Abstract
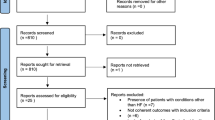
Cardiovascular diseases are the main cause of mortality in the world, generating important socioeconomic and cultural impacts. Spirituality has been associated with the main risk factors for acute myocardial infarction, influencing lifestyle, and drug treatment compliance. Estimate the level of spiritual well-being and its association with coronary artery disease. We conducted a case–control study with 88 adults (42 cases and 46 controls) individually interviewed. Using a spiritual well-being scale and collecting socioeconomic and demographic information. We compared groups by Chi-square and Mann–Whitney tests. Friedman’s analysis of variance was used to evaluate the differences between the values assigned to the scale items in each group. Statistically, there was no significant difference between categories and levels of spiritual well-being in any of the groups. Both had high rates, driven by the high level of religious well-being. There was no difference between the rates attributed to the items on the subscale of religious well-being, in the case or control groups (p = 0.959 and p = 0.817). However, the existential well-being subscale revealed variability between the scores attributed to each item in both groups (p < 0.001). The results revealed a high level of spiritual well-being in the analyzed sample. There was no correlation between the levels of spiritual, religious, and existential well-being with coronary artery disease, possibly due to the reduced ability of the religious well-being subscale to discriminate between groups.

Similar content being viewed by others
References
Alexander, M.-A. (2012). Implicações dos estudos brasileiros em psiquiatria e espiritualidade. Revista de Psiquiatria Clínica, 39(5), 181. https://doi.org/10.1590/S0101-60832012000500008.
Alexander, M.-A., Ilana, P., Marcos, Z., & Ronaldo, L. (2010). Envolvimento religioso e fatores sociodemográficos: Resultados de um levantamento nacional no Brasil. Revista de Psiquiatria Clínica, 37(1), 12–15. https://doi.org/10.1590/S0101-60832010000100003.
Alexandre, V. S. M., Rosa, S. P. L., de Jesus, M. J., & Lessa, H. B. (2003). Relação entre bem-estar espiritual e transtornos psiquiátricos menores: Estudo transversal. Revista de Saúde Pública, 37(4), 440–445. https://doi.org/10.1590/S0034-89102003000400008.
Amour, J. M., Samuel, N., Hayley, H., Bruna, B., Denise, G., da Gloria Miotto, W. M., et al. (2015). Spirituality, gender, and drug use among students from one University in Barbados. Texto & Contexto—Enfermagem, 24(spe), 117–124. https://doi.org/10.1590/0104-07072015001140014.
Avezum, Á., Piegas, L. S., & Pereira, J. C. R. (2005). Fatores de Risco Associados com Infarto Agudo do Miocárdio na Região Metropolitana de São Paulo. Uma Região Desenvolvida em um País em Desenvolvimento (Vol. 84, No. 3). Março: Arquivos Brasileiros de Cardiologia.
Bekelman, et al. (2007). Spiritual well-being and depression in heart failure. Society of General Internal Medicine, 22, 470–477.
Bergh, C., Udumyan, R., Fall, K., Almroth, H., & Montgomery, S. (2015). Stress resilience and physical fitness in adolescence and risk of coronary heart disease in middle age. Heart, 101(8), 623–629. https://doi.org/10.1136/heartjnl-2014-306703.
Bhatnagar, P., Wickramasinghe, K., Williams, J., Rayner, M., & Townsend, N. (2015). The epidemiology of cardiovascular disease in the UK 2014. Heart, 101(15), 1182–1189. https://doi.org/10.1136/heartjnl-2015-307516.
Boletim Eletrônico da CEInfo Edição Especial. (2013). Mortalidade 2013Aspectos da mortalidade no município de São Paulo, Fevereiro/2015 Ano 6.
Brasil. Ministério da Saúde. (2015). Brasília: Ministério da Saúde. [Acesso 8 out2015]. Disponível em: http://portal.saude.gov.br/saude.
Bufford, R. K., Paloutzian, R. F., & Ellison, C. W. (1991). Norms for the spiritual well-being scale. Journal of Psychology & Theology, 19, 56–70.
Burg, M. M., Meadows, J., Shimbo, D., Davidson, K. W., Schwartz, J. E., & Soufer, R. (2014). Confluence of depression and acute psychological stress among patients with stable coronary heart disease: Effects on myocardial perfusion. Journal of the American Heart Association: Cardiovascular and Cerebrovascular Disease, 3(6), e000898. https://doi.org/10.1161/JAHA.114.000898.
Carmen, D. E., & Maria, B. S. (2012). Transição demográfica e epidemiológica: A Epidemiologia e Serviços de Saúde revisita e atualiza o tema. Epidemiologia e Serviços de Saúde, 21(4), 529–532. https://doi.org/10.5123/S1679-49742012000400001.
Cunningham, R., Poppe, K., Peterson, D., Every-Palmer, S., Soosay, I., & Jackson, R. (2019). Prediction of cardiovascular disease risk among people with severe mental illness: A cohort study. PLoS ONE, 14(9), e0221521. https://doi.org/10.1371/journal.pone.0221521.
DCNT. (2011). Plano de ações estratégicas para o enfrentamento das doenças crônicas não transmissíveis (DCNT) no Brasil 2011–2022. Ministério da Saúde. Secretaria de Vigilância em Saúde (p. 160). Brasília: Departamento de Análise de Situação de Saúde, Ministério da Saúde (Série B. Textos Básicos de Saúde).
de Souza, G. A. M., & Cristina, P. S. (2009). Adaptação transcultural e avaliação da consistência interna da versão em português da Spirituality Self Rating Scale (SSRS). Revista de Psiquiatria Clínica, 36(1), 10–15. https://doi.org/10.1590/S0101-60832009000100002.
Fernandes, M. L., Castellá, S. J., & Dalbosco, D. A. D. (2009). Adaptação e validação da Escala de Bem-estar Espiritual (EBE): Adaptation and validation of Spiritual Well-Being Scale (SWS). Avaliação Psicológica, 8(2), 179–186.
Giancarlo, L., de Camargo, A. L. G., & Lamas, G. A. (2010). Espiritualidade no paciente em diálise: o nefrologista deve abordar? Jornal Brasileiro de Nefrologia, 32(1), 128–132. https://doi.org/10.1590/S0101-28002010000100020.
Giancarlo, L., Granero, L. A. L., & Homero, V. (2013). Measuring spirituality and religiosity in clinical research: A systematic review of instruments available in the Portuguese language. Sao Paulo medical journal, 131(2), 112–122.
Hackett, R. A., Hudson, J. L., & Chilcot, J. (2020). Loneliness and type 2 diabetes incidence: Findings from the English longitudinal study of ageing. Diabetologia. https://doi.org/10.1007/s00125-020-05258-6.
Ho, P. M., Bryson, C. L., & Rumsfeld, J. S. (2009). Medication adherence. Its importance in cardiovascular outcomes. Circulation, 119(23), 3028–3035. https://doi.org/10.1161/circulationaha.108.768986.
Holt-Lunstad, J., Steffen, P. R., Sandberg, J., & Jensen, B. (2011). Understanding the connection between spiritual well-being and physical health: An examination of ambulatory blood pressure, inflammation, blood lipids and fasting glucose. Behavioral Medicine, 34, 477. https://doi.org/10.1007/s10865-011-9343-7.
Joanne, O. K. (2015). Conhecimento necessário para usar o poder da espiritualidade nos cuidados à saúde. Acta Paulista de Enfermagem, 28(2), 3–4. https://doi.org/10.1590/1982-0194201500017.
Keenan, J. (2017). Improving adherence to medication for secondary cardiovascular disease prevention. European Journal of Preventive Cardiology, 24(3S), 29–35.
Kivimäki, M., Jokela, M., Nyberg, S. T., Singh-Manoux, A., et al. (2015). Long working hours and risk of coronary heart disease and stroke: A systematic review and meta-analysis of published and unpublished data for 603 838 individuals. Lancet, 386, 1739–1746.
Koenig, H. G. (2012). Religion, spirituality and health: The research and clinical implications. ISRN Psychiatry, 2012, 33. https://doi.org/10.5402/2012/278730.
Lanas, F., Avezum, Á., Bautista, L. E., Diaz, R., Luna, M., Islam, S., et al. (2007). Risk factors for acute myocardial infarction in Latin America: The INTERHEART Latin American study, for the INTERHEART Investigators in Latin America. Revista Brasileira de Hipertensao, 14(4), 278–279.
Lewis, M., Chondros, P., Mihalopoulos, C., Lee, Y. Y., Gun, J. M., Harvey, C., et al. (2020). The assertive cardiac care trial: A randomised controlled trial of a coproduced assertive cardiac care intervention to reduce absolute cardiovascular disease risk in people with severe mental illness in the primary care setting. Contemporary Clinical Trials. https://doi.org/10.1016/j.cct.2020.106143.
Li, J., Zhang, M., Loerbroks, A., Peter, A., & Siegrist, J. (2015). Work stress and the risk of recurrent coronary heart disease events: A systematic review and meta-analysis. International Journal of Occupational Medicine and Environmental Health, 28(1), 8–19. https://doi.org/10.2478/s13382-014-0303-7.
Lucchese, F. A., & Koenig, H. G. (2013). Religion, spirituality and cardiovascular disease: Research, clinical implications, and opportunities in Brazil. Revista Brasileira de Cirurgia Cardiovascular, 28(1), 103–128.
Meijer, A., et al. (2011). Prognostic association of depression following myocardial infarction with mortality and cardiovascular events: A meta-analysis of 25 years of research. General Hospital Psychiatry, 33, 203–216.
Mills, P. J., Wilson, K., & Iqbal, N. (2015). Depressive symptoms and spiritual wellbeing in asymptomatic heart failure patients. Journal of Behavioral Medicine, 38(3), 407–415. https://doi.org/10.1007/s10865-014-9615-0.
Ministério da Saúde (BR). (2012). Secretaria de Vigilância em Saúde. Saúde Brasil 2012: uma análise da situação de saúde e dos 40 anos do Programa Nacional de Imunização, Brasília (DF).
Park, C. L., Lim, H., Suresh, D. P., & Bliss, D. E. (2014). Dimensions of religiousness and spirituality as predictors of well-being in advanced chronic heart failure patients. Journal of Religion and Health, 53, 579–590.
Penna, G. H., & Álvaro, A. (2007). O impacto da espiritualidade na saúde física. Revista de Psiquiatria Clínica, 34(Suppl 1), 88–94. https://doi.org/10.1590/S0101-60832007000700012.
Plante, T. B., Koh, I., Judd, S. E., Howard, G., Howard, V. J., Zakai, N. A., et al. (2020). Life’s simple 7 and incident hypertension: The REGARDS study. Journal of the American Heart Association. https://doi.org/10.1161/jaha.120.016482.
Rankinen, T., Sarzynski, M. A., Ghosh, S., & Bouchard, C. (2015). Are there genetic paths common to obesity, cardiovascular disease outcomes, and cardiovascular risk factors? Circulation Research, 116(5), 909–922.
Sens IBGE. (2010). Instituto Brasileiro de Geografia e Estatística (BR). Censo Demográfico 2010: Características gerais da população, religião e pessoas com deficiência, Brasil.
Siegel, S. E., & Castellan, N. J., Jr. (2006). Estatística não paramétrica para ciências do comportamento (p. 448). Porto Alegre: Segunda edição, Artmed.
Souto, A. J., Adams, G. L., Hoefel, N. A., Brugalli, Z. M. C., et al. (2016). Association between spirituality and adherence to management in outpatients with heart failure. Arquivos Brasileiros de Cardiologia, 106(6), 491–501. https://doi.org/10.5935/abc.20160076.
Tauanay, T. C. D., et al. (2012). Validação da versão brasileira da escala de religiosidade de Duke (DUREL). Revista de Psiquiatria Clínica, 39(4), 130–135.
Yusuf, S., Rangarajan, S., Teo, K., Islam, S., Li, W., Liu, L., et al. (2014). Cardiovascular risk and events in 17 low-, middle-, and high-income countries. New England Journal of Medicine, 371, 818–827. https://doi.org/10.1056/NEJMoa1311890.
Zangiacomi, M. E., dos Santos, A. R. G., Rodrigues, G. F., & de Duarte, C. A. C. (2013). Notas sobre a versão em língua portuguesa da Escala de Bem-Estar Espiritual. Jornal Brasileiro de Psiquiatria, 62(1), 76–80. https://doi.org/10.1590/S0047-20852013000100010.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
de Eston Armond, R., de Eston Armond, J., Konstantyner, T. et al. Spiritual Well-Being and Its Association with Coronary Artery Disease. J Relig Health 61, 467–478 (2022). https://doi.org/10.1007/s10943-020-01115-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10943-020-01115-3