Abstract
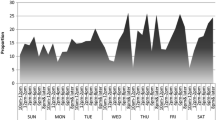
Most adolescents face numerous obstacles to good sleep, which may undermine healthy development. In this study, we used latent class analysis and identified four categories of sleep barriers in a diverse sample of 553 urban youth (57% female). The majority profile, School/Screens Barriers, reported the most homework and extracurricular barriers, along with high screen time. The Home/Screens Barriers class (i.e., high environmental noise, light, screen use) and the High/Social Barriers class (i.e., high barriers across domains, particularly social) reported the poorest sleep quality and highest depressive/anxiety symptoms. The Minimal Barriers class—predominately male, with low depressive/anxiety symptoms—reported more sleep per night. We discuss implications of our findings for targeting interventions to address poor adolescent sleep among specific clusters of students.

Similar content being viewed by others
References
Adam, E. K., Snell, E. K., & Pendry, P. (2007). Sleep timing and quantity in ecological and family context: a nationally representative time-diary study. Journal of Family Psychology, 21(1), 4–19.
Bartel, K. A., & Gradisar, M. (2017). New directions in the link between technology use and sleep in young people. In: S. Nevšímalová, O. Bruni (Eds.), Sleep Disorders in Children (pp. 69–80). Switzerland: Springer International Publishing.
Bartel, K. A., Gradisar, M., & Williamson, P. (2015). Protective and risk factors for adolescent sleep: a meta-analytic review. Sleeping Medicine Reviews, 21, 72–85.
Blake, M., Schwartz, O., Waloszek, J. M., Raniti, M., Simmons, J. G., Murray, G., & Allen, N. B. (2017). The SENSE study: Treatment mechanisms of a cognitive behavioral and mindfulness-based group sleep improvement intervention for at-risk adolescents. Sleep, 40(6), 1–11. https://doi.org/10.1093/sleep/zsx061.
Blake, M., Waloszek, J. M., Schwartz, O., Raniti, M., Simmons, J. G., Blake, L., & Dudgeon, P. (2016). The SENSE study: post intervention effects of a randomized controlled trial of a cognitive–behavioral and mindfulness-based group sleep improvement intervention among at-risk adolescents. Journal of Consulting and Clinical Psychology, 84(12), 1039–1051.
Cain, N., & Gradisar, M. (2010). Electronic media use and sleep in school-aged children and adolescents: a review. Sleeping Medicine, 11(8), 735–742.
Cappuccio, F., Taggart, F. M., Kandala, N., Currie, A., Peile, E., Stranges, S., & Miller, M. A. (2008). Meta-analysis of short sleep duration and obesity in children and adults. Sleep, 31(5), 619–626.
Carskadon, M. A. (2011). Sleep in adolescents: the perfect storm. Pediatric Clinics of North America, 58(3), 637–647. https://doi.org/10.1016/j.pcl.2011.03.003.
Cassoff, J., Knäuper, B., Michaelsen, S., & Gruber, R. (2013). School-based sleep promotion programs: effectiveness, feasibility and insights for future research. Sleeping Medicine Reviews, 17(3), 207–214.
Clinkinbeard, S. S., Simi, P., Evans, M. K., & Anderson, A. L. (2011). Sleep and delinquency: does the amount of sleep matter? Journal of Youth and adolescence, 40(7), 916–930. https://doi.org/10.1007/s10964-010-9594-6.
Collins, L. M., & Lanza, S. T. (2013). Latent class and latent transition analysis: With applications in the social, behavioral, and health sciences (Vol. 718). Hoboken, NJ: John Wiley & Sons.
Condén, E., Ekselius, L., & Åslund, C. (2013). Type D personality is associated with sleep problems in adolescents. Results from a population-based cohort study of Swedish adolescents. Journal of Psychosomatic Research, 74(4), 290–295.
Dahl, R. E., & Lewin, D. S. (2002). Pathways to adolescent health sleep regulation and behavior. Journal of Adolescent Health, 31(6), 175–184.
Danielsson, N. S., Harvey, A. G., MacDonald, S., Jansson-Fröjmark, M., & Linton, S. J. (2013). Sleep disturbance and depressive symptoms in adolescence: the role of catastrophic worry. Journal of Youth and adolescence, 42(8), 1223–1233.
de la Vega, R., Tome-Pires, C., Sole, E., Racine, M., Castarlenas, E., Jensen, M. P., & Miro, J. (2015). The Pittsburgh Sleep Quality Index: validity and factor structure in young people. Psychological Assessment, 27(4), e22–27. https://doi.org/10.1037/pas0000128.
Doane, L. D., & Thurston, E. C. (2014). Associations among sleep, daily experiences, and loneliness in adolescence: evidence of moderating and bidirectional pathways. Journal of Adolescence, 37(2), 145–154. https://doi.org/10.1016/j.adolescence.2013.11.009.
Fuligni, A. J., & Hardway, C. (2006). Daily variation in adolescents’ sleep, activities, and psychological well-being. Journal of Research on Adolescence, 16(3), 353–378.
Gaarde, J., Hoyt, L. T., Ozer, E. J., Harvey, A. G., Gorham, T. P., Deardorff, J.,… Kyauk, C. K. (2018). So much to do before I sleep: a mixed-method study of adolescent-perceived barriers and facilitators to sleep. Youth & Society. [Epub ahead of print].
Gradisar, M., Gardner, G., & Dohnt, H. (2011). Recent worldwide sleep patterns and problems during adolescence: a review and meta-analysis of age, region, and sleep. Sleeping Medicine, 12(2), 110–118.
Hale, L., & Guan, S. (2015). Screen time and sleep among school-aged children and adolescents: a systematic literature review. Sleeping Medicine Reviews, 21, 50–58.
Heissel, J. A., Sharkey, P. T., Torrats‐Espinosa, G., Grant, K., & Adam, E. K. (2017). Violence and vigilance: the acute effects of community violent crime on sleep and cortisol. Child Development. [Epub ahead of print].
Hirshkowitz, M., Whiton, K., Albert, S. M., Alessi, C., Bruni, O., DonCarlos, L., & Kheirandish-Gozal, L. (2015). National Sleep Foundation’s sleep time duration recommendations: methodology and results summary. Sleeping Health, 1(1), 40–43.
Kann, L., McManus, T., Harris, W., Shanklin, S., Flint, K., Hawkins, J., & Zaza, S. (2016). Youth risk behavior survellience—United States, 2015. Center for Disease Control and Prevention Morbidity and Mortality Weekly Report, 65(6), 1–174.
Keyes, K. M., Maslowsky, J., Hamilton, A., & Schulenberg, J. (2015). The great sleep recession: changes in sleep duration among US adolescents, 1991–2012. Pediatrics, 135(3), 460–468.
Laursen, B. P., & Hoff, E. (2006). Person-centered and variable-centered approaches to longitudinal data. Merrill-Palmer Quarterly, 52(3), 377–389.
Marco, C. A., Wolfson, A. R., Sparling, M., & Azuaje, A. (2012). Family socioeconomic status and sleep patterns of young adolescents. Behavioral Sleeping Medicine, 10(1), 70–80.
Maslowsky, J., & Ozer, E. J. (2014). Developmental trends in sleep duration in adolescence and young adulthood: evidence from a national United States sample. Journal of Adolescent Health, 54(6), 691–697. https://doi.org/10.1016/j.jadohealth.2013.10.201.
Minges, K. E., & Redeker, N. S. (2016). Delayed school start times and adolescent sleep: a systematic review of the experimental evidence. Sleeping Medicine Reviews, 28, 86–95.
Muthén, L. K., & Muthén, B. O. (1998–2015). Mplus User’s Guide. 7 ed. Los Angeles, CA: Muthén & Muthén..
National Science Foundation (2014). 2014 Sleep in America poll: sleep in the modern family. Retrieved November 1, 2017, from http://www.sleepfoundation.org/sleep-polls-data/sleep-in-americapoll/2014-sleep-in-the-modern-family
Noland, H., Price, J. H., Dake, J., & Telljohann, S. K. (2009). Adolescents’ sleep behaviors and perceptions of sleep. Journal of School Health, 79(5), 224–230.
Owens, J., Wang, G., Lewin, D., Skora, E., & Baylor, A. (2017). Association between short sleep duration and risk behavior factors in middle school students. Sleep, 40(1), Zsw004.
Park, H., Tsai, K. M., Dahl, R. E., Irwin, M. R., McCreath, H., Seeman, T. E., & Fuligni, A. J. (2016). Sleep and inflammation during adolescence. Psychosomatic Medicine, 78(6), 677–685.
Paruthi, S., Brooks, L. J., D’Ambrosio, C., Hall, W. A., Kotagal, S., Lloyd, R. M., & Quan, S. F. (2016). Recommended amount of sleep for pediatric populations: a consensus statement of the American Academy of Sleep Medicine. Journal of Clinical Sleeping Medicine, 12(6), 785.
Pasch, K. E., Latimer, L. A., Cance, J. D., Moe, S. G., & Lytle, L. A. (2012). Longitudinal bi-directional relationships between sleep and youth substance use. Journal of Youth and adolescence, 41(9), 1184–1196.
Passchier-Vermeer, W., & Passchier, W. F. (2000). Noise exposure and public health. Environmental Health Perspectives, 108(Suppl 1), 123–131.
Radloff, L. S. (1977). The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1(3), 385–401.
Reynolds, C. R., & Richmond, B. O. (1978). What I think and feel: a revised measure of children’s manifest anxiety. Journal of Abnormal Child Psychology, 6(2), 271–280.
Roberts, R., Roberts, C., & Duong, H. (2009). Sleepless in adolescence: prospective data on sleep deprivation, health and functioning. Journal of Adolescence, 32(5), 1045–1057.
Sadeh, A., Gruber, R., & Raviv, A. (2003). The effects of sleep restriction and extension on school‐age children: What a difference an hour makes. Child Development, 74(2), 444–455.
Seidman, E., Allen, L., Lawrence Aber, J., Mitchell, C., Feinman, J., Yoshikawa, H., & Ortiz-Torres, B. (1995). Development and validation of adolescent‐perceived microsystem scales: Social support, daily hassles, and involvement. American Journal of Community Psychology, 23(3), 355–388.
Singh, G. K., & Kenney, M. K. (2013). Rising prevalence and neighborhood, social, and behavioral determinants of sleep problems in US children and adolescents, 2003–2012. Sleep Disorders, Article ID 394320.
Sivertsen, B., Harvey, A. G., Pallesen, S., & Hysing, M. (2015). Mental health problems in adolescents with delayed sleep phase: results from a large population-based study in Norway. Journal of Sleeping Research, 24(1), 11–18. https://doi.org/10.1111/jsr.12254.
Tavernier, R., & Adam, E. K. (2017). Text message intervention improves objective sleep hours among adolescents: the moderating role of race-ethnicity. Sleeping Health, 3(1), 62–67.
Tavernier, R., Heissel, J. A., Sladek, M. R., Grant, K. E., & Adam, E. K. (2017). Adolescents’ technology and face-to-face time use predict objective sleep outcomes. Sleeping Health: Journal of the National Sleeping Foundation, 3(4), 276–283.
Tavernier, R., & Willoughby, T. (2014). Sleep problems: predictor or outcome of media use among emerging adults at university? Journal of Sleeping Research, 23(4), 389–396.
Van den Bulck, J. (2004). Television viewing, computer game playing, and Internet use and self-reported time to bed and time out of bed in secondary-school children. Sleep, 27(1), 101–104.
Vollmer, C., Michel, U., & Randler, C. (2012). Outdoor light at night (LAN) is correlated with eveningness in adolescents. Chronobiology International, 29(4), 502–508.
Waloszek, J. M., Schwartz, O., Simmons, J. G., Blake, M., Blake, L., Murray, G., & Dudgeon, P. (2015). The SENSE Study (Sleep and Education: learning New Skills Early): a community cognitive-behavioural therapy and mindfulness-based sleep intervention to prevent depression and improve cardiac health in adolescence. BMC Psychology, 3(39), 1–12.
Weaver, E., Gradisar, M., Dohnt, H., Lovato, N., & Douglas, P. (2010). The effect of presleep video-game playing on adolescent sleep. Journal of Clinical Sleeping Medicine, 6(2), 184–189.
Wood, A. W., Loughran, S. P., & Stough, C. (2006). Does evening exposure to mobile phone radiation affect subsequent melatonin production? International Journal of Radiation Biology, 82(2), 69–76.
Acknowledgements
We thank the study participants, the participating schools, and our research team at the University of California at Berkeley.
Authors’ Contributions
L.T.H. designed the current study, participated in data collection, analysis, and interpretation, and drafted the manuscript; J.M. participated in the design of the current study, interpretation of the analysis, and helped draft the manuscript; J.S.O. performed the statistical analysis and helped draft the manuscript; E.J.O. and A.G.H. designed and led the larger intervention study and provided critical revisions of the manuscript. J.D. participated in the study design and provided critical revisions of the manuscript. All authors read and approved the final manuscript.
Funding
This study was funded by the National Institutes of Health (NIH): National Institute on Drug Abuse (NIDA) 5 R34 DA035349-03 (co-PIs Emily J. Ozer and Allison G. Harvey). The findings and conclusions of this report are solely the responsibility of the authors and do not necessarily represent the official views of the NIH. The NIH played no role in the study design, data collection, writing, or decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures involving human participants were in accordance with the APA Ethical Standards in the treatment of the participants and approved by the Institutional Review Board at the University of California, Berkeley.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Hoyt, L.T., Maslowsky, J., Olson, J.S. et al. Adolescent Sleep Barriers: Profiles within a Diverse Sample of Urban Youth. J Youth Adolescence 47, 2169–2180 (2018). https://doi.org/10.1007/s10964-018-0829-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10964-018-0829-2