Abstract
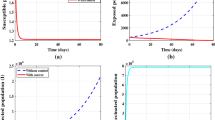
In this article, we propose a modified SVIRS model that describes the evolution of the Covid-19 on a human population during a vaccination strategy. After describing our proposed model, we study the local and the global stability analysis of the model using Routh-Hurwitz criteria and by constructing the Lyapunov functions. In order to formulate an optimal control problem, we study the sensitivity analysis of the model parameters to determine the model robustness to parameter values, that is, to help us know the parameters that have a high impact on the reproduction number \(\mathscr {R}_{0}\) and to propose some appropriate control. The existence of the optimal control is investigated, and a characterization of the optimal control is given using the Pontryagin’s maximum principle. By this, we propose three control strategies that help the public health officials to implement programs to achieve collective immunity and thus come closer to reduce the spread of the SARS-CoV-2 virus. These strategies are as follows: awareness and prevention, administrative measures and awareness campaigns about the importance of vaccination and also the prevention measures, and finally, strengthening internal measures by controlling the proportion of immigrants coming to the country. In the end, some numerical simulations are performed to illustrate the theoretical results.







Similar content being viewed by others
Data availability
The data used to support the findings of this study are available from the corresponding author upon request.
Notes
References
Hui, D.S., Azhar, E.I., Madani, T.A., Ntoumi, F., Kock, R., Dar, O., Ippolito, G., Mchugh, T.D., Memish, Z.A., Drosten, C., Zumla, A., Petersen, E.: The continuing 2019-ncov epidemic threat of novel coronaviruses to global health - the latest 2019 novel coronavirus outbreak in wuhan, china. International journal of infectious diseases : IJID : official publication of the International Society for Infectious Diseases 91, 264–266 (2020)
Wang, L., Zhou, Y., He, J., Zhu, B., Wang, F., Tang, L., Kleinsasser, M., Barker, D., Eisenberg, M.C., Song, P.X.: An epidemiological forecast model and software assessing interventions on the covid-19 epidemic in china. Journal of Data Science 18(3), 409–432 (2020)
Grifoni, A., Weiskopf, D., Ramirez, S.I., Mateus, J., Dan, J.M., Moderbacher, C.R., Rawlings, S.A., Sutherland, A., Premkumar, L., Jadi, R.S., et al.: Targets of t cell responses to sars-cov-2 coronavirus in humans with covid-19 disease and unexposed individuals. Cell 181(7), 1489–1501 (2020)
WHO: Report of the who-china joint mission on coronavirus disease 2019 (covid-19). Encyclopedia Britannica. (2022)
Rogers, K.: Covid-19 vaccine. World Health Organization (2020)
Seto, W., Tsang, D., Yung, R., Ching, T., Ng, T., Ho, M., Ho, L., Peiris, J.: Effectiveness of precautions against droplets and contact in prevention of nosocomial transmission of severe acute respiratory syndrome (sars). The lancet 361(9368), 1519–1520 (2003)
Al-Jasser, F.S., Nouh, R.M., Youssef, R.M.: Epidemiology and predictors of survival of mers-cov infections in riyadh region, 2014–2015. Journal of infection and public health 12(2), 171–177 (2019)
Thompson, W.W., Weintraub, E., Dhankhar, P., Cheng, P.-Y., Brammer, L., Meltzer, M.I., Bresee, J.S., Shay, D.K.: Estimates of us influenza-associated deaths made using four different methods. Influenza and other respiratory viruses 3(1), 37–49 (2009)
Organization, W.H., et al.: Are the ebola outbreaks in nigeria and senegal over. http://www.who.int/mediacentre/news/ebola/14-october-2014/en (2014)
Walensky, R.P., Del Rio, C.: From mitigation to containment of the covid-19 pandemic: putting the sars-cov-2 genie back in the bottle. Jama 323(19), 1889–1890 (2020)
Walker, P.G., Whittaker, C., Watson, O.J., Baguelin, M., Winskill, P., Hamlet, A., Djafaara, B.A., Cucunubá, Z., Olivera Mesa, D., Green, W., et al.: The impact of covid-19 and strategies for mitigation and suppression in low-and middle-income countries. Science 369(6502), 413–422 (2020)
Rabady, S.: No one is safe unless everyone is safe. Zeitschrift für Allgemeinmedizin 97(10), 385–385 (2021)
Rogers, K.: World health organization: Advice for public. WHO Int (2020)
Wang, X., Washington, D., Weber, G.F.: Complex systems analysis informs on the spread of covid-19. Epidemiologic Methods 10(s1), 20210019 (2021)
Anderson, R.M., May, R.M.: Infectious diseases of humans: dynamics and control. Oxford university press (1991)
Lin, Q., Zhao, S., Musa, S., Gao, D., Lou, Y., Yang, S., Musa, S., Wang, M., Cai, Y., Wang, W., et al.: A conceptual model of the outbreak of novel coronavirus (2019-ncov) in wuhan, china, with human reaction and holiday effects. Int. J. Infect. Dis. 93, 211–216 (2020)
Peng, L., Yang, W., Zhang, D., Zhuge, C., Hong, L.: Epidemic analysis of covid-19 in china by dynamical modeling. arXiv preprint arXiv:2002.06563 (2020)
López, L., Rodo, X.: A modified seir model to predict the covid-19 outbreak in spain and italy: simulating control scenarios and multi-scale epidemics. Results in Physics 21, 103746 (2021)
Zuo, C., Zhu, F., Ling, Y.: Analyzing covid-19 vaccination behavior using an seirm/v epidemic model with awareness decay. Frontiers in Public Health 10, 817749 (2022)
Li, Y., Ge, L., Zhou, Y., Cao, X., Zheng, J.: Toward the impact of non-pharmaceutical interventions and vaccination on the covid-19 pandemic with time-dependent seir model. Frontiers in Artificial Intelligence 4, 648579 (2021)
Yang, C., Yang, Y., Li, Y.: Assessing vaccination priorities for different ages and age-specific vaccination strategies of covid-19 using an seir modelling approach. Plos one 16(12), 0261236 (2021)
Kar, T.K., Batabyal, A.: Stability analysis and optimal control of an sir epidemic model with vaccination. Biosystems 104(2-3), 127–135 (2011)
Bakare, E.A., Nwagwo, A., Danso-Addo, E.: Optimal control analysis of an sir epidemic model with constant recruitment. International Journal of Applied Mathematics Research 3(3), 273 (2014)
Laarabi, H., Abta, A., Hattaf, K.: Optimal controliwliw of a delayed sirs epidemic model with vaccination and treatment. Acta biotheoretica 63(2), 87–97 (2015)
Samsuzzoha, M., Singh, M., Lucy, D.: Uncertainty and sensitivity analysis of the basic reproduction number of a vaccinated epidemic model of influenza. Applied Mathematical Modelling 37(3), 903–915 (2013)
Rodrigues, H.S., Monteiro, M.T.T., Torres, D.F.: Sensitivity analysis in a dengue epidemiological model. In: Conference Papers in Mathematics, vol. 2013, pp. 1–7 (2013). Hindawi Limited
Mahata, A., Paul, S., Mukherjee, S., Das, M., Roy, B.: Dynamics of caputo fractional order seirv epidemic model with optimal control and stability analysis. International Journal of Applied and Computational Mathematics 8(1), 28 (2022)
Kriss, J.L., Reynolds, L.E., Wang, A., Stokley, S., Cole, M.M., Harris, L.Q., Shaw, L.K., Black, C.L., Singleton, J.A., Fitter, D.L., et al.: Covid-19 vaccine second-dose completion and interval between first and second doses among vaccinated personsunited states, december 14, 2020- february 14, 2021. Morbidity and Mortality Weekly Report 70(11), 389 (2021)
Roser, M., Ritchie, H., Ortiz-Ospina, E., Hasell, J.: Coronavirus disease (covid-19)–statistics and research. Our World in data 4, 1–45 (2020)
Van den Driessche, P., Watmough, J.: Reproduction numbers and sub-threshold endemic equilibria for compartmental models of disease transmission. Mathematical biosciences 180(1-2), 29–48 (2002)
Ye, H., Gao, J., Ding, Y.: A generalized gronwall inequality and its application to a fractional differential equation. Journal of Mathematical Analysis and Applications 328(2), 1075–1081 (2007). https://doi.org/10.1016/j.jmaa.2006.05.061
Roskilly, T., Mikalsen, R.: Closed-loop stability. Marine Systems Identification, Modelling and Control, 97–122 (2015)
Makinde, O.D., Okosun, K.O.: Impact of chemo-therapy on optimal control of malaria disease with infected immigrants. BioSystems 104(1), 32–41 (2011)
Chitnis, N., Cushing, J.M., Hyman, J.: Bifurcation analysis of a mathematical model for malaria transmission. SIAM Journal on Applied Mathematics 67(1), 24–45 (2006)
Bather, J.: Deterministic and stochastic optimal control. Wiley Online Library (1976)
Lukes, D.L.: Differential equations: classical to controlled (1982)
Pontryagin, L.S.: Mathematical theory of optimal processes. CRC press (1987)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lalaoui Ben Cherif, S.M., Balatif, O. & Kebiri, O. ANALYSIS AND OPTIMAL CONTROL OF A VACCINATED PANDEMIC COVID-19 MODEL. J Math Sci (2024). https://doi.org/10.1007/s10958-024-06992-7
Accepted:
Published:
DOI: https://doi.org/10.1007/s10958-024-06992-7