Abstract
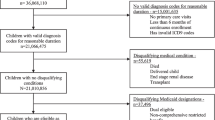
Objectives To examine the association between having a patient-centered medical home (PCMH) and healthcare expenditures and quality of care for children with special health care needs (CSHCN). Methods We conducted a cross-sectional analysis of 8802 CSHCN using the 2008–2012 Medical Expenditure Panel Survey. A PCMH indicator was constructed from survey responses. Inverse probability treatment weighting was applied to balance the cohort. CSHCN’s annual health care expenditures and quality were analyzed using two-part and logistic models, respectively. Results Covariate-adjusted annual total expenditures were similar between CSHCN with and without a PCMH ($4267 vs. $3957, p = 0.285). CSHCN with a PCMH had higher odds of incurring expenditure (OR 1.66, 95% CI 1.22–2.25)—in particular, office-based services and prescriptions (OR 1.46 and 1.36, 95% CI 1.24–1.72 and 1.17–1.58, respectively)—compared to those without a PCMH, without shifting expenditures. When examined in detail, PCMH was associated with lower odds of accessing office-based mental health services (OR 0.80, 95% CI 0.66–0.96), leading to lower expenditures ($106 vs. $137; p = 0.046). PCMH was associated with higher odds of post-operation and immunization visits (OR 1.23 and 1.22, 95% CI 1.05–1.45 and 1.004–1.48, respectively) without changing expenditures. Parents of CSHCN with a PCMH were more likely to report having the best health care quality (OR 2.33, p < 0.001). Conclusions CSHCN who had a PCMH experienced better health care quality and were more likely to access preventive services, with unchanged expenditures. However, they were less likely to use mental health services in office-based settings. As the effects of PCMH varied across services for CSHCN, more research is warranted.

Similar content being viewed by others
Notes
Nationwide Report from 2009/10 National Survey of Children with Special Health Care Needs. Retrieved from http://www.childhealthdata.org.
MEPS-HC Sample Design and Collection Process. Retrieved from http://www.meps.ahrq.gov/survey_comp/hc_data_collection.jsp.
Using Appropriate Price Indices for Analyses of Health Care Expenditures or income across multiple years. Retrieved from https://meps.ahrq.gov/about_meps/Price_Index.shtml.
References
Abdus, S., & Selden, T. M. (2013). Adherence with recommended well-child visits has grown, but large gaps persist among various socioeconomic groups. Health Affairs, 32(3), 508–515.
Ambler, G., Omar, R. Z., & Royston, P. (2007). A comparison of imputation techniques for handling missing predictor values in a risk model with a binary outcome. Statistical Methods in Medical Research, 16(3), 277–298.
American Academy of Family Physicians. (2008). Joint principles of the patient-centered medical home. Delaware Medical Journal, 80(1), 21.
An, R. (2016). Unmet Mental Health Care Needs in US Children with Medical Complexity, 2005–2010. Journal of Psychosomatic Research, 82, 1–3. https://doi.org/10.1016/j.jpsychores.2015.12.007.
Andersen, R. (1995). Revisiting the behavioral model and access to medical care: Does it matter? Journal of Health and Social Behavior, 36(1), 1–10.
Austin, P. C. (2011). An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behavioral Research, 46(3), 399–424.
Belotti, F., Deb, P., Manning, W. G., & Norton, E. C. (2015). twopm: Two-part models. Stata Journal, 15(1), 3–20.
Caldwell, J. B. T. (2013). Trends in well-child visits: United States, 2002–2009. Retrieved from http://meps.ahrq.gov/mepsweb/data_files/publications/st419/stat419.shtml.
Cooley, W. C., McAllister, J. W., Sherrieb, K., & Kuhlthau, K. (2009). Improved Outcomes associated with medical home implementation in pediatric primary care. Pediatrics, 124(1), 358–364. https://doi.org/10.1542/peds.2008-2600.
Deb, P., Manning, W., & Norton, E. (2006). Modeling health care costs and counts. Paper presented at the 8th World Congress on Health Economics.
Diedhiou, A., Probst, J. C., Hardin, J. W., Martin, A. B., & Xirasagar, S. (2010). Relationship Between presence of a reported medical home and emergency department use among children with asthma. Medical Care Research and Review, 67(4), 450–475. https://doi.org/10.1177/1077558710367735.
DuGoff, E. H., Schuler, M., & Stuart, E. A. (2014). Generalizing observational study results: Applying propensity score methods to complex surveys. Health Services Research, 49(1), 284–303.
Garcia-Huidobro, D., Shippee, N., Joseph-DiCaprio, J., O’Brien, J. M., & Svetaz, M. V. (2016). Effect of patient-centered medical home on preventive services for adolescents and young adults. Pediatrics, 137, e20153813.
Han, B., Yu, H., & Friedberg, M. W. (2017). Evaluating the impact of parent-reported medical home status on children’s health care utilization, expenditures, and quality: A difference-in-differences analysis with causal inference methods. Health Services Research, 52(2), 786–806.
Homer, C. J., Klatka, K., Romm, D., Kuhlthau, K., Bloom, S., Newacheck, P., … Perrin, J. M. (2008). A review of the evidence for the medical home for children with special health care needs. Pediatrics, 122(4), e922–e937.
McPherson, M., Arango, P., Fox, H., Lauver, C., McManus, M., Newacheck, P. W., … Strickland, B. (1998). A new definition of children with special health care needs. Pediatrics, 102(1 Pt 1), 137–140.
MEPS HC-155: 2012 Full Year Consolidated Data File. (2014). Retrieved from https://meps.ahrq.gov/data_stats/download_data/pufs/h155/h155doc.shtml.
MEPS HC-152G: 2012 Office-Based Medical Provider Visits. (2014). Retrieved from https://meps.ahrq.gov/data_stats/download_data/pufs/h152g/h152gdoc.shtml.
Miller, J. E., Nugent, C. N., Gaboda, D., & Russell, L. B. (2013). Reasons for unmet need for child and family health services among children with special health care needs with and without medical homes. PLoS ONE, 8(12), e82570. https://doi.org/10.1371/journal.pone.0082570.
Newacheck, P. W., & Kim, S. E. (2005). A national profile of health care utilization and expenditures for children with special health care needs. Archives of Pediatrics and Adolescent Medicine, 159(1), 10–17.
Olson, L. M., Tanner, J. L., Stein, M. T., & Radecki, L. (2008). Well-child care: Looking back, looking forward. Pediatric Annals. https://doi.org/10.3928/00904481-20080301-08.
Romaire, M. A., & Bell, J. F. (2010). The medical home, preventive care screenings, and counseling for children: Evidence from the medical expenditure panel survey. Academic Pediatrics, 10(5), 338–345.
Romaire, M. A., Bell, J. F., & Grossman, D. C. (2012). Medical home access and health care use and expenditures among children with special health care needs. Archives of Pediatrics and Adolescent Medicine, 166(4), 323–330. https://doi.org/10.1001/archpediatrics.2011.1154.
Sannicandro, T., Parish, S. L., Son, E., & Powell, R. M. (2016). Health care changes for children with special health care needs, 2005–2011. Maternal and Child Health Journal, 21, 1–7.
Strickland, B. B., Jones, J. R., Ghandour, R. M., Kogan, M. D., & Newacheck, P. W. (2011). The medical home: Health care access and impact for children and youth in the United States. Pediatrics, 127(4), 604–611.
The Children with Special Health Care Needs (CSHCN) Screener. (1998). Retrieved from http://www.cahmi.org/wp-content/uploads/2014/06/CSHCNS-Survey-and-scoring.pdf.
The Medical Home. (2002). Pediatrics, 110(1 Pt 1), 184–186.
Zuvekas, S. H., & Olin, G. L. (2009). Validating household reports of health care use in the medical expenditure panel survey. Health Services Research, 44(5 Pt 1), 1679–1700. https://doi.org/10.1111/j.1475-6773.2009.00995.x.
Funding
Funding was provided by Leonard D. Schaeffer Center for Health Policy and Economics (US) and Medica Research Institute.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Lin, CW., Romley, J.A. & Carlin, C. The Relationship Between the Patient-Centered Medical Homes, Healthcare Expenditures, and Quality of Care Among Children with Special Health Care Needs. Matern Child Health J 22, 1751–1760 (2018). https://doi.org/10.1007/s10995-018-2572-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-018-2572-4