Abstract
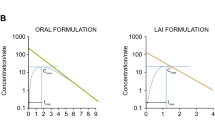
Mavoglurant (MVG) is an antagonist at the metabotropic glutamate receptor-5 currently under clinical development at Novartis Pharma AG for the treatment of central nervous system diseases. The aim of this study was to develop and optimise a population whole-body physiologically-based pharmacokinetic (WBPBPK) model for MVG, to predict the impact of drug–drug interaction (DDI) and age on its pharmacokinetics. In a first step, the model was fitted to intravenous (IV) data from a clinical study in adults using a Bayesian approach. In a second step, the optimised model was used together with a mechanistic absorption model for exploratory Monte Carlo simulations. The ability of the model to predict MVG pharmacokinetics when orally co-administered with ketoconazole in adults or administered alone in 3–11 year-old children was evaluated using data from three other clinical studies. The population model provided a good description of both the median trend and variability in MVG plasma pharmacokinetics following IV administration in adults. The Bayesian approach offered a continuous flow of information from pre-clinical to clinical studies. Prediction of the DDI with ketoconazole was consistent with the results of a non-compartmental analysis of the clinical data (threefold increase in systemic exposure). Scaling of the WBPBPK model allowed reasonable extrapolation of MVG pharmacokinetics from adults to children. The model can be used to predict plasma and brain (target site) concentration–time profiles following oral administration of various immediate-release formulations of MVG alone or when co-administered with other drugs, in adults as well as in children.








Similar content being viewed by others
References
Wendling T, Ogungbenro K, Pigeolet E, Dumitras S, Woessner R, Aarons L (2015) Model-based evaluation of the impact of formulation and food intake on the complex oral absorption of mavoglurant in healthy subjects. Pharm Res 32(5):1764–1778. doi:10.1007/s11095-014-1574-1
Walles M, Wolf T, Jin Y, Ritzau M, Leuthold LA, Krauser J, Gschwind HP, Carcache D, Kittelmann M, Ocwieja M, Ufer M, Woessner R, Chakraborty A, Swart P (2013) Metabolism and disposition of the metabotropic glutamate receptor 5 antagonist (mGluR5) mavoglurant (AFQ056) in healthy subjects. Drug Metab Dispos 41(9):1626–1641. doi:10.1124/dmd.112.050716
Wendling T, Ogungbenro K, Pigeolet E, Dumitras S, Woessner R, Aarons L (2014) Model-based evaluation of the impact of formulation and food intake on the complex oral absorption of mavoglurant in healthy subjects. Pharm Res. doi:10.1007/s11095-014-1574-1
Edginton AN, Theil FP, Schmitt W, Willmann S (2008) Whole body physiologically-based pharmacokinetic models: their use in clinical drug development. Expert Opin Drug Metab Toxicol 4(9):1143–1152. doi:10.1517/17425255.4.9.1143
Wakefield JC, Smith AFM (1994) Bayesian analysis of linear and non-linear population models by using the Gibbs sampler. Appl Stat 43:201–221
Yates JW (2006) Structural identifiability of physiologically based pharmacokinetic models. J Pharmacokinet Pharmacodyn 33(4):421–439. doi:10.1007/s10928-006-9011-7
Tsamandouras N, Rostami-Hodjegan A, Aarons L (2015) Combining the ‘bottom up’ and ‘top down’ approaches in pharmacokinetic modelling: fitting PBPK models to observed clinical data. Br J Clin Pharmacol 79(1):48–55. doi:10.1111/bcp.12234
Sheiner LB (1984) The population approach to pharmacokinetic data analysis: rationale and standard data analysis methods. Drug Metab Rev 15(1–2):153–171. doi:10.3109/03602538409015063
Wakefield JC (1996) The Bayesian analysis of population pharmacokinetic models. J Am Stat Assoc 91:61–76
Bois FY, Gelman A, Jiang J, Maszle DR, Zeise L, Alexeef G (1996) Population toxicokinetics of tetrachloroethylene. Arch Toxicol 70(6):347–355
Jonsson F, Johanson G (2001) Bayesian estimation of variability in adipose tissue blood flow in man by physiologically based pharmacokinetic modeling of inhalation exposure to toluene. Toxicology 157(3):177–193
Gueorguieva I, Aarons L, Rowland M (2006) Diazepam pharamacokinetics from preclinical to phase I using a Bayesian population physiologically based pharmacokinetic model with informative prior distributions in WinBUGS. J Pharmacokinet Pharmacodyn 33(5):571–594. doi:10.1007/s10928-006-9023-3
Nestorov I (2007) Whole-body physiologically based pharmacokinetic models. Expert Opin Drug Metab Toxicol 3(2):235–249. doi:10.1517/17425255.3.2.235
Willmann S, Hohn K, Edginton A, Sevestre M, Solodenko J, Weiss W, Lippert J, Schmitt W (2007) Development of a physiology-based whole-body population model for assessing the influence of individual variability on the pharmacokinetics of drugs. J Pharmacokinet Pharmacodyn 34(3):401–431. doi:10.1007/s10928-007-9053-5
Gomez-Mancilla B, Berry-Kravis E, Hagerman R, von Raison F, Apostol G, Ufer M, Gasparini F, Jacquemont S (2014) Development of mavoglurant and its potential for the treatment of fragile X syndrome. Expert Opin Investig Drugs 23(1):125–134. doi:10.1517/13543784.2014.857400
Jakab A, Winter S, Raccuglia M, Picard F, Dumitras S, Woessner R, Mistry S, Chudasama J, Guttikar S, Kretz O (2013) Validation of an LC-MS/MS method for the quantitative determination of mavoglurant (AFQ056) in human plasma. Anal Bioanal Chem 405(1):215–223. doi:10.1007/s00216-012-6456-y
Yu LX, Lipka E, Crison JR, Amidon GL (1996) Transport approaches to the biopharmaceutical design of oral drug delivery systems: prediction of intestinal absorption. Adv Drug Deliv Rev 19(3):359–376
Hintz RJ, Johnson KC (1989) The effect of particle size distribution on dissolution rate and oral absorption. Int J Pharm 51(9–17):9–17
Takano R, Sugano K, Higashida A, Hayashi Y, Machida M, Aso Y, Yamashita S (2006) Oral absorption of poorly water-soluble drugs: computer simulation of fraction absorbed in humans from a miniscale dissolution test. Pharm Res 23(6):1144–1156. doi:10.1007/s11095-006-0162-4
Nestorov I (2001) Modelling and simulation of variability and uncertainty in toxicokinetics and pharmacokinetics. Toxicol Lett 120(1–3):411–420
Howgate EM, Rowland Yeo K, Proctor NJ, Tucker GT, Rostami-Hodjegan A (2006) Prediction of in vivo drug clearance from in vitro data. I: impact of inter-individual variability. Xenobiotica 36(6):473–497. doi:10.1080/00498250600683197
Fieller EC (1954) Some problems in interval estimation. J R Stat Soc B 16(2):175–185
Jansson R, Bredberg U, Ashton M (2008) Prediction of drug tissue to plasma concentration ratios using a measured volume of distribution in combination with lipophilicity. J Pharm Sci 97(6):2324–2339. doi:10.1002/jps.21130
Boeckmann AJ, Sheiner LB, Beal SL (2013) NONMEM users guide—part VIII. ICON Development Solutions, Hanover
Martins JRRA, Sturdza P, Alonson JJ (2003) The complex-step derivative approximation. ACM Trans Math Softw 29:245–262
Yetter RA, Dryer FL, Rabitz H (1985) Some interpretive aspects of elementary sensitivity gradients in combustion kinetics modeling. Combust Flame 59:107–133
Gelman A, Rubin DB (1992) Inference from iterative simulation using multiple sequences. Stat Sci 7(4):457–472. doi:10.2307/2246093
Best NG, Cowles MK, Vines SK (1995) CODA manual version 0.30. MRC Biostatistics Uni, Cambridge
Oberle RL, Chen TS, Lloyd C, Barnett JL, Owyang C, Meyer J, Amidon GL (1990) The influence of the interdigestive migrating myoelectric complex on the gastric emptying of liquids. Gastroenterology 99(5):1275–1282
Yu LX, Amidon GL (1998) Saturable small intestinal drug absorption in humans: modeling and interpretation of cefatrizine data. Eur J Pharm Biopharm 45(2):199–203
Tsamandouras N, Wendling T, Rostami-Hodjegan A, Galetin A, Aarons L (2015) Incorporation of stochastic variability in mechanistic population pharmacokinetic models: handling the physiological constraints using normal transformations. J Pharmacokinet Pharmacodyn. doi:10.1007/s10928-015-9418-0
Schiller C, Frohlich CP, Giessmann T, Siegmund W, Monnikes H, Hosten N, Weitschies W (2005) Intestinal fluid volumes and transit of dosage forms as assessed by magnetic resonance imaging. Aliment Pharmacol Ther 22(10):971–979. doi:10.1111/j.1365-2036.2005.02683.x
Lennernas H (2014) Human in vivo regional intestinal permeability: importance for pharmaceutical drug development. Mol Pharm 11(1):12–23. doi:10.1021/mp4003392
Valentin J (2002) Guide for the practical application of the ICRP Human Respiratory Tract Model. A report of ICRP supporting guidance 3: approved by ICRP committee 2 in October 2000. Ann ICRP 32(1–2):13–306
Matheson PJ, Wilson MA, Garrison RN (2000) Regulation of intestinal blood flow. J Surg Res 93(1):182–196. doi:10.1006/jsre.2000.5862
Paine MF, Khalighi M, Fisher JM, Shen DD, Kunze KL, Marsh CL, Perkins JD, Thummel KE (1997) Characterization of interintestinal and intraintestinal variations in human CYP3A-dependent metabolism. J Pharm Exp Ther 283(3):1552–1562
Sun D, Lennernas H, Welage LS, Barnett JL, Landowski CP, Foster D, Fleisher D, Lee KD, Amidon GL (2002) Comparison of human duodenum and Caco-2 gene expression profiles for 12,000 gene sequences tags and correlation with permeability of 26 drugs. Pharm Res 19(10):1400–1416
Sjogren E, Abrahamsson B, Augustijns P, Becker D, Bolger MB, Brewster M, Brouwers J, Flanagan T, Harwood M, Heinen C, Holm R, Juretschke HP, Kubbinga M, Lindahl A, Lukacova V, Munster U, Neuhoff S, Nguyen MA, Peer A, Reppas C, Hodjegan AR, Tannergren C, Weitschies W, Wilson C, Zane P, Lennernas H, Langguth P (2014) In vivo methods for drug absorption - comparative physiologies, model selection, correlations with in vitro methods (IVIVC), and applications for formulation/API/excipient characterization including food effects. Eur J Pharm Sci 57:99–151. doi:10.1016/j.ejps.2014.02.010
Zhao P, Ragueneau-Majlessi I, Zhang L, Strong JM, Reynolds KS, Levy RH, Thummel KE, Huang SM (2009) Quantitative evaluation of pharmacokinetic inhibition of CYP3A substrates by ketoconazole: a simulation study. J Clin Pharmacol 49(3):351–359. doi:10.1177/0091270008331196
Walsky RL, Gaman EA, Obach RS (2005) Examination of 209 drugs for inhibition of cytochrome P450 2C8. J Clin Pharmacol 45(1):68–78. doi:10.1177/0091270004270642
Stresser DM, Broudy MI, Ho T, Cargill CE, Blanchard AP, Sharma R, Dandeneau AA, Goodwin JJ, Turner SD, Erve JC, Patten CJ, Dehal SS, Crespi CL (2004) Highly selective inhibition of human CYP3Aa in vitro by azamulin and evidence that inhibition is irreversible. Drug Metab Dispos 32(1):105–112. doi:10.1124/dmd.32.1.105
Rowland Yeo K, Jamei M, Yang J, Tucker GT, Rostami-Hodjegan A (2010) Physiologically based mechanistic modelling to predict complex drug–drug interactions involving simultaneous competitive and time-dependent enzyme inhibition by parent compound and its metabolite in both liver and gut—the effect of diltiazem on the time-course of exposure to triazolam. Eur J Pharm Sci 39(5):298–309. doi:10.1016/j.ejps.2009.12.002
Johnson TN, Rostami-Hodjegan A, Tucker GT (2006) Prediction of the clearance of eleven drugs and associated variability in neonates, infants and children. Clin Pharmacokinet 45(9):931–956. doi:10.2165/00003088-200645090-00005
Edginton AN, Schmitt W, Willmann S (2006) Development and evaluation of a generic physiologically based pharmacokinetic model for children. Clin Pharmacokinet 45(10):1013–1034. doi:10.2165/00003088-200645100-00005
Edginton AN, Schmitt W, Voith B, Willmann S (2006) A mechanistic approach for the scaling of clearance in children. Clin Pharmacokinet 45(7):683–704. doi:10.2165/00003088-200645070-00004
ICRP (1975) Report of the task group on reference man. ICRP Publication 23, Pergamon Press, Oxford
Dokoumetzidis A, Aarons L (2009) A method for robust model order reduction in pharmacokinetics. J Pharmacokinet Pharmacodyn 36(6):613–628. doi:10.1007/s10928-009-9141-9
Jorgensen AL, FitzGerald RJ, Oyee J, Pirmohamed M, Williamson PR (2012) Influence of CYP2C9 and VKORC1 on patient response to warfarin: a systematic review and meta-analysis. PLoS One 7(8):e44064. doi:10.1371/journal.pone.0044064
Wang J, Flanagan DR (1999) General solution for diffusion-controlled dissolution of spherical particles. 1. Theory. J Pharm Sci 88(7):731–738. doi:10.1021/js980236p
Wang J, Flanagan DR (2002) General solution for diffusion-controlled dissolution of spherical particles. 2. Evaluation of experimental data. J Pharm Sci 91(2):534–542
Berg D, Godau J, Trenkwalder C, Eggert K, Csoti I, Storch A, Huber H, Morelli-Canelo M, Stamelou M, Ries V, Wolz M, Schneider C, Di Paolo T, Gasparini F, Hariry S, Vandemeulebroecke M, Abi-Saab W, Cooke K, Johns D, Gomez-Mancilla B (2011) AFQ056 treatment of levodopa-induced dyskinesias: results of 2 randomized controlled trials. Mov Disord 26(7):1243–1250. doi:10.1002/mds.23616
Stocchi F, Rascol O, Destee A, Hattori N, Hauser RA, Lang AE, Poewe W, Stacy M, Tolosa E, Gao H, Nagel J, Merschhemke M, Graf A, Kenney C, Trenkwalder C (2013) AFQ056 in Parkinson patients with levodopa-induced dyskinesia: 13-week, randomized, dose-finding study. Mov Disord 28(13):1838–1846. doi:10.1002/mds.25561
Brown RP, Delp MD, Lindstedt SL, Rhomberg LR, Beliles RP (1997) Physiological parameter values for physiologically based pharmacokinetic models. Toxicol Ind Health 13(4):407–484
Yang J, Jamei M, Yeo KR, Tucker GT, Rostami-Hodjegan A (2007) Prediction of intestinal first-pass drug metabolism. Curr Drug Metab 8(7):676–684
Acknowledgments
The authors would like to thank Nikolaos Tsamandouras and Andres Olivares-Morales (Manchester Pharmacy School, The University of Manchester, Manchester, United-Kingdom) for fruitful discussions.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Thierry Wending is an employee of Novartis Pharma AG and a Ph.D. student at the University of Manchester.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Wendling, T., Dumitras, S., Ogungbenro, K. et al. Application of a Bayesian approach to physiological modelling of mavoglurant population pharmacokinetics. J Pharmacokinet Pharmacodyn 42, 639–657 (2015). https://doi.org/10.1007/s10928-015-9430-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10928-015-9430-4