Abstract
Objective: The purpose of this study was to determine the false positive percentage of capillary blood lead screening in a statewide surveillance system and to explore potential predictors of false positive results.
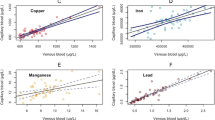
Methods: Data were all blood lead tests of 0–5 year old children in Maine during 2002–2003. We determined the proportion of children with elevated (≥10 μg/dL) capillary test results who received a venous confirmatory test, and calculated the percentage of false positive tests, defined as a capillary test of ≥10 μg/dL with a confirmatory venous test of <10 μg/dL. Multivariable binomial regression was used to determine whether capillary blood lead level and length of time between capillary and venous tests predicted false positive results, after controlling for potential confounders. We also examined the positive bias of the capillary test among both false positive and true positive results.
Results: Seventy-three percent of elevated capillary screening tests (2.2 percent of all capillary screening tests) were false positives. False positive results were less likely for capillary levels of 15–19 μg/dL (RR=0.78; 95% CI 0.5–0.92) and 20 μg/dL or above (RR=0.83; 95% CI 0.71–0.96) compared to 10–14 μg/dL. The percentage of false positives did not vary by interval between screening and confirmatory tests. The capillary test exhibited a positive bias compared to the venous test, even among true positive results.
Conclusions: False positive results may have been caused by sample contamination, rather than laboratory error or true variation in blood lead level between screening and confirmatory tests. Capillary screening could be improved by training in proper sample collection methods.


Similar content being viewed by others
References
U.S. Department of Health and Human Services. Healthy People 2010, 2nd edn. With understanding and improving health and objectives for improving health. 2 vols. Washington, DC: U.S. Government Printing Office; 2000.
Centers for Disease Control and Prevention. Preventing lead poisoning in young children: a statement by the centers for disease control. Atlanta, GA: CDC; 1991.
Schlenker TL, Fritz CJ, Mark D, et al. Screening for lead poisoning: comparability of simultaneously drawn capillary and venous blood samples. JAMA 1994;271:1346–8.
Schonfeld DJ, Cullen MR, Rainey PM, et al. Screening for lead poisoning in an urban pediatric clinic using samples obtained by fingerstick. Pediatrics 1994;94(2):174–9.
Parsons PJ, Reilly AA, Esernio-Jenssen D. Screening children exposed to lead: an assessment of the capillary blood lead fingerstick test. Clin Chem 1997;43(2):302–11.
Schonfeld DJ, Rainey PM, Cullen MR, Showalter DR, Cicchetti DV. Screening for lead poisoning by fingerstick in suburban pediatric practices. Arch Pediatr Adolesc Med 1995;149:447–50.
Sargent JD, Dalton M, Klein RZ. Diagnostic testing unwarranted for children with blood lead 10 to 14 ug/dL. Pediatrics 1999;103(4):e51.
Fischbein A. Occupational and environmental exposure to lead. In: Rom WN, editor, Environmental and occupational medicine. Philadelphia: Lippincott-Raven; 1998, pp. 977–978.
Sargent JD, Dalton MA. Rethinking the threshold for an abnormal capillary blood lead screening test. Arch Pediatr Adolesc Med 1996;150:1084–8.
Centers for Disease Control and Prevention. Update: blood lead levels—United States, 1991–1994. MMWR Morb Mortal Wkly Rep 1997;46:141–6.
Centers for Disease Control and Prevention. Blood lead levels—United States, 1999–2002. MMWR Morb Mortal Wkly Rep 2005;54:513–6.
Centers for Disease Control and Prevention. Screening young children for lead poisoning: guidance for state and local public health officials. Atlanta, GA: CDC; 1997.
Parsons PJ, Slavin E. A rapid Zeeman graphite furnace atomic absorption spectrometric method for the determination of lead in blood. Spectrochimica Acta 1993;48B:925–39.
Maine Childhood Lead Poisoning Prevention Program, Environmental Health Unit. Childhood Lead Poisoning in Maine: 2004 Surveillance Report. Augusta, Maine: Maine Department of Health and Human Services; Forthcoming 2007.
Schlenker T. Comparability of capillary and venous blood samples for lead screening [letters]. JAMA 1994;272:1482.
Agency for Toxic Substances and Disease Registry (ATSDR). Toxicological profile for lead. (Draft for Public Comment). Atlanta, GA: U.S. Department of Health and Human Services, Public Health Service; 2005.
Centers for Disease Control and Prevention. Managing elevated blood lead levels among young children: recommendations from the advisory committee on childhood lead poisoning prevention. Atlanta, GA: CDC; 2002.
US Department of Agriculture Economic Research Service. Measuring rurality: rural-urban commuting area codes. Available at http://www.ers.usda.gov/briefing/Rurality/RuralUrbanCommutingAreas/. Accessed March 7, 2006.
Kemper AR, Cohn LM, Fant KE, Dombkowski KJ, Hudson SR. Follow-up testing among children with elevated screening blood lead levels. JAMA 2005;293:2232–7.
Canfield RL, Henderson CR, Cory-Slechta DA, Cox C, Jusko TA, Lanphear BP. Intellectual impairment in children with blood lead concentrations below 10 μg per deciliter. N Engl J Med 2003;348:1517–26.
Acknowledgments
The authors gratefully acknowledge Katie Meyer, ScD, for technical and editorial assistance, Chris Paulu, ScD, for sharing his modifications to the rural/urban classification system, and Andrew Smith, SM, ScD, for guidance and assistance in data presentation. This study was supported in part by an appointment to the Applied Epidemiology Fellowship Program administered by the Council of State and Territorial Epidemiologists (CSTE) and funded by the Centers for Disease Control and Prevention (CDC) Cooperative Agreement U60/CCU007277.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Anderson, M.K., Amrich, M., Decker, K.L. et al. Using State Lead Poisoning Surveillance System Data to Assess False Positive Results of Capillary Testing. Matern Child Health J 11, 603–610 (2007). https://doi.org/10.1007/s10995-007-0196-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-007-0196-1