Abstract
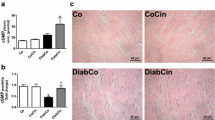
The contractile hyporesponsiveness of the streptozotocin diabetic rat heart in vitro to β-adrenergic agonists is eliminated when the heart is perfused with NG-nitro-l-arginine methyl ester (l-NAME), a non-selective inhibitor of nitric oxide synthase (NOS). The following study evaluated the hypothesis that an increased production of NO/cGMP within the diabetic myocyte inhibits the β-adrenergic-stimulated increase in calcium current and contractile response. Male Sprague-Dawley rats were given an intravenous injection of streptozotocin (60 mg/kg). After 8 weeks, L-type calcium currents were recorded in ventricular myocytes using the whole cell voltage-clamp method. Shortening of isolated myocytes was determined using a video edge detection system. cAMP and cGMP were measured using radioimmunoassay. Nitric oxide production was determined using the Griess assay kit. Basal cGMP levels and nitric oxide production were elevated in diabetic myocytes. Shortening of the diabetic myocytes in response to isoproterenol (1 μM) was markedly diminished. However, there was no detectable difference in the isoproterenol-stimulated L-type calcium current or cAMP levels between control and diabetic myocytes. Acute superfusion of the diabetic myocyte with l-NAME (1 mM) decreased basal cGMP and markedly enhanced the shortening response to isoproterenol but did not alter isoproterenol-stimulated calcium current. These data suggest that increased production of NO/cGMP within the diabetic myocyte suppressed β-adrenergic stimulated shortening of the myocyte. However, NO/cGMP apparently does not suppress shortening of the myocyte by inhibition of the β-stimulated calcium current.






Similar content being viewed by others
References
Tomlinson KC, Gardiner SM, Hebden RA, Bennett T (1992) Functional consequences of streptozotocin-induced diabetes mellitus, with particular reference to the cardiovascular system. Pharmacol Rev 44:103–150
Rodrigues B, McNeill JH (1992) The diabetic heart: metabolic causes for the development of a cardiomyopathy. Cardiovasc Res 26:913–922
Vadlamudi RV, McNeill JH (1984) Effects of experimental diabetes on isolated rat heart responsiveness to isoproterenol. Can J Physiol Pharmacol 62:124–131
Heller BA, Paulson DJ, Kopp SJ, Peace DG, Tow JV (1988) Depressed in vivo myocardial reactivity to dobutamine in streptozotocin diabetic rat: influence of exercise training. Cardiovasc Res 22:417–424
Smith JM, Paulson DJ, Romano FD (1997) Inhibition of nitric oxide synthase by l-NAME improves ventricular performance in streptozotocin-diabetic rats. J Mol Cell Cardiol 29:2393–2402
Gando S, Hattori Y, Akaishi Y, Nishihira J, Kanno M (1997) Impaired contractile response to beta adrenoceptor stimulation in diabetic rat hearts: alterations in beta adrenoceptor-G protein-adenylate cyclase system and phospholamban phosphorylation. J Pharmacol Exp Ther 282:475–484
Horackova M, Murphy MG (1988) Effects of chronic diabetes mellitus on the electrical and contractile activities, 45Ca2+ transport, fatty acid profiles and ultrastructure of isolated rat ventricular myocytes. Pflugers Arch 411:564–572
Tamada A, Hattori Y, Houzen H, Yamada Y, Sakuma I, Kitabatake A, Kanno M (1988) Effects of β-adrenoceptor stimulation on contractility, [Ca2+]i, and Ca2+ current in diabetic rat cardiomyocytes. Am J Physiol 274:H1849–H1857
Rees DD, Palmer RMJ, Schulz R, Hodson HF, Moncada S (1990) Characterization of three inhibitors of endothelial nitric oxide synthase in vitro and in vivo. Br J Pharmacol 101:746–752
Griffith OW, Stuehr J (1995) Nitric oxide synthases: properties and catalytic mechanism. Ann Rev Physiol 57:707–736
Balligand JL, Cannon PJ (1997) Nitric oxide synthases and cardiac muscle. Arterioscler Thromb Vasc Biol 17:1846–1858
Kelly RA, Balligand JL, Smith TW (1996) Nitric oxide and cardiac function. Circ Res 79:363–380
Ursell PC, Mayes M (1995) Anatomic distribution of nitric oxide synthase in the heart. Int J Cardiol 50:217–223
Balligand JL (1999) Regulation of cardiac β-adrenergic response by nitric oxide. Cardiovasc Res 43:607–620
Rozanski GJ, Witt RC (1994) IL-1 inhibits β-adrenergic control of cardiac calcium current: role of l-arginine/nitric oxide pathway. Am J Physiol 67:H1753–H1758
Wahler GM, Dollinger SM (1995) Nitric oxide donor SIN-1 inhibits mammalian cardiac calcium current through cGMP-dependent protein kinase. Am J Physiol 268:C45–C54
Sumii K, Sperelakis N (1995) cGMP-dependent protein kinase regulation of L-type Ca2+current in rat ventricular myocytes. Circ Res 77:803–812
Barouch LA, Harrison RW, Skaf MW, Rosas GO, Cappola TP, Kobeissi ZA, Hobai IA, Lemmon CA, Burnett AL, O’Rourke B, Rodriguez ER, Huang PL, Lima JAC, Berkowitz DE, Hare JM (2002) Nitric oxide regulates the heart by spatial confinement of nitric oxide synthase isoforms. Nature 416:337–340
Paulson DJ, Crass MF III (1982) Endogenous triacylglycerol metabolism in the diabetic heart. Am J Physiol 242:H1084–H1094
Yazawa K, Kaibara M, Ohara M, Kameyama M (1990) An improved method for isolating cardiac myocytes useful for patch-clamp studies. Jpn J Physiol 40:157–163
MacKenzie A, Wadsworth RM (2003) Extracellular l-arginine is required for optimal NO synthesis by eNOS and iNOS in the rat mesenteric artery wall. Br J Pharmacol 139:1487–1497
Shen LJ, Beloussow K, Shen WC (2005) Accessibility of endothelial and inducible nitric oxide synthase to the intracellular citrulline–arginine regeneration pathway. Biochem Pharmacol 69:97–104
Steadmann BW, Moore KB, Spitzer KW, Bridge JHB (1988) A video system for measuring motion in contracting heart cells. Inst Electr Eng Trans Biomed Eng 35:264–272
Ziolo MT, Dollinger SJ, Wahler GM (1998) Myocytes isolated from rejecting transplanted rat hearts exhibit reduced basal shortening which is reversible by aminoguanidine. J Mol Cell Cardiol 30:1009–1017
Cheng X, Cheng XS, Kuo-Hsing K, Pang CCY (2004) Inhibition of iNOS augments cardiovascular action of noradrenaline in streptozotocin-induced diabetes. Cardiovas Res 64:298–307
Nagareddy PR, Zhengyuan X, McNeill JH, MacLeod KM (2005) Increased expression of iNOS is associated with endothelial dysfunction and impaired pressor responsiveness in streptozotocin-induced diabetes. Am J Physiol 289:H2144–H2152
Kinugawa K-I, Kohmoto O, Atsushi Y, Serizawa T, Takahashi T (1997) Cardiac inducible nitric oxide synthase negatively modulates myocardial function in cultured rat myocytes. Am J Physiol 272:H35–H47
Yamamoto S, Tsutsui H, Tagawa H, Saito K, Takahashi M, Tada H, Yamamoto M, Katoh M, Egashira K, Takeshita A (1997) Role of myocyte nitric oxide in β-adrenergic hyporesponsiveness in heart failure. Circulation 95:1111–1114
Joe EK, Schussheim AE, Longrois D, Maki T, Kelly RA, Smith TW, Balligand JL (1998) Regulation of cardiac myocyte contractile function by inducible nitric oxide synthase (iNOS): mechanisms of contractile depression by nitric oxide. J Mol Cell Cardiol 30:303–315
Balligand JL, Ungureanu D, Kelly RA, Lobzik L, Pimental D, Smith MT, Smith TW (1993) Abnormal contractile function due to induction of nitric oxide synthesis in rat cardiac myocytes follows exposure to activated macrophage-conditioned medium. J Clin Invest 91:2314–2319
Ungureanu-Longrois D, Balligand JL, Simmons WW, Okada I, Kobzik L, Lowenstein CJ, Kunkel SL, Michel T, Kelly RA, Smith TW (1995) Induction of nitric oxide synthase activity by cytokines in ventricular myocytes is necessary but not sufficient to decrease contractile responsiveness to β-adrenergic agonists. Circ Res 77:494–502
Vila-Petroff MG, Younes A, Egan J, Lakatta EG, Sollott SJ (1999) Activation of distinct cAMP-dependent and cGMP-dependent pathways by nitric oxide in cardiac myocytes. Circ Res 84:1020–1031
Bardell AL, MacLeod KM (2001) Evidence for inducible nitric-oxide synthase expression and activity in vascular smooth muscle of streptozotocin-diabetic rats. J Pharmacol Exp Ther 296:252–259
Tannous M, Rabini RA, Vignini A, Moretti N, Fumelli P, Zielinski B, Mazzanti L, Mutus B (1999) Evidence for iNOS-dependent peroxynitrite production in diabetic platelets. Diabetologia 42:539–544
Stockklauser-Farber K, Ballhausen T, Laufer A, Rosen P (2000) Influence of diabetes on cardiac nitric oxide synthase expression and activity. Biochim Biophys Acta 1535:10–20
Kojda G, Kottenberg K (1999) Regulation of basal myocardial function by NO. Cardiovas Res 41:514–523
Hare JM (2003) Nitric oxide and excitation–contraction coupling. J Mol Cell Cardiol 35:719–729
Hove-Madsen L, Mery PF, Jurevicius J, Skeberdis AV, Rischmeister R (1996) Regulation of myocardial calcium channels by cyclic AMP metabolism. Basic Res Cardiol 91(Suppl 2):1–8
Leone RJ, Straznicka M, Scholz PM, Weiss HR (2000) Cyclic GMP attenuates cyclic AMP-stimulated inotropy and oxygen consumption in control and hypertrophic hearts. Basic Res Cardiol 95:28–38
Wichelhaus A, Russ M, Petersen S, Eckel J (1994) G protein expression and adenylate cyclase regulation in ventricular cardiomyocytes from STZ-diabetic rats. Am J Physiol 267:H548–H555
Yu Z, Quamme GA, McNeill JH (1994) Depressed [Ca2+] responses to isoproterenol and cAMP in isolated cardiomyocytes from experimental diabetic rats. Am J Physiol 266:H2334–H2342
Jiang LH, Gawler DJ, Hodson N, Milligan CJ, Pearson HA, Porter V, Wray D (2000) Regulation of cloned cardiac L-type calcium channels by cGMP-dependent protein kinase. J Biol Chem 275:6135–6143
Tsuchida K, Watajima H, Otomo S (1994) Calcium current in rat diabetic ventricular myocytes. Am J Physiol 267:H2280–H2289
Chattou S, Diacono J, Feuvray D (1999) Decrease in sodium–calcium exchange and calcium currents in diabetic rat ventricular myocytes. Acta Physiol Scand 166:137–144
Kawamura A, Wahler GM (1994) Perforated-patch recording does not enhance the effect of isobutylmethylxanthine on the cardiac calcium current. Am J Physiol 266:C1619–C1627
Ziolo MT, Harshbarger CH, Roycroft KE, Smith JM, Romano FD, Sondgeroth KL, Wahler GM (2001): Myocytes isolated from rejecting transplanted rat hearts exhibit a nitric oxide-mediated reduction in the calcium current. J Mol Cell Cardiol 33:1691–1699
Xu YW, Huso DL, Dawson TM, Bredt DS, Becker LC (1999) Nitric oxide synthase in cardiac sarcoplasmic reticulum. Proc Natl Acad Sci USA 96:657–662
Stojanovic WC, Wolska BM, Wahler GM, Solaro RJ (1996) Effects of nitric oxide on protein phosphorylation in rat cardiomyocytes. Biophys J 70:A392 (Abstract)
Shah AM, Spurgeon HA, Sollott SJ, Talo A, Lakatta EG (1994) 8-bromo-cGMP reduces the myofilament response to Ca2+ in intact cardiac myocytes. Circ Res 74:970–978
Ziolo MT, Katoh H, Bers DM (2001) Expression of inducible nitric oxide synthase depresses β-adrenergic stimulated calcium release from the sarcoplasmic reticulum in intact ventricular myocytes. Circulation 104:2961–2966
Yu Z, Tibbits GF, McNeil JH (1994) Cellular functions of diabetic cardio-myocytes: contractility, rapid-cooling contracture, and ryanodine binding. Am J Physiol 266:H2082–H2089
Ganguly PK, Pierce GN Dhalla KS, Dhalla NS (1983) Defective sarcoplasmic reticular calcium transport in diabetic cardiomyopathy. Am J Physiol 244:E528–E535
Penpargkul S, Fein F, Sonnenblick EH, Scheuer J (1981) Depressed cardiac sarcoplasmic reticular function from diabetic rats. J Mol Cell Cardiol 13:303–309
Lagadic-Gossmann D, Buckler KJ, Le Prigent K, Feuvray D (1996) Altered Ca2+ handling in ventricular myocytes isolated from diabetic rats. Am J Physiol 270:H1529–H1537
Pierce GN, Russell JC (1997) Regulation of intracellular Ca2+in the heart during diabetes. Cardiovas Res 34:41–47
Weiss HR, Sadoff JD, Scholz PM, Klabunde RE (1997) Nitric oxide reduces myocardial contractility in isoproterenol-stimulated rat hearts by a mechanism independent of cyclic GMP or cyclic AMP. Pharmacol 55:202–210
Sandirasegarane L, Diamond J (1999) The nitric oxide donors, SNAP and DEA/NO, exert a negative inotropic effect in rat cardiomyocytes which is independent of cyclic GMP elevation. J Mol Cell Cardiol 31:799–808
Stambler JS (1994) Redox signaling: nitrosylation and related target interactions of nitric oxide. Cell 78:931–936
Vedia LM, McDonald B, Reep B, Brune B, Di Silvio M, Billiar TR, Lapetina EG (1992) Nitric oxide-induced S-nitrosylation of glyceraldehyde-3-phosphate dehydrogenase inhibits enzymatic activity and increases endogenous ADP-ribosylation. J Biol Chem 267:24929–24932
Recchia FA, McConnell PI, Loke KE, Xiaobin X, Ochoa M, Hintze TH (1999) Nitric oxide controls cardiac substrate utilization in the conscious dog. Cardiovas Res 44:325–332
Schulz R, Dodge KL, Lopaschuk GD, Clanachan AS (1997) Peroxynitrite impairs cardiac contractile function by decreasing cardiac efficiency. Am J Physiol 272:H1212–H1219
Acknowledgements
Funding for this grant was provided by the Max Goldenberg Foundation, NIH grant R15 HL/OD56356-01 and Midwestern University.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Smith, J.M., Sondgeroth, K.B. & Wahler, G.M. Inhibition of nitric oxide synthase enhances contractile response of ventricular myocytes from streptozotocin-diabetic rats. Mol Cell Biochem 300, 129–137 (2007). https://doi.org/10.1007/s11010-006-9376-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11010-006-9376-3