Abstract
Despite long being the target of racism, Asians and Asian Americans remain an understudied group regarding the mental health implications of racism. Even less is known about how Asians and Asian Americans may use religion to cope with racism and the resulting mental health implications. In this study, 330 Asian and Asian American adults from various regions of the USA were surveyed. The study results suggest that negative religious coping was associated with worsening depression, anxiety, and stress, particularly among Asian Indians, Asian Hindus, and Asian Muslims. In addition, negative religious coping may have exacerbated the deleterious effects of racism on mental health. Surprisingly, positive religious coping failed to provide any protection against racism-related mental health problems during the COVID-19 pandemic.
Similar content being viewed by others
Introduction
On March 16, 2021, six Asian women were senselessly murdered in a series of shooting rampages in the metropolitan area of Atlanta. Although the perpetrator, Robert Aaron Long, was not charged with racially motivated hate crimes, many commentators and the public have associated this tragedy with a growing wave of anti-Asian hate crimes in the USA during the COVID-19 pandemic (McLaughlin et al., 2021). According to a June 2020 Pew Research study, 58% of Asian Americans perceived an increase in racist views against them since the pandemic began (Pew Research Center, 2020). Overall, as of the Atlanta shootings, nearly 3,800 anti-Asian racist incidents had been reported across the USA since early 2020—a 32% increase from a year before (Stop AAPI Hate, 2021).
In response to the Atlanta mass shootings and numerous other anti-Asian hate crimes, mass protests have occurred across the USA and around the world calling for #StopAsianHate. What has remained less visible and rarely discussed, however, is how this wave of anti-Asian racism may affect the mental health of Asians and Asian Americans. Specifically, how do Asians and Asian Americans use their personal religious beliefs and practices to cope with mental distress from racism? What kinds of religious coping relieve mental distress from racism, and what kinds of religious coping can backfire? Inspired by the Minority Stress Theory (Meyer, 2003), this study surveyed 330 Asian and Asian American adults living in the USA to better understand the mental health consequences of anti-Asian racism during the COVID-19 pandemic. More importantly, this study examines how different kinds of religious coping strategies might alleviate or perhaps exacerbate minority stress for Asians and Asian Americans.
Literature Review
Prior research has revealed a complex, dynamic relationship between religion and mental health. Some aspects of religiosity may protect one’s mental health by providing social support, a sense of assurance and comfort, or a stronger bond with a higher power. These forms of religiosity may include but are not limited to frequent religious service attendance (e.g., Bradshaw & Ellison, 2010), religious salience (e.g., prayer) (e.g., Ellison et al.,2009a; b), and a belief in an afterlife (e.g., Ellison & Burdette, 2012). Particularly, research has shown that when one encounters hardships, positive religious coping, such as seeking spiritual support and benevolent religious reappraisals, may significantly improve one’s health outcomes (Pargament et al., 2004).
In contrast, a growing body of the literature has revealed the “dark side” of religion for mental health. Studies have shown that certain elements of religiosity may introduce doubting one’s faith, interpersonal conflicts with fellow believers, and a negative relationship with a higher power, which may harm one’s mental health outcomes (e.g., Ellison et al., 2010; Exline, 2002; Pargament, 2002). This is especially the case when people are confronted with traumatic experiences and use the “dark side” of religion for coping. For example, Pargament and colleagues found that when a sample of elderly, hospitalized subjects adopted negative religious coping strategies, such as punishing God reappraisal and interpersonal religious discontent, their health significantly worsened (Pargament et al., 2004).
When one is confronted with traumatic experiences such as racism, how would religion affect one’s mental health? Specifically, in the context of the COVID-19 pandemic and the resulting waves of Asian hate, would the different kinds of religious coping discussed above protect or harm the mental health of Asians and Asian Americans? By addressing these questions, this study distinguishes itself from prior studies and contributes to the subfield in several ways. First, there is a lack of studies on racism, religious coping, and mental health with a focus on Asian Americans. Only two empirical studies so far have examined how racism affects the mental health of Asian Americans through religious coping (Kim, 2017; Kim et al., 2015).
However, Asian Americans have very distinct religious and cultural characteristics compared to other racial and ethnic groups in the USA, which might lead to unique religious coping strategies in response to racism as well as unexpected mental health outcomes. According to a Pew study, compared to the general public, a higher percentage of Asian Americans are affiliated with non-Christian religions, such as Buddhism (14% vs. 1%) and Hinduism (10% vs. 0.5%) (Pew Research Center, 2012). This higher prevalence of non-Judeo-Christian religions within the Asian American population might challenge some of the previous research on religious coping and mental health, which is based on samples of Christian Asian American college students (Kim, 2017; Kim et al., 2015) and thus ignores the diverse religious and demographic profiles of the Asian American population.
Second, even for Christian Asian Americans, who account for the largest share (42%) of the Asian American population, unique Asian cultural values emphasizing collectivism, emotional restraint, dependence on relationships, and respect for hierarchy may lead to differences in religious coping styles compared to their counterparts from other racial and ethnic groups (Kim, 2017; Pew Research Center, 2012). For example, Bjorck et al. (2001) found that compared to European Americans, Asian Americans scored higher on religious coping strategies emphasizing collectivism, self-restraints, and other Asian cultural values. Kim (2017) speculated that the unique religious coping strategies in the Asian cultural context might be responsible for unexpected mental health outcomes for Asian Americans. For example, religious coping strategies emphasizing forgiveness only exacerbated mental distress from racism for a sample of 169 Christian Asian American college students (Kim, 2017).
In another study based on 107 Christian Asian American college students, Kim and colleagues (2015) found that negative religious coping strategies protected the subjects from racism-related mental health hazards. The authors argued that negative religious coping may trigger Asians, whose culture values social relationships, to seek social support, which in turn improved mental health (Kim et al., 2015). What would be some other “counterintuitive” religious coping effects on the minority stress of Asians and Asian Americans, and how might unique Asian cultural values and beliefs explain those unexpected religious coping outcomes? With a special focus on Asians and Asian Americans, this study contributes to knowledge of this understudied population.
Finally, the COVID-19 pandemic has created a unique social and historical context for the study of racism, religious coping, and mental health among Asian Americans. The minority stress theory argues that adverse health outcomes among minorities, including Asian Americans, can be traced back to social stressors, which include distal stressors, such as blatant discrimination, as well as proximal stressors, such as vigilance and anxiety about prejudice (Cheng et al., 2015; Meyer, 2003). During the pandemic, the sharp rise in anti-Asian racism, along with health concerns about COVID-19, may pose added social stressors to the already vulnerable Asian and Asian American population. In addition, as a result of the pandemic, many religious gatherings have been cancelled or converted to virtual meetings. As discussed above, Asian culture values collectivism and dependence on social relationships. What would be the impacts of this reduced religious social support on Asian Americans’ religious coping with racism and minority stress? This study contributes to research on Asian American religious coping and the minority stress theory by capturing this unique period effect—the COVID-19 pandemic.
Methods
Data
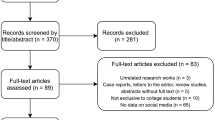
Data were collected via an online survey on Qualtrics between January 4, 2022 and January 13, 2022. Survey participants came from Qualtrics panel sample, who were recruited by Qualtrics via various channels, such as social media, customer loyalty web portals, targeted email lists, gaming sites, and member referrals. Panel members received an email from Qualtrics that included a hyperlink to the survey. They were also informed that upon completing the survey, Qualtrics would compensate them the amount they agreed upon before entering into the survey. To participate, panel members must have self-identified as Asian, been 18 or older, and lived in the USA at the time of survey.
Based on those screening criteria and the project budget, 330 complete survey responses were collected. The sample was 56.97% female and 43.03% male with a median age of 36, which is close to that of the general Asian American population: 34 (Pew Research Center, 2021a; b). The ethnicities with the highest representation in the sample were Asian Indians (23.03%), followed by Chinese (21.82%) and Pilipino (18.18%), which is somewhat in line with the demographics within the general Asian American population where Chinese account for 24%, Indians 21%, and Pilipino 19% (Pew Research Center, 2021a; b). By location, the 330 survey participants came from all regions of the USA with the Pacific (WA, OR, CA, AL, HI) being the most reported region of residence, accounting for 29.09% of the respondents. Finally, regarding country of birth and English proficiency, 50.3% of the respondents were born outside the USA, and 73.03% of the respondents could speak English very well. By comparison, among the general Asian American adult population, 71% were born in another country, and 72% could speak English proficiently ().
Measurements
The minority stress theory suggests that minority groups are more likely to suffer adverse health outcomes including worsened mental health (Meyer, 2003). To measure the dependent variable mental health, this study used the Depression, Anxiety and Stress Scale—21 Items (DASS-21). The DASS-21 includes three subscales with seven items for depression, anxiety, and stress, respectively. Depression was assessed by asking respondents to self-rate the frequency of experiencing dysphoria, hopelessness, devaluation of life, self-deprecation, lack of interest or involvement, anhedonia, and inertia since the beginning of the COVID-19 pandemic in the USA (January 2020). The response categories are 0 = did not apply to me at all, 1 = applied to me to some degree or some of the time, 2 = applied to me to a considerable degree or a good part of time, and 3 = applied to me very much or most of the time.
The same kind of response categories were used when assessing anxiety and stress. For anxiety, respondents were asked to self-rate the frequency of experiencing autonomic arousal, skeletal muscle effects, situational anxiety, and subjective experience of anxious affect since the start of the pandemic. The stress scale assesses difficulty relaxing, nervous arousal, and being easily upset, agitated, irritable, over-reactive, and impatient. Scores were summed for each of the three subscales to evaluate the extent of subjects’ mental health problems (Lovibond & Lovibond, 1995). The scale reliability coefficient is .94 for depression, .91 for anxiety, and .91 for stress.
There were two main independent variables in this study, racism and religious coping. The Subtle and Blatant Racism Scale (Yoo et al., 2010) was employed to measure racism. This scale is especially designed to assess racism against the Asian American population. There are four items for subtle racism which include—feeling viewed with suspicion because I’m Asian, overlooked because I’m Asian, faced with barriers in society because I’m Asian, and treated differently because I’m Asian. These items echo with one of the main tenets of the minority stress theory, which argues that minority status may result in increased exposure to proximal stressors such as vigilance and anxiety about prejudice (Meyer, 2003).
For blatant racism, the four items are—I am called names such as “chink, gook, etc.” because I’m Asian, I am made fun of because I’m Asian, I am told “you speak English so well” because I’m Asian, and I have been physically assaulted because I’m Asian. In this study, the survey respondents were asked to rate how often they have experienced those above situations since the beginning of the COVID-19 pandemic in the USA (January 2020). These items are in line with another main tenet of the minority stress theory—minority status may lead to increased exposure to distal stressors including experiences with rejection, prejudice, and discrimination (Meyers, 2003). For both subscales, the response categories are 0 = never, 1 = seldom, 2 = sometimes, 3 = often, and 4 = almost always for both subscales. Scores were summed for each subscale to measure the degree of racism. The scale reliability coefficient is .91 for subtle racism and .80 for blatant racism.
To measure religious coping, the brief RCOPE scale was adopted, which is a shortened version of the original 105-item RCOPE (Pargament et al., 1990, 2011). The brief RCOPE has seven items for positive religious coping including looked for a stronger connection with God, sought God’s love and care, sought help from God in letting go of my anger, tried to put my plans into action together with God, tried to see how God might be trying to strengthen me in this situation, asked forgiveness for my sins, and focused on religion to stop worrying about my problems.
In addition, the RCOPE has seven items for negative religious coping including wondered whether God had abandoned me, felt punished by God for my lack of devotion, wondered what I did for God to punish me, questioned God’s love for me, wondered whether my religious group had abandoned me, decided the devil made this happen, and questioned the power of God. Survey respondents in this study were asked to assess how often they have used those religious coping strategies since the beginning of the pandemic (January 2020). The response categories are 0 = not at all, 1 = little, 2 = somewhat, and 3 = a great deal. Scores were summed for each scale. The scale reliability coefficient is .97 for positive religious coping and .93 for negative religious coping.
In addition to religious coping, this study also controlled for other aspects of religiosity. Survey respondents were asked to report their frequency of religious service attendance (0 = never to 6 = more than once a week), frequency of reading religious scriptures in private (0 = never to 6 = many times a day), frequency of praying in private (0 = never to 6 = many times a day), importance of religion in life (0 = not important at all to 4 = extremely important), and beliefs in the existence of god (0 = definitely not to 4 = definitely yes). Responses to those variables were z-scored to create a scale measuring the mean religiosity of the respondent. The scale reliability coefficient is .90.
Regarding religious identity, this study originally followed the advice of Corcoran et al. (2021) on Asian religiosity by using more specified categories for the non-Judeo-Christian faiths as well as allowing respondents to choose multiple religious identities. This resulted in a religious identity measure with 28 response categories. However, due to the small sample size (N = 330), several response categories had fewer than 10 responses. To facilitate data analyses, this study collapsed all responses on Catholic and Protestant denominations to 1 = Christianity (n = 124, 37.58%). The other categories were 2 = Buddhism (n = 25, 7.58%), 3 = Hinduism (n = 40, 12.12%), 4 = Islam (n = 22, 6.67%), 5 = other religions (n = 15, 4.55%), 6 = more than one religion (n = 31, 9.39%), and 7 = none including agnostics, atheists, spiritual but not religious, and not religious (n = 73, 22.12%).
This study also controlled for a variety of demographic variables, such as sex (1 = male, 2 = female), marital status (1 = married, 0 = otherwise), age, number of children, education (0 = less than high school to 4 = graduate), employment status (1 = working full time, 0 = otherwise), family income (0 = less than $1000 to 25 = $150,000 or more), length of residence in current address, and residential environment (1 = rural area, 2 = small city/town, 3 = suburb near a mid-sized city, 4 = suburb near a large city, 5 = mid-sized city, and 6 = large city). Asian ethnicity was originally assessed using the US Census 2020 categorization method. However, due to the small sample size, many categories had fewer than 10 responses. Therefore, this study kept the three largest Asian ethnicities in the sample with 1 = Asian Indian (n = 76, 23.03%), 2 = Chinese (n = 72, 21.82%), and 3 = Pilipino (n = 60, 18.18%), while collapsing all other Asian ethnicities into 4 = other (n = 122, 36.97%).
Plan of Analysis
Data analyses were conducted in STATA 15. Due to the characteristics of the dependent variables, ordinary least square (OLS) regression was used for multivariate analyses. Main model assumptions were examined. Robust standard errors were used to cope with heteroscedasticity. There was no missing value in the sample provided by Qualtrics panel. Thus, there was no need for multiple imputation.
Results
Table 1 displays the descriptive statistics of variables used in this study. Following advice from prior research (Lovibond & Lovibond, 1995), the original mean of each mental health subscale was multiplied by two and compared to the cutoffs between mental health statuses: normal, mild, moderate, severe, or extremely severe for a given mental illness condition. The results suggest that on average, the sample respondents had mild depression, as their mean score of 12.84 fell within the range for that category (10–13). The sample respondents’ average score of 11 on the anxiety subscale fell within the category of moderate anxiety (10–14), and their mean score of 13.88 on the stress subscale was within the normal but borderline mild stress range, with the cutoff between normal and mild stress being 14. These mental health outcomes of the sample may indicate the grave mental health challenges confronting the Asian and Asian American community during the COVID-19 pandemic.
Other research shows that compared to 2019, there was a significant increase in Asian Americans screening for depression and anxiety in 2020—the only major racial group that saw an increase in that year (Mental Health America, 2022). Consistent with prior research on Asian Americans, subtle racism (mean = 6.57) was more often experienced than blatant racism (mean = 4.71) (Yoo et al., 2010), and positive religious coping was more often utilized than negative religious coping (Kim, 2017). In addition to the basic descriptive statistics in Table 1, results of bivariate associations among some main variables—negative religious coping, subtle racism, ethnicity, and religious tradition—were included in the appendix section for the readers’ reference (see Appendix 1). These variables, as the following regression analyses would suggest, demonstrated statistical robustness and were integral to the key findings of this study.
Table 2 presents the ordinary least square regression results for the three dependent variables: depression, anxiety, and stress. Model 1 only regresses each dependent variable on the key independent variables—subtle and blatant racism. Model 2 includes all other variables but the two religious coping scales. Model 3 is the complete model. From Model 1, one can see that both forms of racism were associated with the outcome variables: more frequent experience with racism was related to more depression, anxiety, and stress. Subtle racism had a stronger relationship than blatant racism for depression and stress, while the opposite was true for anxiety. In Model 2, all other variables except religious coping measures are included. Both forms of racism remained associated with the three mental health outcomes in Model 2 although blatant racism now had stronger relationships with mental health outcomes than did subtle racism.
Model 3 includes positive religious coping and negative religious coping scales along with all other control variables. To save space, complete results for the full models are shown in Appendix 2. The inclusion of these religious coping scales rendered blatant racism insignificant to mental health outcomes. In addition, the coefficients of blatant racism were significantly reduced for all three mental health outcomes. In contrast, the coefficients of subtle racism remained relatively stable for all three mental health measures after the inclusion of the religious coping scales. These results suggest that while religious coping may mediate the relationship between blatant racism and mental health, it had a very limited impact on the relationship between subtle racism and mental health. Overall, religious coping, specifically positive religious coping, failed to provide any protection against depression, anxiety, and stress.
Negative religious coping, conversely, had a much larger coefficient than positive religious coping and was associated with all three mental health outcomes. These results suggest that greater usage of negative religious coping was tied to higher levels of depression, anxiety, and stress. It is also important to note that negative religious coping was the only religious measure that was consistently predictive of all three mental health outcomes. In contrast, neither religious affiliation nor positive religious coping protected the subjects from mental health problems. As for the religiosity scale, it was only associated with lower depression (see Appendix 2). Therefore, religion provided little protection against mental health problems for this sample of Asians and Asian Americans. Rather, some aspect of religiosity, in this case negative religious coping, may have significantly harmed the subjects’ mental well-being.
A Wald test was performed to test model fit. For each dependent variable, the Wald test showed that the inclusion of the religious coping scales in Model 3 created a statistically significant improvement in model fit: F = 33.62 and p < .001 for depression, F = 27.46 and p < .001 for anxiety, and F = 24.27 and p < .001 for stress.
In Table 3, interaction terms between religious coping and racism are included. Each of the three dependent variable has four models. Model 1 and Model 2 contain the interaction terms between positive religious coping and blatant and subtle racism, respectively. Model 3 and Model 4 cover the interactions between negative religious coping and the two forms of racism, respectively. All control variables are included in each model. To save space, the results of control variables are not shown in Table 3.
The OLS regression results suggest that positive religious coping provided no protection against the deleterious effects of racism on mental health. None of the interaction terms involving positive religious coping were statistically significant. In contrast, negative religious coping consistently exacerbated the harmful relationship between racism and mental health. From Models 3 and 4 for each mental health outcome, one can see that all interaction terms involving negative religious coping achieved statistical significance even after controlling for multiple variables. Overall, rather than being protective, religion seemed to only backfire on the mental well-being of Asians and Asian Americans in the face of racism during the COVID-19 pandemic.
From Tables 2 and 3, one may conclude that compared to other religious measures, negative religious coping had a consistently significant relationship with mental health. Does negative religious coping work differently for different demographic groups with respect to mental health outcomes? Data exploration shows that ethnicity and religious tradition matter.
Table 4 presents interaction terms between negative religious coping and ethnicity and religious tradition on mental health. For all three mental health outcomes, interaction terms between ethnicity and negative religious coping was statistically significant—Chinese, Pilipino, and other Asians exhibited a significantly different relationship between negative religious coping and mental health than did Asian Indians. Regarding religious tradition, statistically significant variations were found for the relationship between negative religious coping and mental health when using Asian Christians as the reference group.
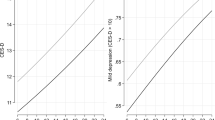
To better understand the ethnic and religious tradition variations in the negative religious coping effects on mental health, marginal plots were constructed. Figure 1 visualizes the interactive effect of Asian ethnicities and negative religious coping on depression. The graph suggests that when negative religious coping increased, all ethnicities may have experienced an increase in depression. However, this relationship was the strongest for Asian Indians relative to other ethnicities. This pattern held for the other two mental health outcomes as evidenced in Figs. 2 and 3. Speculations about these interesting ethnic variations can be found in the discussion section below.
Figures 4 and 5 show that while greater usage of negative religious coping was tied to higher levels of depression and anxiety for all religious groups, as compared to Asian Christians, the relationship was stronger for Asian Hindus and Muslims. Regarding stress (Fig. 6), as compared to Asian Christians, Asian Hindus and Muslims experienced more deleterious influences from negative religious coping, while it was the opposite to Asian Buddhists.
Discussion
In this study, 330 Asians and Asian Americans from various US regions, religions, ages, and ethnicities were surveyed for their racism experience, mental health conditions, and religiosity during the COVID-19 pandemic. The results suggest that contrary to prior research (e.g., Kim et al., 2015), religion provided very little protection against racism-induced mental health issues for this sample of Asians and Asian Americans. Instead, a certain aspect of religiosity, negative religious coping, led to worsening mental health in the face of racism.
In addition, negative religious coping also emerged as the sole consistently robust religious predictor of mental health outcomes. The lack of statistical significance of the other religious measures might be due to the pandemic as well as unique Asian cultural values. Prior research suggests that Asian culture places a high interest in collectivism and social relationships, which is also reflected in their religious life (Bjorck et al., 2001). Within such a cultural context, the pandemic and resulting social isolation measures might have significantly reduced the mental health benefits that one might have otherwise received from religious services attendance. This may especially be the case when one is confronted with traumatic experiences, such as racism, and needs social support for coping. Conversely, the unique Asian cultural value of emotional restraint, along with the reduced social interaction during the pandemic, may have exacerbated the deleterious effects of negative religious coping on mental health. However, given that in this study there was no direct measure on Asian cultural traits, such as collectivism, future research with relevant measures may want to examine the above speculations.
Another interesting finding worth noting is the existence of ethnic and religious group variations in negative religious coping effects on mental health. Asian Indians, as compared to other ethnicities, tended to experience more harmful impacts of negative religious coping on mental health outcomes. Concerning variations by religious tradition, when compared to Asian Christians, Asian Hindus and Muslims tended to experience more deleterious effects of negative religious coping on mental health.
What may explain the Asian Indian exception? When looking into the religious profile of Asian Indians in the sample, 72.37% of them were affiliated with Hinduism or Islam—the two religious groups that experienced more mental health hazards from negative religious coping. In contrast, in the sample, Hinduism and Islam collectively accounted for 0% of Chinese, 1.67% of Pilipino, and 4.92% of other Asian ethnic groups. Therefore, the high population share of Hindus and Muslims among Asian Indians may explain why the relationship between negative religious coping and mental health was stronger for Asian Indians than any other Asian ethnic groups.
What may explain the Hindu and Muslim exceptions mentioned above? It may be possible that some unique, unmeasured religious beliefs in Hinduism or Islam could affect the negative religious coping effect on mental health. To determine what specific Hindu or Islamic beliefs may be responsible, future research may want to include more diverse measures on religious beliefs as well as overcome some of this study’s limitations discussed below.
Besides the religiously affiliated Asians and Asian Americans, Asian and Asian American nones also stand out. Despite claiming no religious affiliation, many Asian and Asian American nones still scored above “0 = never” for the positive and negative religious coping scales. Otherwise, the line representing Asian and Asian American nones could not be created in Figs. 4, 5 and 6. Particularly, in Figs. 4, 5 and 6, the negative religious coping effects on mental health outcomes were almost identical between Asian and Asian American nones and their religious peers. These phenomena may lend support to previous research which suggests that Asian Americans, particularly Chinese Americans, may not conform to the Western and Protestant definition of religion. As a result, they may identify with no religion even though they may still respond to religious measures (Jeung et al., 2019). Therefore, more research is needed to understand how non-Christians interpret and understand the attitudinal statements in religious measures, such as the positive and negative religious coping scales.
Limitations of the Study
Despites its merits, this study is not without limitations. First, should funding and other resources permit, a larger, more nationally representative sample would be more convincing when generalizing key findings to the broader population. For example, the Asian Indian exception discussed above may be due to influences from non-Christian religions, particularly Hinduism and Islam. However, non-Christian religions include many different kinds of religions, such as Buddhism and folk religions, which are sometimes dominant in other ethnic groups that are not South Asian. Will the dominance of Buddhism or some other non-Christian religions also explain the negative religious coping effects on mental health for Asians who are not Indians? A larger Asian sample containing more respondents from various Asian ethnicities may be needed to better answer this question. Within the scope of available funding and conditions set by Qualtrics, this study has already achieved the largest possible sample size. However, this study employed a relatively larger and more diverse sample than other studies on racism, religion, and mental health among Asian Americans.
Second, more qualitative research may be needed to better understand some of the findings of this study. For example, from Figs. 4, 5 and 6, we may see that negative religious coping had more deleterious mental health effects for Asian Hindus and Muslims. In contrast, Asian Buddhists experienced very minimal effects from negative religious coping on their mental health. Are there any unique religious beliefs and practices among Asian Americans following these religions that may explain these variations? In-depth interviews might be used to further investigate the socio-religious mechanisms leading to particular religious coping styles and mental health outcomes across different religious backgrounds.
Third, compared to nationally representative samples, the sample in this study has a higher proportion of non-Protestant respondents. Therefore, readers may want to exercise caution when interpreting findings on religiosity, which was measured by measures from national surveys using predominantly Protestant samples (Bender et al., 2013; Iwamura et al., 2014). Finally, does negative religious coping cause mental health problems, or is it possible that those who are mentally ill are more likely to use negative religious coping? Should funding permit, longitudinal data should be collected to examine the causal direction of the negative religious coping-mental health association found in this study.
To the best of the author’s knowledge, this study is one of the few that has specifically examined the Asians’ and Asian Americans’ experience of racism, religion, and mental health during the COVID-19 pandemic. The study results suggest that contrary to conventional wisdom, religion fails to provide sufficient mental health protection to Asians and Asian Americans when coping with racism during the pandemic. Instead, the dark side of religion exists and significantly harms mental health when one is traumatized by blatant or subtle racism.
This study contributes to a growing subfield on the dark side of religion and mental health (e.g., Ellison & Lee, 2010; Nie & Olson, 2016) as they relate to a pressing social issue: Asian hate. In addition, this study provides empirical support for the famed minority stress theory with a focus on religious coping in an understudied population. Empirically, the study results may provide important implications for Asian religious leaders when helping their community members combat racism and related mental health issues during this challenging time.
Data Availability
The data presented in this study are available on request from the corresponding author.
References
Bender, C., Cadge, W., Levitt, P., & Smilde, D. (Eds.). (2013). Religion on the edge: De-centering and re-centering the sociology of religion. Oxford University Press.
Bjorck, J. P., Cuthbertson, W., Thurman, J. W., & Lee, Y. S. (2001). Ethnicity, coping, and distress among Korean Americans, Filipino Americans, and Caucasian Americans. The Journal of Social Psychology, 141, 421–442. https://doi.org/10.1080/00224540109600563
Bradshaw, M., & Ellison, C. G. (2010). Financial hardship and psychological distress: Exploring the buffering effects of religion. Social Science and Medicine, 71(1), 196–204. https://doi.org/10.1016/j.socscimed.2010.03.015
Cheng, H., Lin, S., & Cha, C. H. (2015). Perceived discrimination, intergenerational family conflicts, and depressive symptoms in foreign-born and U.S.-born Asian American emerging adults. Asian American Journal of Psychology, 6, 107–116. https://doi.org/10.1037/a0038710
Corcoran, K. E., Scheitle, C. P., & Dabbs, E. (2021). Multiple (non)religious identities leads to undercounting religious nones and Asian religious identities. Journal for the Scientific Study of Religion, 60(2), 424–441. https://doi.org/10.1111/jssr.12719
Ellison, C. G., & Burdette, A. M. (2012). Religion and the sense of control among U.S. adults. Sociology of Religion, 73(1), 1–22. https://doi.org/10.1093/socrel/srr035
Ellison, C. G., Burdette, A. M., & Hill, T. D. (2009a). Blessed assurance: Religion, anxiety, and tranquility among U.S. adults. Social Science Research, 38(3), 656–667. https://doi.org/10.1016/j.ssresearch.2009a.02.002
Ellison, C. G., Finch, B. K., Ryan, D. N., & Salinas, J. J. (2009b). Religious involvement and depressive symptoms among Mexican-origin adults in California. Journal of Community Psychology, 37(2), 171–193. https://doi.org/10.1002/jcop.20287
Ellison, C. G., & Lee, J. (2010). Spiritual struggles and psychological distress: Is there a dark side of religion? Social Indicator Research, 98, 501–517. https://doi.org/10.1007/s11205-009-9553-3
Ellison, C. G., Roalson, L. A., Guillory, J. M., Flannelly, K. J., & Marcum, J. P. (2010). Religious resources, spiritual struggles, and mental health in a nationwide sample of PCUSA clergy. Pastoral Psychology, 59(3), 287–304. https://doi.org/10.1007/s11089-009-0239-1
Exline, J. J. (2002). Stumbling blocks on the religious road: Fractured relationships, nagging vices, and the inner struggle to believe. Psychological Inquiry, 13(3), 182–189. https://doi.org/10.1207/S15327965PLI1303_03
Iwamura, J. N., Joshi, K. Y., Suh, S., & Wong, J. (2014). Reflections on the Pew Forum on religion and public life’s Asian Americans: A mosaic of faiths data and report. Amerasia Journal, 40(1), 1–16. https://doi.org/10.17953/amer.40.1.t1nt4407v3120734
Jeung, R. M., Fong, S. S., & Kim, H. J. (2019). Family sacrifices: The worldviews and ethics of Chinese Americans. Oxford University Press.
Kim, P. Y. (2017). Revisiting and extending the role of religious coping in the racism-mental health relation among Christian, Asian American Students. Psychology & Theology, 45(3), 166–181. https://doi.org/10.1177/009164711704500302
Kim, P. Y., Kendall, D. L., & Webb, M. (2015). Religious coping moderates the relation between racism and psychological well-being among Christian Asian American college students. Journal of Counseling Psychology, 62(1), 87–94. https://doi.org/10.1037/cou0000055
Lovibond, S. H., & Lovibond, P. (1995). Manual for the depression anxiety & stress scales (2nd ed.). Psychology Foundation.
McLaughlin, E. C., Tolan, C., & Watts, A. (2021). What we know about Robert Aaron Long, the suspect in Atlanta spa shootings. CNN. https://www.cnn.com/2021/03/17/us/robert-aaron-long-suspected-shooter/index.html.
Mental Health America. (2022). How race matters: What we can learn from mental health America’s screening in 2020. https://mhanational.org/mental-health-data-2020#:~:text=In%202020%2C%20Asian%20or%20Pacific,2019%2C%20at%20about%205%20percent.
Meyer, I. H. (2003). Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychological Bulletin, 129, 674–697. https://doi.org/10.1037/0033-2909.129.5.674
Nie, F., & Olson, D. V. A. (2016). Demonic influence: The negative mental health effects of belief in demons. Journal for the Scientific Study of Religion, 55(3), 498–515. https://doi.org/10.1111/jssr.12287
Pargament, K. I. (2002). The bitter and the sweet: An evaluation of the costs and benefits of religiousness. Psychological Inquiry, 13(3), 168–181. https://doi.org/10.1207/S15327965PLI1303_02
Pargament, K. I., Ensing, D. S., Falgout, K., Olsen, H., Reilly, B., Haitsma, K. V., & Warren, R. (1990). God help me (I): Religious coping efforts as predictors of the outcomes to significant negative life events. American Journal of Community Psychology, 18(6), 793–824. https://doi.org/10.1007/BF00938065
Pargament, K. I., Feuille, M., & Burdzy, D. (2011). The brief RCOPE: Current psychometric status of a short measure of religious coping. Religions, 2, 51–76. https://doi.org/10.3390/rel2010051
Pargament, K. I., Koenig, H. G., Tarakeshwar, N., & Hahn, J. (2004). Religious coping methods as predictors of psychological, physical and spiritual outcomes among medically ill elderly patients. Journal of Health Psychology, 9(6), 713–730. https://doi.org/10.1177/1359105304045366
Pew Research Center. (2012). Asian Americans: A mosaic of faiths. https://www.pewresearch.org/religion/2012/07/19/asian-americans-a-mosaic-of-faiths-overview/#:~:text=Religious%20Affiliation,-The%20survey%20finds&text=Roughly%20one%2Din%2Dseven%20Asian,followers%20of%20numerous%20other%20faiths.&text=Thus%2C%20Asian%20Americans%20are%20more,is%20overwhelmingly%20Christian%20(75%25).
Pew Research Center. (2020). Many Black, Asian Americans say they have experienced discrimination amid coronavirus. https://www.pewresearch.org/social-trends/2020/07/01/many-black-and-asian-americans-say-they-have-experienced-discrimination-amid-the-covid-19-outbreak/
Pew Research Center. (2021a). Key facts about Asian Americans, a diverse and growing population. https://www.pewresearch.org/fact-tank/2021a/04/29/key-facts-about-asian-americans/#:~:text=Chinese%20Americans%20are%20the%20largest,(or%204.2%20million%20people
Pew Research Center. (2021b). Key facts about Asian origin groups in the U.S. https://www.pewresearch.org/fact-tank/2021b/04/29/key-facts-about-asian-origin-groups-in-the-u-s/
Stop AAPI Hate. (2021). Stop AAPI hate national report. https://stopaapihate.org/national-report-through-december-31-2021/
Yoo, H. C., Steger, M. F., & Lee, R. M. (2010). Validation of the subtle and blatant racism scale for Asian American college students (SABR-A2). Cultural Diversity and Ethnic Minority Psychology, 16, 323–334. https://doi.org/10.1037/a0018674
Funding
This work was supported by the Jack Shand Research Grants of the Society for the Scientific Study of Religion, grant number JSRG2021-7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author declares no conflict of interest.
Ethical Approval
The study was conducted according to the guidelines of the Declaration of Helsinki and has been exempted from Institutional Review Board (IRB) review in accordance with Federal regulations (Protocol Code: 04210-2021). The IRB, a university committee established by Federal law, protects the rights and welfare of research participants.
Informed Consent
Informed consent was obtained from all subjects involved in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendix 1: Bivariate Associations for Some Main Variables
Negative Religious Coping | Subtle Racism | |
|---|---|---|
Negative religious coping | – | .27*** |
Subtle racism | .27*** | – |
Ethnicity | ||
Indian | 3.78*** | .78 |
Chinese | − 2.18* | − .67 |
Pilipino | − .49 | − .23 |
Other | − 1.03 | .08 |
Religious Tradition | ||
Christianity | 1.66 | − .44 |
Buddhism | − 1.45 | 1.42 |
Hinduism | 2.37* | − 1.06 |
Islam | 3.03** | 1.35 |
Other religions | .08 | − 1.38 |
Mixed religions | − 5.09*** | − .31 |
None | .50 | .90 |
Appendix 2: Ordinary Least Square Regression of Mental Health on Racism and Religious Coping (Full Model)
Dependent variables | Depression | Anxiety | Stress | |||
|---|---|---|---|---|---|---|
Model 1 | Model 2 | Model 3 | ||||
Key independent variables | B | SE | B | SE | B | SE |
Subtle racism | 0.23** | 0.09 | 0.22** | 0.08 | 0.23** | 0.08 |
Blatant racism | 0.10 | 0.1 | 0.19 | 0.10 | 0.13 | 0.09 |
Positive religious coping | 0.03 | 0.07 | 0.06 | 0.06 | 0.02 | 0.06 |
Negative religious coping | 0.49*** | 0.06 | 0.39*** | 0.06 | 0.39*** | 0.06 |
Control variables | ||||||
Religiosity | − 1.04* | 0.48 | − 0.48 | 0.39 | − 0.50 | 0.45 |
Religious affiliation (ref = Christianity) | ||||||
Buddhism | − .68 | 1.03 | − .90 | .78 | − .77 | .93 |
Hinduism | − .56 | 1.14 | − .40 | .96 | − 1.24 | 1.04 |
Islam | − .09 | 1.22 | .42 | 1.06 | .15 | 1.26 |
Other religion | − 0.41 | 1.12 | 1.20 | 0.95 | − 0.87 | 1.15 |
More than one religion | 1.17 | .99 | 0.44 | 0.86 | 0.14 | 0.86 |
None | 1.02 | 0.86 | 1.30 | 0.72 | 1.38 | 0.85 |
Female | 0.94 | 0.89 | 0.25 | 0.43 | 0.27 | 0.48 |
Ethnicity (ref = Asian Indian) | ||||||
Chinese | − 0.53 | 0.92 | − 1.30 | 0.81 | − 1.69 | 0.91 |
Pilipino | 0.46 | 0.98 | 0.14 | 0.79 | 0.04 | 0.95 |
Other | − 0.85 | 0.89 | − 1.49 | 0.76 | − 1.03 | 0.85 |
Age | − 0.06* | 0.02 | − 0.05* | 0.02 | − 0.06** | 0.02 |
Educational attainment | − 0.53* | 0.21 | − 0.38* | 0.17 | − 0.34 | 0.18 |
Fully employed | − 0.96 | 0.51 | − 0.85 | 0.45 | − 0.69 | 0.47 |
Income | 0.04 | 0.09 | 0.08 | 0.07 | 0.11 | 0.08 |
Married | − 1.44* | 0.68 | − 0.58 | 0.58 | − 1.08 | 0.62 |
Number of children | 0.01 | 0.28 | 0.05 | 0.28 | 0.28 | 0.25 |
Length of residence | − 0.13 | 0.14 | − 0.21 | 0.11 | − 0.22 | 0.13 |
Living environment (ref = rural area) | ||||||
Small city/town | − 0.22 | 0.88 | − 0.57 | 0.90 | − 0.72 | 0.83 |
Suburb near a mid-sized city | 0.74 | 0.90 | 0.45 | 0.86 | 0.19 | 0.86 |
Suburb near a large city | 0.44 | 0.78 | 0.13 | 0.79 | 0.26 | 0.75 |
Mid-sized city | 1.43 | 1.08 | 0.39 | 1.00 | 0.40 | 0.99 |
Large city | 0.57 | 0.86 | .95 | 0.91 | − 0.19 | 0.81 |
Number of cases | 330 | 330 | 330 | |||
R-squared | 0.49 | 0.52 | 0.46 | |||
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Nie, F. Asian Hate, Minority Stress, and Religious Coping: A Study of Asian and Asian American Adults in the USA During the COVID-19 Pandemic. J Relig Health 62, 681–701 (2023). https://doi.org/10.1007/s10943-022-01693-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10943-022-01693-4