Abstract
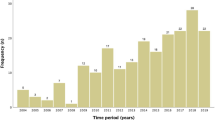
Objectives To describe a population choosing to continue with their pregnancy despite being eligible to receive a medical termination of pregnancy (TOP). Methods Nine-year retrospective study of data (01/01/2006 to 31/12/2014) from three French prenatal diagnostic centers describing the perinatal outcomes of these pregnancies. Pregnancies were classified according to etiology and severity of its fetal pathology. Several perinatal parameters were described: maternal characteristics, parental prenatal choices and information on the pregnancy and neonatal outcomes. These parameters were classified in function of the severity of fetal pathology according to the classification proposed by Dommergues et al. (Prenatal Diagnosis 30(6):531–539, 2010) Results Overall, 155 pregnancies were continued; 140 have been included in our study. Pregnancy outcomes consisted of four TOPs (2.9%); 20 in utero deaths (14.3%); 110 live births (78.6%) of which 55.4% were still alive at 2 years old as the most recent information; and 6 (4.2%) with unknown outcomes. In 27 cases, perinatal palliative care was requested (an increase of 37% over 9 years). 36.4% of cases were classified as having a high mortality risk; 19.3% with a severe handicap risk; 11.4% with a risk of isolated intellectual disability; and 32.9% with an uncertain prognosis. The parental decisions to choose perinatal palliative care were significantly higher within the high mortality risk group as compared to other severity groups (p < 0.001); this group also had a significantly higher mortality (p < 0.001), with a survival rate of 26.3%. Conclusion Over the study period, in France, there was an increase in continued pregnancies, despite a diagnosis of severe fetal pathology in France. Therefore, it is essential that perinatal professionals are provided with a palliative care framework and training in their approach for this population which is heterogeneous in terms of etiology.

Similar content being viewed by others
References
Avis N° 107: Avis sur les problèmes éthiques liés aux diagnostics anténatals: le diagnostic prénatal (DPN) et le diagnostic préimplantatoire (DPI). (2009). Retrieved August 30, 2016, from http://www.ccne-ethique.fr/fr/publications/avis-sur-les-problemes-ethiques-lies-aux-diagnostics-antenatals-le-diagnostic-prenatal.
Betremieux, P. (2009). Palliative care of the newborn, how is it possible? Archives de pediatrie: organe officiel de la Societe francaise de pediatrie, 16(6), 603–605.
Betremieux, P., Huillery, M. L. (2015). Palliative care, anticipation and uncertainty in perinatal medicine. Journal of Medpal,14, 331–340.
Betremieux, P., & Mannoni, C. (2013). Neonatal palliative care and culture. Archives de pediatrie: organe officiel de la Societe francaise de pediatrie, 20(9), 1000–1005.
Carlsson, T., Bergman, G., Melander Marttala, U., Wadensten, B., & Mattsson, E. (2015). Information following a diagnosis of congenital heart defect: Experiences among parents to prenatally diagnosed children. PLoS ONE, 10(2), e0117995.
Code de la santé publique—Article R.4127-33. (2011). Retrieved August 30, 2016, from https://www.legifrance.gouv.fr/affichCodeArticle.do?cidTexte=LEGITEXT000006072665&idArticle=LEGIARTI000006687544&dateTexte=vig.
Code de la santé publique—Article L2213-1. (2011). Retrieved August 30, 2016, from https://www.legifrance.gouv.fr/affichCodeArticle.do?cidTexte=LEGITEXT000006072665&idArticle=LEGIARTI000006687544&dateTexte=vig.
De Mezerac, I. (2004). Un enfant pour l’éternité. Paris: Editions du Rocher.
Dehan, M., Gold, F., Grassin, M., Janaud, J. C., Morisot, C., Ropert, J. C., et al. (2001). Withholding and withdrawing treatment in the perinatal period: Importance of a coherent attitude between gyneco-obstetricians and paediatricians. Journal de gynécologie, obstétrique et biologie de la reproduction, 30(2), 133–138.
Dommergues, M., Mandelbrot, L., Mahieu-Caputo, D., Boudjema, N., & Durand-Zaleski, I. (2010). Termination of pregnancy following prenatal diagnosis in France: How severe are the foetal anomalies? Prenatal Diagnosis, 30(6), 531–539.
Fonseca, A., Nazare, B., & Canavarro, M. C. (2013). Clinical determinants of parents’ emotional reactions to the disclosure of a diagnosis of congenital anomaly. Journal of Obstetric, Gynecologic, and Neonatal Nursing: JOGNN/NAACOG, 42(2), 178–190.
Groupe de Reflexion sur les Aspects Ethiques de la Périnatologie, Dageville C., Rameix S., Andrini P., Betremieux P., Jarreau P. H., et al. (2007). End of life in neonatal medicine under the direction of French law. Archives de pediatrie: organe officiel de la Societe francaise de pediatrie,14(10), 1219–1230.
Guon, J., Wilfond, B. S., Farlow, B., Brazg, T., Janvier, A. (2014). Our children are not a diagnosis: The experience of parents who continue their pregnancy after a prenatal diagnosis of trisomy 13 or 18. American Journal of Medical Genetics Part A, 164A(2), 308–318.
Hubert, P., Canoui, P., Cremer, R., Leclerc, F., & Gfrup (2005). Withholding or withdrawing life saving treatment in paediatric intensive care unit: GFRUP guidelines. Archives de pediatrie: organe officiel de la Societe francaise de pediatrie, 12(10), 1501–1508.
Jaquier, M., Klein, A., & Boltshauser, E. (2006). Spontaneous pregnancy outcome after prenatal diagnosis of anencephaly. BJOG: An International Journal of Obstetrics and Gynaecology, 113(8), 951–953.
Larsson, A. K., Svalenius, E. C., Lundqvist, A., & Dykes, A. K. (2010). Parents’ experiences of an abnormal ultrasound examination—vacillating between emotional confusion and sense of reality. Reproductive Health, 7, 10.
Le Coz P. (2014). Vulnerability of the newborn, philosophical ans ethical challenges. Cahiers de la puériculture, 280, 12–16.
Loi n° 2005-370 du 22 avril 2005 relative aux droits des malades et à la fin de vie. (2005). Retrieved August 30, 2016, from https://www.legifrance.gouv.fr/affichTexte.do?cidTexte=JORFTEXT000031970253&categorieLien=id.
Loi n° 2016-87 du 2 février 2016 créant de nouveaux droits en faveur des malades et des personnes en fin de vie. (2016). Retrieved August 30, 2016, from https://www.legifrance.gouv.fr/affichTexte.do?cidTexte=JORFTEXT000031970253&categorieLien=id
Loi n° 75-17 du 17 janvier 1975 relative à l’interruption volontaire de la grossesse. (1975). Retrieved August 30, 2016, from https://www.legifrance.gouv.fr/affichTexte.do?cidTexte=JORFTEXT000000700230.
Madeuf, A., Roman, H., & Verspyck, E. (2016). Continuation of pregnancy despite a diagnosis of severe fetal anomaly: A retrospective French study. Acta obstetricia et gynecologica Scandinavica, 95(8), 934–940.
Mazille, N., Litzler-Renault, S., Weider, I., Donato, L., Astruc, D., & Kuhn, P. (2104). [Palliative care for newborns: Practices in a level-III unit during a 5-year period]. Archives de pediatrie: organe officiel de la Societe francaise de pediatrie, 21(2), 177–183.
Rapport médical et scientifique de l’assistance médicale à la procréation et de la génétique humaine en France, 2014. Agence de la biomédecine. Retrieved August 30, 2016, from http://www.agencebiomedecine.fr/annexes/bilan2014/donnees/diag-prenat/02centres/synthese.htm.
Tosello, B., Dany, L., Betremieux, P., Le Coz, P., Auquier, P., Gire, C., et al. (2015). Barriers in referring neonatal patients to perinatal palliative care: A French multicenter survey. PLoS ONE, 10(5), e0126861.
Tosello, B., Dany, L., Gire, C., Betremieux, P., Vriet-Ndour, M. E., Le Coz, P., et al. (2014). Perceptions of lethal fetal abnormality among perinatal professionals and the challenges of neonatal palliative care. Journal of Palliative Medicine, 17(8), 924–930.
Tosello, B., Haddad, G., Gire, C., & Einaudi, M. A. (2016). Lethal fetal abnormalities: How to approach perinatal palliative care? The Journal of Maternal-Fetal & Neonatal Medicine, 26, 1–4.
Tosello, B., Le Coz, P., Payot, A., Gire, C., & Einaudi, M. A. (2013). Palliative care birth plan: A field of perinatal medicine to build. Gynecologie, Obstetrique & Fertilite, 41(4), 251–254.
Wilkinson, D., de Crespigny, L., & Xafis, V. (2014). Ethical language and decision-making for prenatally diagnosed lethal malformations. Seminars in Fetal & Neonatal Medicine, 19(5), 306–311.
Wilkinson, D. J., Thiele, P., Watkins, A., & De Crespigny, L. (2012). Fatally flawed? A review and ethical analysis of lethal congenital malformations. BJOG: An International Journal of Obstetrics and Gynaecology, 119(11), 1302–1308.
Wool, C. (2011). Systematic review of the literature: Parental outcomes after diagnosis of fetal anomaly. Advances in Neonatal Care, 11(3), 182–192.
Wool C. (2013). State of the science on perinatal palliative care. Journal of Obstetric, Gynecologic, & Neonatal Nursing, 42(3), 372–382 (quiz E54-5).
Author information
Authors and Affiliations
Corresponding author
Appendix: Leonetti Law of 22 April 2005
Appendix: Leonetti Law of 22 April 2005
The main directives derived from this law are:
-
Ratification of ability to refuse extraordinary therapeutic measures (Art. 1)
-
More rigorous enforcement of provision of information to patients (Art. 2)
-
More rigorous enforcement of freedom of choice accorded to conscious patients (Art. 6)
-
The introduction of the concept of “double effect”
-
The introduction of the “collegial procedure” for patients unable to express their wishes
-
The decriminalization of limitation of treatments (Art. 122-4 of the French Criminal Code) provided procedure is adhered to
-
Ratification of palliative care (extended to community-based healthcare establishments and more rigorously enforced in healthcare institutions).
The French Law of 22 April 2005 on patient rights and end-of-life reinforces the rights of all patients and accords specific rights to end-of-life patients. The practitioner must support the patient until their final moments, ensure quality of life through appropriate care and measures, protect the patient’s dignity, and comfort their entourage. The practitioner does not have the right to deliberately cause death (Art. R.4127-38 of the French Public Health Code). As regards situations of lethal fetal abnormality, this law applies to the unborn baby. The newborn acquires the legal status of a person; they too can die and the law makes it possible for them to die supported, relieved and surrounded.
Rights and permissions
About this article
Cite this article
Bourdens, M., Tadonnet, J., Hostalery, L. et al. Severe Fetal Abnormality and Outcomes of Continued Pregnancies: A French Multicenter Retrospective Study. Matern Child Health J 21, 1901–1910 (2017). https://doi.org/10.1007/s10995-017-2305-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-017-2305-0