Abstract
Objectives
Stillbirth is an important health problem, and in Mexico, only half of the stillbirths have an explainable cause. The aim of this study was to implement a multidisciplinary workup to identify the etiology and potential risk factors for stillbirth at the Hospital Universitario “Dr. José Eleuterio González”.
Methods
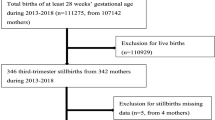
This is a prospective, descriptive, observational study that included stillbirths from the Obstetrics Service from October 1st, 2019 to May 25, 2020. Evaluation strategies included a complete maternal medical history, physical examination of the fetus, and a photographic medical record. For every stillbirth either a prenatal ultrasound, a postnatal x-ray, or a fetal autopsy, were needed. Multiplex Ligation Probe Amplification (MLPA) was performed with an umbilical cord sample.
Results
Thirty-three stillbirths were reported; 21 were included in the analysis. Eleven women (52.3%) had known risk factors for stillbirth, mainly elevated body mass index and diabetes. On physical examination, external birth defects were found in 8 fetuses (38%). X-ray was performed in 14 cases (66%), alterations were detected as a probable etiologic cause just in one. All cases underwent MLPA, which were reported negative. Three cases had criteria for autopsy. Findings were inconclusive to determine etiology.
Conclusions
The best tools for evaluation of stillbirth were the elaboration of clinical history, physical examination, and prenatal ultrasound. Diabetes and obesity were the most frequent risk factors found in our population. These factors are preventable by implementing strategies that lead to better prenatal care.
Significance
Stillbirth is a health problem whose causes are rarely evaluated and explained to the families that go through this situation. To completely explain the causes of stillbirth a complete workup should be performed, where a multidisciplinary participation is needed. Mainly these workups have been performed retrospectively, however we introduce a complete evaluation of stillbirth since the moment of arrival to obstetrics department and performing evaluations for fetal, maternal or combined causes, including genetic testing; detecting key health issues in our population, that can be prevented with an adequate prenatal care.

Similar content being viewed by others
Data Availability
Data are available upon reasonable request.
Code Availability
Not applicable.
References
Aminu, M., Bar-Zeev, S., & van den Broek, N. (2017). Cause of and factors associated with stillbirth: A systematic review of classification systems. Acta Obstetricia et Gynecologica Scandinavica, 96(5), 519–528.
Aune, D., Saugstad, O. D., Henriksen, T., & Tonstad, S. (2014). Maternal body mass index and the risk of fetal death, stillbirth, and infant death: A systematic review and meta-analysis. JAMA: The Journal of the American Medical Association, 311(15), 1536–1546.
Bradley, R. J., Brudenell, J. M., & Nicolaides, K. H. (1991). Fetal acidosis and hyperlacticaemia diagnosed by cordocentesis in pregnancies complicated by maternal diabetes mellitus. Diabetic Medicine: A Journal of the British Diabetic Association, 8(5), 464–468.
Bukowski, R., Hansen, N. I., Pinar, H., Willinger, M., Reddy, U. M., Parker, C. B., Silver, R. M., Dudley, D. J., Stoll, B. J., Saade, G. R., Koch, M. A., Hogue, C., Varner, M. W., Conway, D. L., Coustan, D., Goldenberg, R. L., Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) Stillbirth Collaborative Research Network (SCRN). (2017). Altered fetal growth, placental abnormalities, and stillbirth. PloS one, 12(8), e0182874.
Castro, D. M. (2012). Alteraciones genéticas y estrategias diagnósticas en muerte fetal. Ginecología y Obstetricia de México, 80, 313–319.
Cheong-See, F., Schuit, E., Arroyo-Manzano, D., Khalil, A., Barrett, J., Joseph, K. S., Asztalos, E., Hack, K., Lewi, L., Lim, A., Liem, S., Norman, J. E., Morrison, J., Combs, C. A., Garite, T. J., Maurel, K., Serra, V., Perales, A., Rode, L., Global Obstetrics Network (GONet) Collaboration. (2016). Prospective risk of stillbirth and neonatal complications in twin pregnancies: Systematic review and meta-analysis. BMJ, 354, i4353.
Dudley, D. J. (2007). Diabetic-associated stillbirth: incidence, pathophysiology, and prevention. Clinics in Perinatology, 34(4), 611–626.
Flenady, V., Koopmans, L., Middleton, P., Frøen, J. F., Smith, G. C., Gibbons, K., Coory, M., Gordon, A., Ellwood, D., McIntyre, H. D., Fretts, R., & Ezzati, M. (2011). Major risk factors for stillbirth in high-income countries: A systematic review and meta-analysis. The Lancet, 377(9774), 1331–1340.
Gardosi, J., Madurasinghe, V., Williams, M., Malik, A., & Francis, A. (2013). Maternal and fetal risk factors for stillbirth: Population based study. BMJ, 346(jan24.3), 108–108. https://doi.org/10.1136/bmj.f108
Gestations, M. (2021). Twin, Triplet, and higher-order multifetal pregnancies: ACOG practice bulletin summary, number 231. Obstetrics and Gynecology, 137(6), 1140–1143.
Hernández-Herrera, R. J., Alcalá-Galván, L. G., Castillo-Martínez, N. E., Flores-Santos, R., Cortés-Flores, R., & Buenrostro-Lozano, A. (2009). A 35 year period review of the perinatal mortality in a gynecology-obstetric unit. Revista Medica del Instituto Mexicano del Seguro Social, 47(4), 353–356.
Holmes, L. B., Nasri, H., Beroukhim, R., Hunt, A.-T., Roberts, D. J., Hassan Toufaily, M., & Westgate, M.-N. (2018). Stillborn infants: Associated malformations. In Birth Defects Research, 110(2), 114–121. https://doi.org/10.1002/bdr2.1097
Hug, L., You, D., Blencowe, H., Mishra, A., Wang, Z., Fix, M. J., Wakefield, J., Moran, A. C., Gaigbe-Togbe, V., Suzuki, E., Blau, D. M., Cousens, S., Creanga, A., Croft, T., Hill, K., Joseph, K. S., Maswime, S., McClure, E. M., Pattinson, R., UN Inter-agency Group for Child Mortality Estimation and its Core Stillbirth Estimation Group. (2021). Global, regional, and national estimates and trends in stillbirths from 2000 to 2019: A systematic assessment. The Lancet, 398(10302), 772–785.
López-Uriarte, A., & Aguinaga-Ríos, M. (2012). Discordancia de defectos congénitos en recién nacidos de embarazos múltiples en el Instituto Nacional de Perinatología. Perinatología y Reproducción Humana, 26(1), 08–16.
Lord, J., McMullan, D. J., Eberhardt, R. Y., Rinck, G., Hamilton, S. J., Quinlan-Jones, E., Prigmore, E., Keelagher, R., Best, S. K., Carey, G. K., Mellis, R., Robart, S., Berry, I. R., Chandler, K. E., Cilliers, D., Cresswell, L., Edwards, S. L., Gardiner, C., Henderson, A., Prenatal Assessment of Genomes and Exomes Consortium. (2019). Prenatal exome sequencing analysis in fetal structural anomalies detected by ultrasonography (PAGE): A cohort study. The Lancet, 393(10173), 747–757.
Malacova, E., Tippaya, S., Bailey, H. D., Chai, K., Farrant, B. M., Gebremedhin, A. T., Leonard, H., Marinovich, M. L., Nassar, N., Phatak, A., Raynes-Greenow, C., Regan, A. K., Shand, A. W., Shepherd, C. C. J., Srinivasjois, R., Tessema, G. A., & Pereira, G. (2020). Stillbirth risk prediction using machine learning for a large cohort of births from Western Australia, 1980–2015. In Scientific Reports. https://doi.org/10.1038/s41598-020-62210-9
Man, J., Hutchinson, J. C., Heazell, A. E., Ashworth, M., Levine, S., & Sebire, N. J. (2016). Stillbirth and intrauterine fetal death: Factors affecting determination of cause of death at autopsy. Ultrasound in Obstetrics & Gynecology: The Official Journal of the International Society of Ultrasound in Obstetrics and Gynecology, 48(5), 566–573.
Murguía-Peniche, T., Illescas-Zárate, D., Chico-Barba, G., & Bhutta, Z. A. (2016). An ecological study of stillbirths in Mexico from 2000 to 2013. Bulletin of the World Health Organization, 94(5), 322-330A.
Page, J. M., Bardsley, T., Thorsten, V., Allshouse, A. A., Varner, M. W., Debbink, M. P., Dudley, D. J., Saade, G. R., Goldenberg, R. L., Stoll, B., Hogue, C. J., Bukowski, R., Conway, D., Reddy, U. M., & Silver, R. M. (2019). Stillbirth associated with infection in a diverse U.S. cohort. In Obstetrics & Gynecology, 134(6), 1187–1196. https://doi.org/10.1097/aog.0000000000003515
Page, J. M., Christiansen-Lindquist, L., Thorsten, V., Parker, C. B., Reddy, U. M., Dudley, D. J., Saade, G. R., Coustan, D., Rowland Hogue, C. J., Conway, D., Bukowski, R., Pinar, H., Heuser, C. C., Gibbins, K. J., Goldenberg, R. L., & Silver, R. M. (2017). Diagnostic tests for evaluation of stillbirth. In Obstetrics & Gynecology, 129(4), 699–706. https://doi.org/10.1097/aog.0000000000001937
Pauli, R. M., & Reiser, C. A. (1994). Wisconsin Stillbirth service program: II. Analysis of diagnoses and diagnostic categories in the first 1000 referrals. American Journal of Medical Genetics, 50(2), 135–153.
Pinar, H., Koch, M., Hawkins, H., Heim-Hall, J., Abramowsky, C., Thorsten, V., Carpenter, M., Zhou, H., & Reddy, U. (2012). The stillbirth collaborative research network postmortem examination protocol. In American Journal of Perinatology, 29(03), 187–202. https://doi.org/10.1055/s-0031-1284228
Reddy, U. M., Page, G. P., Saade, G. R., Silver, R. M., Thorsten, V. R., Parker, C. B., Pinar, H., Willinger, M., Stoll, B. J., Heim-Hall, J., Varner, M. W., Goldenberg, R. L., Bukowski, R., Wapner, R. J., Drews-Botsch, C. D., O’Brien, B. M., Dudley, D. J., Levy, B., NICHD Stillbirth Collaborative Research Network. (2012). Karyotype versus microarray testing for genetic abnormalities after stillbirth. The New England Journal of Medicine, 367(23), 2185–2193.
Rosenfeld, J. A., Tucker, M. E., Escobar, L. F., Neill, N. J., Torchia, B. S., McDaniel, L. D., Schultz, R. A., Chong, K., & Chitayat, D. (2015). Diagnostic utility of microarray testing in pregnancy loss. Ultrasound in Obstetrics & Gynecology: The Official Journal of the International Society of Ultrasound in Obstetrics and Gynecology, 46(4), 478–486.
Rosenstein, M. G., Cheng, Y. W., Snowden, J. M., Nicholson, J. M., Doss, A. E., & Caughey, A. B. (2012). The risk of stillbirth and infant death stratified by gestational age in women with gestational diabetes. American Journal of Obstetrics and Gynecology, 206(4), 309.e1-e7.
Silver, R. M., Varner, M. W., Reddy, U., Goldenberg, R., Pinar, H., Conway, D., Bukowski, R., Carpenter, M., Hogue, C., Willinger, M., Dudley, D., Saade, G., & Stoll, B. (2007). Work-up of stillbirth: A review of the evidence. In American Journal of Obstetrics and Gynecology, 196(5), 433–444. https://doi.org/10.1016/j.ajog.2006.11.041
Stacey, T., Tennant, P., McCowan, L., Mitchell, E. A., Budd, J., Li, M., Thompson, J., Martin, B., Roberts, D., & Heazell, A. (2019). Gestational diabetes and the risk of late stillbirth: A case-control study from England, UK. BJOG: An International Journal of Obstetrics and Gynaecology, 126(8), 973–982.
Tavares Da Silva, F., Gonik, B., McMillan, M., Keech, C., Dellicour, S., Bhange, S., Tila, M., Harper, D. M., Woods, C., Kawai, A. T., Kochhar, S., Munoz, F. M., Brighton Collaboration Stillbirth Working Group. (2016). Stillbirth: Case definition and guidelines for data collection, analysis, and presentation of maternal immunization safety data. Vaccine, 34(49), 6057–6068.
Tennant, P. W. G., Glinianaia, S. V., Bilous, R. W., Rankin, J., & Bell, R. (2014). Pre-existing diabetes, maternal glycated haemoglobin, and the risks of fetal and infant death: A population-based study. Diabetologia, 57(2), 285–294.
Tomlinson, A. J., Martindale, E., Bancroft, K., & Heazell, A. (2018). Improved management of stillbirth using a care pathway. In International Journal of Health Governance, 23(1), 18–37. https://doi.org/10.1108/ijhg-09-2017-0045
Visintin, C., Mugglestone, M. A., James, D., Kilby, M. D., Guideline Development Group. (2011). Antenatal care for twin and triplet pregnancies: summary of NICE guidance. BMJ, 343, d5714.
Whitworth, M., Bricker, L., & Mullan, C. (2015). Ultrasound for fetal assessment in early pregnancy. Cochrane Database of Systematic Reviews, 7, CD007058.
Wojcik, M. H., Brodsky, D., Stewart, J. E., & Picker, J. (2018). Peri-mortem evaluation of infants who die without a diagnosis: Focus on advances in genomic technology. Journal of Perinatology: Official Journal of the California Perinatal Association, 38(9), 1125–1134.
Funding
The project was funded with resources of the Genetics Department as well as the Radiology and Pathology Departments of the Hospital Universitario “Dr. José Eleuterio González,” Universidad Autónoma de Nuevo León.
Author information
Authors and Affiliations
Contributions
KR-E: Project development, sample collection, patient evaluation, data collection, tissue processing, data analysis, manuscript writing. GAL-U: Project development, data analysis, manuscript writing/editing. GBG-C: Tissue processing. IT-M: Tissue processing and analysis. JJL-T: Tissue processing and analysis. GE-R: Project development OB-Q: Project Development MP-C: Project Development AG-L: Project Development LMV: Project development, data analysis, manuscript writing/editing.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical Approval
The study was approved by the Ethics Committee of the Facultad de Medicina and Hospital Universitario, Universidad Autónoma de Nuevo León with registration number GN19-00004.
Consent to Participate
Participants provided written consents for participation, use and storage of tissue samples.
Consent for Publication
Participants provided written consent explaining protocol and usage of data for publication.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Robles Espinoza, K., López Uriarte, G.A., García Castañeda, G.B. et al. Multidisciplinary Workup for Stillbirth at a Tertiary-Care Hospital in Northeast Mexico: Findings, Challenges and Perspectives. Matern Child Health J 28, 1072–1079 (2024). https://doi.org/10.1007/s10995-023-03874-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-023-03874-3