2029–2035. https://doi.org/10.1161/CIRCULATIONAHA.107.704031
Melchior JT, Street SE, Andraski AB, Furtado JD, Sacks FM, Shute RL et al (2017) Apolipoprotein A-II alters the proteome of human lipoproteins and enhances cholesterol efflux from ABCA1. J Lipid Res 58:1374–1385. https://doi.org/10.1194/jlr.M075382
Wang Y, Niimi M, Nishijima K, Waqar AB, Yu Y, Koike T et al (2013) Human apolipoprotein A-II protects against diet-induced atherosclerosis in transgenic rabbits. Arterioscler Thromb Vasc Biol 33:224–231. https://doi.org/10.1161/ATVBAHA.112.300445
Anantharamaiah GM, Hughes TA, Iqbal M, Gawish A, Neame PJ, Medley MF et al (1988) Effect of oxidation on the properties of apolipoproteins A-I and A-II. J Lipid Res 29:309–318
Zvintzou E, Xepapadaki E, Kalogeropoulou C, Filou S, Kypreos KE (2019) Pleiotropic effects of apolipoprotein A-II on high-density lipoprotein functionality, adipose tissue metabolic activity and plasma glucose homeostasis. J Biomed Res. https://doi.org/10.7555/JBR.33.20190048
Nishida HI, Nakanishi T, Yen EA, Arai H, Yen FT, Nishida T (1986) Nature of the enhancement of lecithin-cholesterol acyltransferase reaction by various apolipoproteins. J Biol Chem 261:12028–12035
Voudris KV, Chanin J, Feldman DN, Charitakis K (2015) Novel inflammatory biomarkers in coronary artery disease: potential therapeutic approaches. Curr Med Chem 22:2680–2689. https://doi.org/10.2174/0929867322666150420124427
Witkowski A, Chan GKL, Boatz JC, Li NJ, Inoue AP, Wong JC et al (2018) Methionine oxidized apolipoprotein A-I at the crossroads of HDL biogenesis and amyloid formation. FASEB J 32:3149–3165. https://doi.org/10.1096/fj.201701127R
DiDonato JA, Aulak K, Huang Y, Wagner M, Gerstenecker G, Topbas C et al (2014) Site-specific nitration of apolipoprotein A-I at tyrosine 166 is both abundant within human atherosclerotic plaque and dysfunctional. J Biol Chem 289:10276–10292. https://doi.org/10.1074/jbc.M114.556506
Han CY, Tang C, Guevara ME, Wei H, Wietecha T, Shao B et al (2016) Serum amyloid A impairs the antiinflammatory properties of HDL. J Clin Invest 126:266–281. https://doi.org/10.1172/JCI83475
DiNicolantonio JJ, O’Keefe JH (2018) Effects of dietary fats on blood lipids: a review of direct comparison trials. Open Heart 5:e000871. https://doi.org/10.1136/openhrt-2018-000871
Yanai H, Katsuyama H, Hamasaki H, Abe S, Tada N, Sako A (2015) Effects of dietary fat intake on HDL metabolism. J Clin Med Res 7:145–149. https://doi.org/10.14740/jocmr2030w
Averill M, Rubinow KB, Cain K, Wimberger J, Babenko I, Becker JO et al (2020) Postprandial remodeling of high-density lipoprotein following high saturated fat and high carbohydrate meals. J Clin Lipidol 14:66-76.e11. https://doi.org/10.1016/j.jacl.2019.11.002
Sola R, Baudet MF, Motta C, Maillé M, Boisnier C, Jacotot B (1990) Effects of dietary fats on the fluidity of human high-density lipoprotein: influence of the overall composition and phospholipid fatty acids. Biochim Biophys Acta 1043:43–51. https://doi.org/10.1016/0005-2760(90)90108-a
Liu Q, Matthan NR, Manson JE, Howard BV, Tinker LF, Neuhouser ML et al (2019) Plasma phospholipid fatty acids and coronary heart disease risk: a matched case-control study within the women’s health initiative observational study. Nutrients. https://doi.org/10.3390/nu11071672
Paavola T, Bergmann U, Kuusisto S, Kakko S, Savolainen MJ, Salonurmi T (2021) Distinct fatty acid compositions of HDL phospholipids are characteristic of metabolic syndrome and premature coronary heart disease-family study. Int J Mol Sci 22:4908. https://doi.org/10.3390/ijms22094908
Chen M, Li Y, Sun Q, Pan A, Manson JE, Rexrode KM et al (2016) Dairy fat and risk of cardiovascular disease in 3 cohorts of US adults. Am J Clin Nutr 104:1209–1217. https://doi.org/10.3945/ajcn.116.134460
Wu JHY, Lemaitre RN, King IB, Song X, Psaty BM, Siscovick DS et al (2014) Circulating omega-6 polyunsaturated fatty acids and total and cause-specific mortality: the cardiovascular health study. Circulation 130:1245–1253. https://doi.org/10.1161/CIRCULATIONAHA.114.011590
Harris WS, Poston WC, Haddock CK (2007) Tissue n-3 and n-6 fatty acids and risk for coronary heart disease events. Atherosclerosis 193:1–10. https://doi.org/10.1016/j.atherosclerosis.2007.03.018
Shearer GC, Walker RE (2018) An overview of the biologic effects of omega-6 oxylipins in humans. Prostaglandins Leukot Essent Fatty Acids 137:26–38. https://doi.org/10.1016/j.plefa.2018.06.005
Baker PW, Rye KA, Gamble JR, Vadas MA, Barter PJ (2000) Phospholipid composition of reconstituted high density lipoproteins influences their ability to inhibit endothelial cell adhesion molecule expression. J Lipid Res 41:1261–1267
Chang HY, Lee H-N, Kim W, Surh Y-J (2015) Docosahexaenoic acid induces M2 macrophage polarization through peroxisome proliferator-activated receptor γ activation. Life Sci 120:39–47. https://doi.org/10.1016/j.lfs.2014.10.014
Gallagher H, Williams JO, Ferekidis N, Ismail A, Chan Y-H, Michael DR et al (2019) Dihomo-γ-linolenic acid inhibits several key cellular processes associated with atherosclerosis. Biochim Biophys Acta Mol Basis Dis 1865:2538–2550. https://doi.org/10.1016/j.bbadis.2019.06.011
Tanaka N, Irino Y, Shinohara M, Tsuda S, Mori T, Nagao M et al (2018) Eicosapentaenoic acid-enriched high-density lipoproteins exhibit anti-atherogenic properties. Circ J 82:596–601. https://doi.org/10.1253/circj.CJ-17-0294
Zhang L-Y, Ding L, Shi H-H, Xu J, Xue C-H, Zhang T-T et al (2019) Eicosapentaenoic acid in the form of phospholipids exerts superior anti-atherosclerosis effects to its triglyceride form in ApoE-/-mice. Food Funct 10:4177–4188. https://doi.org/10.1039/c9fo00868c
Bhatt DL, Steg PG, Miller M, Brinton EA, Jacobson TA, Ketchum SB et al (2019) Effects of Icosapent ethyl on total ischemic events: from REDUCE-IT. J Am Coll Cardiol 73:2791–2802. https://doi.org/10.1016/j.jacc.2019.02.032
Pizzini A, Lunger L, Demetz E, Hilbe R, Weiss G, Ebenbichler C et al (2017) The role of omega-3 fatty acids in reverse cholesterol transport: a review. Nutrients 9:1099. https://doi.org/10.3390/nu9101099
Cedó L, Metso J, Santos D, Sánchez-Quesada JL, Julve J, García-León A et al (2015) Consumption of polyunsaturated fat improves the saturated fatty acid-mediated impairment of HDL antioxidant potential. Mol Nutr Food Res 59:1987–1996. https://doi.org/10.1002/mnfr.201500336
Kostara CE, Ferrannini E, Bairaktari ET, Papathanasiou A, Elisaf M, Tsimihodimos V (2020) Early signs of atherogenic features in the HDL lipidomes of normolipidemic patients newly diagnosed with type 2 diabetes. Int J Mol Sci 21:8835. https://doi.org/10.3390/ijms21228835
Ronsein GE, Vaisar T (2017) Inflammation, remodeling and other factors affecting HDL cholesterol efflux. Curr Opin Lipidol 28:52–59. https://doi.org/10.1097/MOL.0000000000000382
Degoricija V, Potočnjak I, Gastrager M, Pregartner G, Berghold A, Scharnagl H et al (2019) HDL subclasses and mortality in acute heart failure patients. Clin Chim Acta 490:81–87. https://doi.org/10.1016/j.cca.2018.12.020
Kim DS, Burt AA, Rosenthal EA, Ranchalis JE, Eintracht JF, Hatsukami TS et al (2014) HDL-3 is a superior predictor of carotid artery disease in a case-control cohort of 1725 participants. J Am Heart Assoc 3:e000902. https://doi.org/10.1161/JAHA.114.000902
Zerrad-Saadi A, Therond P, Chantepie S, Couturier M, Rye K-A, Chapman MJ et al (2009) HDL3-mediated inactivation of LDL-associated phospholipid hydroperoxides is determined by the redox status of apolipoprotein A-I and HDL particle surface lipid rigidity: relevance to inflammation and atherogenesis. Arterioscler Thromb Vasc Biol 29:2169–2175. https://doi.org/10.1161/ATVBAHA.109.194555
Kröger J, Jacobs S, Jansen EHJM, Fritsche A, Boeing H, Schulze MB (2015) Erythrocyte membrane fatty acid fluidity and risk of type 2 diabetes in the EPIC-potsdam study. Diabetologia 58:282–289. https://doi.org/10.1007/s00125-014-3421-7
Liu Q, Lichtenstein AH, Matthan NR, Howe CJ, Allison MA, Howard BV et al (2017) Higher lipophilic index indicates higher risk of coronary heart disease in postmenopausal women. Lipids 52:687–702. https://doi.org/10.1007/s11745-017-4276-8
Xu H, Ärnlöv J, Sandhagen B, Risérus U, Lindholm B, Lind L et al (2016) Lipophilic index, kidney function, and kidney function decline. Nutr Metab Cardiovasc Dis 26:1096–1103. https://doi.org/10.1016/j.numecd.2016.09.006
Sharma M, Kishore A, Roy D, Joshi K (2020) A comparison of the Indian diet with the EAT-lancet reference diet. BMC Public Health 20:812. https://doi.org/10.1186/s12889-020-08951-8
Acknowledgements
Young Scientist fellowship from Department of Health and Research, Ministry of Health and Family Welfare, Government of India, awarded to Himani Thakkar is gratefully acknowledged.
Funding
No funding was received for conducting this study.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by HT, VV, AKG and RK. The first draft of the manuscript was written by HT, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare that are relevant to the content of this article.
Ethical approval
The study was approved by the Institute Ethics Committee of All India Institute of Medical Sciences, New Delhi (Ethics committee reference number: IESC/T-380/17.10.2014) and certify that the study was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Thakkar, H., Vincent, V., Roy, A. et al. Determinants of high-density lipoprotein (HDL) functions beyond proteome in Asian Indians: exploring the fatty acid profile of HDL phospholipids. Mol Cell Biochem 477, 559–570 (2022). https://doi.org/10.1007/s11010-021-04304-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11010-021-04304-0