Abstract
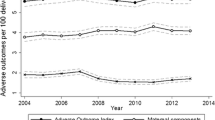
Purpose Describe how Ohio and Massachusetts explored severe maternal morbidity (SMM) data, and used these data for increasing awareness and driving practice changes to reduce maternal morbidity and mortality. Description For 2008–2013, Ohio used de-identified hospital discharge records and International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) codes to identify delivery hospitalizations. Massachusetts used existing linked data system infrastructure to identify delivery hospitalizations from birth certificates linked to hospital discharge records. To identify delivery hospitalizations complicated by one or more of 25 SMMs, both states applied an algorithm of ICD-9-CM diagnosis and procedure codes. Ohio calculated a 2013 SMM rate of 144 per 10,000 delivery hospitalizations; Massachusetts calculated a rate of 162. Ohio observed no increase in the SMM rate from 2008 to 2013; Massachusetts observed a 33% increase. Both identified disparities in SMM rates by maternal race, age, and insurance type. Assessment Ohio and Massachusetts engaged stakeholders, including perinatal quality collaboratives and maternal mortality review committees, to share results and raise awareness about the SMM rates and identified high-risk populations. Both states are applying findings to inform strategies for improving perinatal outcomes, such as simulation training for obstetrical emergencies, licensure rules for maternity units, and a focus on health equity. Conclusion Despite data access differences, examination of SMM data informed public health practice in both states. Ohio and Massachusetts maximized available state data for SMM investigation, which other states might similarly use to understand trends, identify high risk populations, and suggest clinical or population level interventions to improve maternal morbidity and mortality.


Similar content being viewed by others
References
American College of Obstetricians and Gynecologists. (2015). Obstetric care consensus No. 2: Levels of maternal care. Obstetrics and Gynecology, 125, 502–515.
American College of Obstetricians and Gynecologists. (2016). Obstetric care consensus no. 5: Severe maternal morbidity: Screening and review. Obstetrics and Gynecology, 128(3), e54–e60.
Bateman, B. T., Mhyre, J. M., Hernandez-Diaz, S., et al. (2013). Development of a comorbidity index for use in obstetric patients. Obstetrics and Gynecology, 122(5), 957–965.
Brown, H. L., Small, M., Taylor, Y. J., Chireau, M., & Howard, D. L. (2011). Near miss mortality in a multi-ethnic population. Annals of Epidemiology, 21(2), 73–77.
Building U.S. Capacity to Review and Prevent Maternal Deaths. (2018). Report from nine maternal mortality review committees. Retrieved from http://reviewtoaction.org/Report_from_Nine_MMRCs.
Callaghan, W. M. (2014). State-based maternal death reviews: Assessing opportunities to alter outcomes. American Journal of Obstetrics and Gynecology, 211(6), 581–582.
Callaghan, W. M., Creanga, A. A., & Kuklina, E. K. (2012). Severe maternal morbidity among delivery and postpartum hospitalizations in the United States. Obstetrics and Gynecology, 120(5), 1029–1036.
Callaghan, W. M., Grobman, W. A., Kilpatrick, S. J., Main, E. K., & D’Alton, M. (2014). Facility-based identification of women with severe maternal morbidity: it is time to start. Obstetrics and Gynecology, 123(5), 978–981.
Callaghan, W. M., MacKay, A. P., & Berg, C. J. (2008). Identification of severe maternal morbidity during delivery hospitalizations, United States, 1991–2003. American Journal of Obstetrics and Gynecology, 199(2), 133.e1–133.e8.
Creanga, A. A., Bateman, B. T., Kuklina, E. V., & Callaghan, W. M. (2014). Racial and ethnic disparities in severe maternal morbidity: A multi-state analysis, 2008–2010. American Journal of Obstetrics and Gynecology, 210(5), 435.e1–435.e8.
Geller, S. E., Cox, S. M., Callaghan, W. M., & Berg, C. J. (2006). Morbidity and mortality in pregnancy: Laying the groundwork for safe motherhood. Women’s Health Issues, 16(4), 176–188.
Geller, S. E., Rosenberg, D., Cox, S., Brown, M., Simonson, L., & Kilpatrick, S. (2004). A scoring system identified near-miss maternal morbidity during pregnancy. Journal of Clinical Epidemiology, 57(7), 716–720.
Goodman, D., Stampfel, C., Creanga, A. A., Callaghan, W. M., Callahan, T., Bonzon, E., et al. (2013). Revival of a core public health function: State- and urban-based maternal death review processes. Journal of Women’s Health, 22(5), 1–4.
Grobman, W. A., Bailit, J. L., Rice, M. M., Wapner, R. J., Reddy, U. M., Varner, M. W., et al. (2015). Racial and ethnic disparities in maternal morbidity and obstetric care. Obstetrics and Gynecology, 125(6), 1460–1467.
Healthy People 2020 Objective/Title V National Outcome Measure 2. Accessed on 12/15/2015 at http://mchb.hrsa.gov/programs/titlevgrants/blockgrantguidanceappendix.pdf.
Hinkle, S. N., Sharma, A. J., Kim, S. Y., et al. (2012). Prepregnancy obesity trends among low-income women, United States, 1999–2008. Maternal and Child Health Journal, 16(7), 1339–1348.
Howell, E. A., & Zeitlin, J. (2017). Improving hospital quality to reduce disparities in severe maternal morbidity and mortality. Seminars in Perinatology, https://doi.org/10.1053/j.semperi.2017.04.002.
Kilpatrick, S. J., Berg, C., Bernstein, P., Bingham, D., Delgado, A., Callaghan, W. M., et al. (2014). Standardized severe maternal morbidity review: Rationale and process. Obstetrics and Gynecology, 124(2), 361–366.
Kilpatrick, S. J., Prentice, P., Jones, R. L., & Geller, S. (2012). Reducing maternal deaths through state maternal mortality review. Journal of Women’s Health, 21(9), 905–909.
Kuklina, E. V., Whiteman, M. K., Hillis, S., Jamieson, D. J., Meikle, S. F., Posner, S. F., et al. (2008). An enhanced method for identifying obstetric deliveries: implications for estimating maternal morbidity. Maternal and Child Health Journal, 12(4), 469–477.
Main, E. K. (2012). Decisions required for operating a maternal mortality review committee: The California experience. Seminars in Perinatology, 36(1), 37–41.
Main, E. K., Abreo, A., McNulty, J., Gilbert, W., McNally, C., Poeltler, D., et al. (2015). Measuring severe maternal morbidity: validation of potential measures. American Journal of Obstetrics and Gynecology, 214(5), 643.e1–643.e10.
Main, E. K., Cape, V., Abreo, A., Vasher, J., Woods, A., Carpenter, A., et al. (2017). Reduction of severe maternal morbidity from hemorrhage using a state perinatal quality collaborative. Am Journal of Obstetrics and Gynecology, 216, 298.e1–298.e11.
Pettker, C. M., & Grobman, W. A. (2015). Obstetric safety and quality. Obstetrics & Gynecology, 126(1), 196–206.
Shellhaas, C., & Conrey, E. (2018). State-based review of maternal deaths: The Ohio experience. Clinical Obstetrics and Gynecology, 61(2), 332–339.
The Joint Commission. (2017). Sentinel Events (SE). https://www.jointcommission.org/assets/1/6/CAMH_SE_0717.pdf. Accessed 2 Jan 2018.
Acknowledgements
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention. The authors declare that they have no conflicts of interest. The authors would like to acknowledge Don Reed and Ayana Birhanu from the Ohio Department of Health for assistance with data analysis; Ron Benham, Karin Downs, Emily Lu, Tim Nielsen, and Xiaohui Cui from the Massachusetts Department of Public Health; the Ohio Hospital Association for access to data and review of findings, the CDC/MCHEP, UIC, CSTE, CDC/EIS.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts to declare.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Conrey, E.J., Manning, S.E., Shellhaas, C. et al. Severe Maternal Morbidity, A Tale of 2 States Using Data for Action—Ohio and Massachusetts. Matern Child Health J 23, 989–995 (2019). https://doi.org/10.1007/s10995-019-02744-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-019-02744-1