Abstract
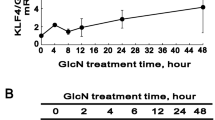
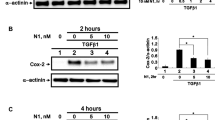
Conjunctival fibrosis is a process of extracellular matrix accumulation and the appearance of myofibroblasts in subconjunctival fibroblasts induced by injury or inflammation, which can significantly reduce the filtration efficiency of glaucoma filtration surgery. In this study, autophagy was confirmed to be involved in regulating the fibrosis of human subconjunctival fibroblasts (hSCFs) induced by TGF-β1. Following the addition of rapamycin, we detected that autophagy activation could reduce the increased expression level of αSMA and the accumulation of extracellular matrix component proteins namely fibronectin and type I collagen induced by TGF-β1 via the inhibition of SMAD2 phosphorylation. Following the addition of HCQ, the inhibition of autophagy aggravated TGF-β1-induced fibrosis of hSCFs. We further verified that trehalose, a safe clinical drug, could alleviate TGF-β1-induced fibrosis of hSCFs by activating autophagy and that these effects could be blocked by autophagy inhibition. In summary, autophagy was shown to be involved in the regulation of TGF-β1-induced fibrosis of hSCFs, which provided a novel perspective for exploring the progression of this lesion. More importantly, the protective effects of trehalose on TGF-β1-induced fibrosis of hSCFs were mediated by the activation of autophagy and could provide possible new approaches for the clinical treatment of conjunctival fibrosis.






Similar content being viewed by others
Abbreviations
- hSCFs:
-
Human subconjunctival fibroblasts
- GFS:
-
Glaucoma filtration surgery
- OCP:
-
Ocular cicatrial pemphigoid
- VKC:
-
Vernal keratoconjunctivitis
- ECM:
-
Extracellular matrix
- αSMA:
-
α-Smooth muscle actin
- CTGF:
-
Connective tissue growth factor
- FN:
-
Fibronectin
- COLA1:
-
Type I collagen
- HCQ:
-
Hydroxychloroquine
- ROS:
-
Reactive oxygen species
References
Saika S, Yamanaka O, Sumioka T, Miyamoto T, Miyazaki K, Okada Y, Kitano A, Shirai K, Tanaka S, Ikeda K (2008) Fibrotic disorders in the eye: targets of gene therapy. Prog Retin Eye Res 27:177–196. https://doi.org/10.1016/j.preteyeres.2007.12.002
Jinza K, Saika S, Kin K, Ohnishi Y (2000) Relationship between formation of a filtering bleb and an intrascleral aqueous drainage route after trabeculectomy: evaluation using ultrasound biomicroscopy. Ophthal Res 32:240–243. https://doi.org/10.1159/000055620
Daniels JT, Schultz GS, Blalock TD, Garrett Q, Grotendorst GR, Dean NM, Khaw PT (2003) Mediation of transforming growth factor-beta(1)-stimulated matrix contraction by fibroblasts: a role for connective tissue growth factor in contractile scarring. Am J Pathol 163:2043–2052. https://doi.org/10.1016/s0002-9440(10)63562-6
Zada M, Pattamatta U, White A (2018) Modulation of fibroblasts in conjunctival wound healing. Ophthalmology 125:179–192. https://doi.org/10.1016/j.ophtha.2017.08.028
Roberts AB, Russo A, Felici A, Flanders KC (2003) Smad3: a key player in pathogenetic mechanisms dependent on TGF-beta. Ann N Y Acad Sci 995:1–10. https://doi.org/10.1111/j.1749-6632.2003.tb03205.x
Yamanaka O, Miyazaki K, Kitano A, Saika S, Nakajima Y, Ikeda K (2009) Suppression of injury-induced conjunctiva scarring by peroxisome proliferator-activated receptor γ gene transfer in mice. Invest Ophthalmol Vis Sci 50:187–193. https://doi.org/10.1167/iovs.08-2282
Yamanaka O, Ikeda K, Saika S, Miyazaki K, Ooshima A, Ohnishi Y (2006) Gene transfer of Smad7 modulates injury-induced conjunctival wound healing in mice. Mol Vis 12:841–851
Futakuchi A, Inoue T, Wei FY, Inoue-Mochita M, Fujimoto T, Tomizawa K, Tanihara H (2018) YAP/TAZ are essential for TGF-b2–mediated conjunctival fibrosis. Invest Ophthalmol Vis Sci 59:3069–3078. https://doi.org/10.1167/iovs.18-24258
Martin LM, Jeyabalan N, Tripathi R, Panigrahi T, Johnson PJ, Ghosh A, Mohan RR (2019) Autophagy in corneal health and disease: a concise review. Ocul Surf 17:186–197. https://doi.org/10.1016/j.jtos.2019.01.008
Chai P, Ni H, Zhang H, Fan X (2016) The evolving functions of autophagy in ocular health: a double-edged sword. Int J Biol Sci 12:1332–1340. https://doi.org/10.7150/ijbs.16245
Lum JJ, Bauer DE, Kong M, Harris MH, Li C, Lindsten T, Thompson CB (2005) Growth factor regulation of autophagy and cell survival in the absence of apoptosis. Cell 120:237–248. https://doi.org/10.1016/j.cell.2004.11.046
Ye HL, Zhang JW, Chen XZ, Wu PB, Chen L, Zhang G (2020) Ursodeoxycholic acid alleviates experimental liver fibrosis involving inhibition of autophagy. Life Sci 242:117175. https://doi.org/10.1016/j.lfs.2019.117175
Cosin-Roger J, Canet F, Macias-Ceja DC, Gisbert-Ferrándiz L, Ortiz-Masiá D, Esplugues JV, Alós R, Navarro F, Barrachina MD, Calatayud S (2019) Autophagy stimulation as a potential strategy against intestinal fibrosis. Cells 8:E1078. https://doi.org/10.3390/cells8091078
Mathur R, Alam MM, Zhao XF, Liao Y, Shen J, Morgan S, Huang T, Lee H, Lee E, Huang Y, Zhu X (2019) Induction of autophagy in Cx3cr1+ mononuclear cells limits IL-23/IL-22 axis-mediated intestinal fibrosis. Mucosal Immunol 12:612–623. https://doi.org/10.1038/s41385-019-0146-4
Wang L, Yuan D, Zheng J, Wu X, Wang J, Liu X, He Y, Zhang C, Liu C, Wang T, Zhou Z (2019) Chikusetsu saponin IVa attenuates isoprenaline-induced myocardial fibrosis in mice through activation autophagy mediated by AMPK/mTOR/ULK1 signaling. Phytomedicine 58:152764. https://doi.org/10.1016/j.phymed.2018.11.024
Li S, Peng F, Gong W, Wu J, Wang Y, Xu Z, Liu W, Li H, Yin B, Zhang Y, Chen S, Luo C, Li P, Chen Y, Huang Q, Zhou W, Long H (2019) Dimethylaminomicheliolide ameliorates peritoneal fibrosis through the activation of autophagy. J Mol Med (Berl) 97:659–674. https://doi.org/10.1007/s00109-019-01757-1
Hill C, Li J, Liu D, Conforti F, Brereton CJ, Yao L, Zhou Y, Alzetani A, Chee SJ, Marshall BG, Fletcher SV, Hancock D, Ottensmeier CH, Steele AJ, Downward J, Richeldi L, Lu X, Davies DE, Jones MG, Wang Y (2019) Autophagy inhibition-mediated epithelial–mesenchymal transition augments local myofibroblast differentiation in pulmonary fibrosis. Cell Death Dis 10:591. https://doi.org/10.1038/s41419-019-1820-x
Du S, Li C, Lu Y, Lei X, Zhang Y, Li S, Liu F, Chen Y, Weng D, Chen J (2019) Dioscin alleviates crystalline silica-induced pulmonary inflammation and fibrosis through promoting alveolar macrophage autophagy. Theranostics 9:1878–1892. https://doi.org/10.7150/thno.29682
Zhang F, Liu K, Cao M, Qu J, Zhou D, Pan Z, Duan X, Zhou Y (2019) Rosiglitazone treatment prevents postoperative fibrosis in a rabbit model of glaucoma filtration surgery. Invest Ophthalmol Vis Sci 60:2743–2752. https://doi.org/10.1167/iovs.18-26526
Collins J, Robinson C, Danhof H, Knetsch CW, van Leeuwen HC, Lawley TD, Auchtung JM, Britton RA (2018) Dietary trehalose enhances virulence of epidemic Clostridium difficile. Nature 553:291–294. https://doi.org/10.1038/nature25178
Chou LF, Cheng YL, Hsieh CY, Lin CY, Yang HY, Chen YC, Hung CC, Tian YC, Yang CW, Chang MY (2019) Effect of trehalose supplementation on autophagy and cystogenesis in a mouse model of polycystic kidney disease. Nutrients 11:E42. https://doi.org/10.3390/nu11010042
Emanuele E (2014) Can trehalose prevent neurodegeneration? Insights from experimental studies. Curr Drug Targets 15:551–557. https://doi.org/10.2174/1389450115666140225104705
Lee HJ, Yoon YS, Lee SJ (2018) Mechanism of neuroprotection by trehalose: controversy surrounding autophagy induction. Cell Death Dis 9:712. https://doi.org/10.1038/s41419-018-0749-9
Kaplon RE, Hill SD, Bispham NZ, Santos-Parker JR, Nowlan MJ, Snyder LL, Chonchol M, LaRocca TJ, McQueen MB, Seals DR (2016) Oral trehalose supplementation improves resistance artery endothelial function in healthy middle-aged and older adults. Aging 8:1167–1183. https://doi.org/10.18632/aging.100962
Evans TD, Jeong SJ, Zhang X, Sergin I, Razani B (2018) TFEB and trehalose drive the macrophage autophagy-lysosome system to protect against atherosclerosis. Autophagy 14:724–726. https://doi.org/10.1080/15548627.2018.1434373
Fondi K, Wozniak PA, Schmidl D, Bata AM, Witkowska KJ, Popa-Cherecheanu A, Schmetterer L, Garhöfer G (2018) Effect of hyaluronic acid/trehalose in two different formulations on signs and symptoms in patients with moderate to severe dry eye disease. J Ophthalmol 2018:4691417. https://doi.org/10.1155/2018/4691417
Pinto-Bonilla JC, Del Olmo-Jimeno A, Llovet-Osuna F, Hernández-Galilea E (2015) A randomized crossover study comparing trehalose/hyaluronate eyedrops and standard treatment: patient satisfaction in the treatment of dry eye syndrome. Ther Clin Risk Manag 11:595–603. https://doi.org/10.2147/TCRM.S77091
Hosseinpour-Moghaddam K, Caraglia M, Sahebkar A (2018) Autophagy induction by trehalose: molecular mechanisms and therapeutic impacts. J Cell Physiol 233:6524–6543. https://doi.org/10.1002/jcp.26583
Sciarretta S, Yee D, Nagarajan N, Bianchi F, Saito T, Valenti V, Tong M, Del Re DP, Vecchione C, Schirone L, Forte M, Rubattu S, Shirakabe A, Boppana VS, Volpe M, Frati G, Zhai P, Sadoshima J (2018) Trehalose-induced activation of autophagy improves cardiac remodeling after myocardial infarction. J Am Coll Cardiol 71:1999–2010. https://doi.org/10.1016/j.jacc.2018.02.066
Ruan S, Xie R, Qin L, Yu M, Xiao W, Hu C, Yu W, Qian Z, Ouyang L, He Q, Gao H (2019) Aggregable nanoparticles-enabled chemotherapy and autophagy inhibition combined with anti-PD-L1 antibody for improved glioma treatment. Nano Lett 19:8318–8332. https://doi.org/10.1021/acs.nanolett.9b03968
Liu LQ, Wang SB, Shao YF, Shi JN, Wang W, Chen WY, Ye ZQ, Jiang JY, Fang QX, Zhang GB, Xuan ZX (2019) Hydroxychloroquine potentiates the anti-cancer effect of bevacizumab on glioblastoma via the inhibition of autophagy. Biomed Pharmacother 118:109339. https://doi.org/10.1016/j.biopha.2019.109339
Ulla A, Mohamed MK, Sikder B, Rahman AT, Sumi FA, Hossain M, Reza HM, Rahman GMS, Alam MA (2017) Coenzyme Q10 prevents oxidative stress and fibrosis in isoprenaline induced cardiac remodeling in aged rats. BMC Pharmacol Toxicol 18:29. https://doi.org/10.1186/s40360-017-0136-7
Choi ME, Ding Y, Kim SI (2012) TGF-β signaling via TAK1 pathway: role in kidney fibrosis. Semin Nephrol 32:244–252. https://doi.org/10.1016/j.semnephrol
Song L, Liu L, Wu Z, Li Y, Ying Z, Lin C, Wu J, Hu B, Cheng SY, Li M, Li J (2012) TGF-β induces miR-182 to sustain NF-κB activation in glioma subsets. J Clin Invest 122:3563–3578. https://doi.org/10.1172/JCI62339
Wu W, Chen F, Cui X, Yang L, Chen J, Zhao J, Huang D, Liu J, Yang L, Zeng J, Zeng Z, Pan Y, Su F, Cai J, Ying Z, Zhao Q, Song E, Su S (2018) LncRNA NKILA suppresses TGF-β-induced epithelial-mesenchymal transition by blocking NF-κB signaling in breast cancer. Int J Cancer 143:2213–2224. https://doi.org/10.1002/ijc.31605
Newman AC, Kemp AJ, Drabsch Y, Behrends C, Wilkinson S (2017) Autophagy acts through TRAF3 and RELB to regulate gene expression via antagonism of SMAD proteins. Nat Commun 8:1537. https://doi.org/10.1038/s41467-017-00859-z
Zheng W, Qian Y, Chen S, Ruan H, Fan C (2018) Rapamycin protects against peritendinous fibrosis through activation of autophagy. Front Pharmacol 9:402. https://doi.org/10.3389/fphar.2018.00402
Chang J, Hisamatsu T, Shimamura K, Yoneno K, Adachi M, Naruse H, Igarashi T, Higuchi H, Matsuoka K, Kitazume MT, Ando S, Kamada N, Kanai T, Hibi T (2013) Activated hepatic stellate cells mediate the differentiation of macrophages. Hepatol Res 43:658–669. https://doi.org/10.1111/j.1872-034X.2012.01111.x
Liaskou E, Zimmermann HW, Li KK, Oo YH, Suresh S, Stamataki Z, Qureshi O, Lalor PF, Shaw J, Syn WK, Curbishley SM, Adams DH (2013) Monocyte subsets in human liver disease show distinct phenotypic and functional characteristics. Hepatology 57:385–398. https://doi.org/10.1002/hep.26016
Kumar S, Enjamoori R, Jaiswal A, Ray R, Seth S, Maulik SK (2009) Catecholamine-induced myocardial fibrosis and oxidative stress is attenuated by Terminalia arjuna (Roxb.). J Pharm Pharmacol 61:1529–1536. https://doi.org/10.1211/jpp/61.11.0013
Radisky ES, Radisky DC (2010) Matrix metalloproteinase-induced epithelial–mesenchymal transition in breast cancer. J Mamm Gland Biol Neoplasia 15:201–212. https://doi.org/10.1007/s10911-010-9177-x
Dilly AK, Ekambaram P, Guo Y, Cai Y, Tucker SC, Fridman R, Kandouz M, Honn KV (2013) Platelet-type 12-lipoxygenase induces MMP9 expression and cellular invasion via activation of PI3K/Akt/NF-κB. Int J Cancer 133:1784–1791. https://doi.org/10.1002/ijc.28165
Argüelles JC (2014) Why can’t vertebrates synthesize trehalose? J Mol Evol 79:111–116. https://doi.org/10.1007/s00239-014-9645-9
Iturriaga G, Suárez R, Nova-Franco B (2009) Trehalose metabolism: from osmoprotection to signaling. Int J Mol Sci 10:3793–3810. https://doi.org/10.3390/ijms10093793
Purvis JE, Yomano LP, Ingram LO (2005) Enhanced trehalose production improves growth of Escherichia coli under osmotic stress. Appl Environ Microbiol 71:3761–3769. https://doi.org/10.1128/AEM.71.7.3761-3769.2005
Benaroudj N, Lee DH, Goldberg AL (2001) Trehalose accumulation during cellular stress protects cells and cellular proteins from damage by oxygen radicals. J Biol Chem 276:24261–24267. https://doi.org/10.1074/jbc.M101487200
Elbein AD, Pan YT, Pastuszak I, Carroll D (2003) New insights on trehalose: a multifunctional molecule. Glycobiology 13:17R–27R. https://doi.org/10.1093/glycob/cwg047
Elbein AD (1974) The metabolism of alpha, alpha-trehalose. Adv Carbohydr Chem Biochem 30:227–256. https://doi.org/10.1016/s0065-2318(08)60266-8
Tanaka M, Machida Y, Niu S, Ikeda T, Jana NR, Doi H, Kurosawa M, Nekooki M, Nukina N (2004) Trehalose alleviates polyglutamine-mediated pathology in a mouse model of Huntington disease. Nat Med 10:148–154. https://doi.org/10.1038/nm985
Sarkar S, Chigurupati S, Raymick J, Mann D, Bowyer JF, Schmitt T, Beger RD, Hanig JP, Schmued LC, Paule MG (2014) Neuroprotective effect of the chemical chaperone, trehalose in a chronic MPTP-induced Parkinson’s disease mouse model. Neurotoxicology 44:250–262. https://doi.org/10.1016/j.neuro.2014.07.006
Singer MA, Lindquist S (1998) Multiple effects of trehalose on protein folding in vitro and in vivo. Mol Cell 1:639–648. https://doi.org/10.1016/s1097-2765(00)80064-7
Crowe JH, Tablin F, Wolkers WF, Gousset K, Tsvetkova NM, Ricker J (2003) Stabilization of membranes in human platelets freeze-dried with trehalose. Chem Phys Lipids 122:41–52. https://doi.org/10.1016/s0009-3084(02)00177-9
Lu F, Sun X, Xu X, Jiang X (2020) SILAC-based proteomic profiling of the suppression of TGF-β1-induced lung fibroblast-to-myofibroblast differentiation by trehalose. Toxicol Appl Pharmacol 391:114916. https://doi.org/10.1016/j.taap.2020.114916
Fujino H, Lee S, Suzuki S, Chung UI, Mochizuki M, Nishimura R, Sasaki N (2011) Trehalose may prevent postsurgical adhesions in a rabbit model of hysterotomy. J Vet Med Sci 73:931–935. https://doi.org/10.1292/jvms.10-0342
Ohata A, Tamura N, Iwata K, Abe N, Doi K, Saito Y, Katoh M, Nojima H (2014) Trehalose solution protects mesothelium and reduces bowel adhesions. J Surg Res 191:224–230. https://doi.org/10.1016/j.jss.2014.03.077
Acknowledgements
The study was supported by the National Key R&D Program of China (2018YFC1106100, 2018YFC1106101), the National Natural Science Foundation of China (Grant Nos. 81770888, 81800873, 31800809 and 31500835), the Shanghai Municipal Education Commission-Gaofeng Clinical Medicine Grant Support (Grant no. 20161421), the Science and Technology Commission of Shanghai Grant (Grant no. 17411963800 and 19JC1411703), Shanghai Pujiang Program (18PJD025), Shanghai Jiao Tong University School of Medicine Two-hundred Talent (20191914).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wu, N., Chen, L., Yan, D. et al. Trehalose attenuates TGF-β1-induced fibrosis of hSCFs by activating autophagy. Mol Cell Biochem 470, 175–188 (2020). https://doi.org/10.1007/s11010-020-03760-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11010-020-03760-4