Abstract
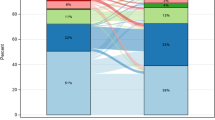
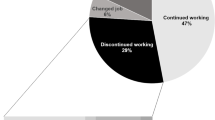
Purpose Work transitions among breast cancer survivors remain an underexplored area. We aimed to examine prevalence and determinants of changes in work status, and the effect of these changes on quality of life of breast cancer survivors. Methods A cross-sectional study of 410 female breast cancer survivors randomly drawn from a larger study sample pool (n = 2644), members of “Leumit” healthcare fund, who were diagnosed with primary nonmetastatic invasive breast cancer in the years 2002–2012. The study questionnaire included questions on work characteristics and health-related quality-of-life and was completed by all women contacted. Work transition was defined as a downgrade (from full-time to part-time), termination, or retirement, and was contrasted to no change in work status (retention of full-time or part-time). Work transition was assessed at two intervals: between breast cancer diagnosis and treatment, and between breast cancer diagnosis and time of the survey. Results A total of 206 breast cancer survivors (50%) were employed prior to their diagnosis, of whom 12% stopped working, and 79% downgraded to part-time during treatment. At the time of survey (mean 8 ± 3 years post-diagnosis), 33% of those employed prior to their diagnosis stopped working or retired, 48% downgraded to part-time, and 19% had no change in their work situation. Work transition between diagnosis and time of the survey was significantly associated with poorer quality-of-life. In multivariable analyses, work transition between diagnosis and time of the survey was positively associated with being immigrant compared to native-born Israeli (odds ratio (OR) 4.65; 95% confidence interval (CI) 1.91–11.37; P = .001), and inversely with education level of college or over compared to high school or less (OR 0.27; 95% CI 0.09–0.86; P = .026). Conclusions Breast cancer survivors with characteristics pointing at underprivileged social circumstances more often experienced changes in work status after surviving breast cancer, irrespective of diagnosis, comorbidity or treatment. Breast cancer patients with immigrant status and/or lower educational attainment need more support to be able to keep their job.



Similar content being viewed by others
Data Availability
The datasets generated during and/or analyzed during the current study are not publicly available to preserve the privacy of participants; but are available from the corresponding author on reasonable request.
Abbreviations
- BCS:
-
Breast cancer survivors
- CI:
-
Confidence interval
- Dx:
-
Diagnosis
- INCR:
-
Israel National Cancer Registry
- LHS:
-
Leumit Health Services
- OR:
-
Odds ratio
- P :
-
P value
- QOL:
-
Quality-of-life
- SD:
-
Standard deviation
- SER:
-
Standardized employment ratio
- SF-36:
-
36-Item short-form health survey
- WT:
-
Work transition
- χ2 :
-
Chi square
References
Hoving JL, Broekhuizen ML, Frings-Dresen MH. Return to work of breast cancer survivors: a systematic review of intervention studies. BMC Cancer. 2009;9(1):117.
Crist P. Functional challenges among late effects cancer survivors: a preliminary report on work engagement issues. Work 2013;46(4):369–379.
Nitkin P, Parkinson M, Schultz I. Cancer and work: a Canadian perspective; Toronto, ON: Canadian Association of Psychosocial Oncology; 2011. http://www.capo.ca/pdf/CancerandWork-ACanadianPerspective.pdf. Accessed 9 Apr 2018.
Drolet M, Maunsell E, Brisson J, Brisson C, Masse B, Deschenes L. Not working 3 years after breast cancer: predictors in a population-based study. J Clin Oncol. 2005;23(33):8305–8312.
Luker K, Campbell M, Amir Z, Davies L. A UK survey of the impact of cancer on employment. Occup Med. 2013;63(7):494–500.
Ferrell BR, Grant MM, Funk B, Otis-Green S, Garcia N. Quality of life in breast cancer survivors as identified by focus groups. Psychooncology 1997;6(1):13–23.
Antao L, Shaw L, Ollson K, Reen K, To F, Bossers A, et al. Chronic pain in episodic illness and its influence on work occupations: a scoping review. Work 2013;44(1):11–36.
Mahar KK, BrintzenhofeSzoc K, Shields JJ. The impact of changes in employment status on psychosocial well-being: a study of breast cancer survivors. J Psychosoc Oncol. 2008;26(3):1–17.
Maunsell E, Drolet M, Brisson J, Brisson C, Masse B, Deschenes L. Work situation after breast cancer: results from a population-based study. J Natl Cancer Inst. 2004;96(24):1813–1822.
Mehnert A, de Boer A, Feuerstein M. Employment challenges for cancer survivors. Cancer 2013;119(Suppl 11):2151–2159.
Amir Z, Moran T, Walsh L, Iddenden R, Luker K. Return to paid work after cancer: a British experience. J Cancer Surviv. 2007;1(2):129–136.
Short PF, Vasey JJ, Tunceli K. Employment pathways in a large cohort of adult cancer survivors. Cancer 2005;103(6):1292–1301.
Johnsson A, Fornander T, Olsson M, Nystedt M, Johansson H, Rutqvist LE. Factors associated with return to work after breast cancer treatment. Acta Oncol. 2007;46(1):90–96.
Hassett MJ, O’Malley AJ, Keating NL. Factors influencing changes in employment among women with newly diagnosed breast cancer. Cancer 2009;115(12):2775–2782.
Fantoni SQ, Peugniez C, Duhamel A, Skrzypczak J, Frimat P, Leroyer A. Factors related to return to work by women with breast cancer in northern France. J Occup Rehabil. 2010;20(1):49–58.
Mols F, Thong MS, Vreugdenhil G, van de Poll-Franse LV. Long-term cancer survivors experience work changes after diagnosis: results of a population-based study. Psychooncology 2009;18(12):1252–1260.
Steiner JF, Cavender TA, Nowels CT, Beaty BL, Bradley CJ, Fairclough DL, et al. The impact of physical and psychosocial factors on work characteristics after cancer. Psychooncology 2008;17(2):138–147.
Bouknight RR, Bradley CJ, Luo Z. Correlates of return to work for breast cancer survivors. J Clin Oncol. 2006;24(3):345–353.
Bradley CJ, Bednarek HL. Employment patterns of long-term cancer survivors. Psychooncology 2002;11(3):188–198.
Peretz S. Compilation of legislation on health insurance. Tel Aviv: Bursi; 1996.
Israel National Cancer Registry. Female breast cancer in Israel: morbidity and mortality data update [Hebrew]; 2016.
National Insurance Institute of Israel. Laws and regulations. http://www.btl.gov.il. Accessed 9 Apr 2018.
Hamood R, Hamood H, Merhasin I, Keinan-Boker L. A feasibility study to assess the validity of administrative data sources and self-reported information of breast cancer survivors. Isr J Health Policy Res. 2016;5(1):50.
Hays RD, Sherbourne CD, Mazel RM. The RAND 36-item health survey 1.0. Health Econ. 1993;2(3):217–227.
Islam T, Dahlui M, Majid HA, Nahar AM, Mohd Taib NA, Su TT. MyBCC study group: factors associated with return to work of breast cancer survivors: a systematic review. BMC Public Health. 2014;14(Suppl 3):S8.
Provencher L, Hogue JC, Desbiens C, Poirier B, Poirier E, Boudreau D, Joyal M, Diorio C, Duchesne N, Chiquette J. Is clinical breast examination important for breast cancer detection? Curr Oncol. 2016;23(4):e332–e339.
Amoran OE, Toyobo OO. Predictors of breast self-examination as cancer prevention practice among women of reproductive age-group in a rural town in Nigeria. Niger Med J. 2015;56(3):185–189.
Schwab FD, Huang DJ, Schmid SM, Schotzau A, Guth U. Self-detection and clinical breast examination: comparison of the two “classical” physical examination methods for the diagnosis of breast cancer. Breast 2015;24(1):90–92.
Latest Population Statistics for Israel Press Release. Israel Central Bureau of Statistics [Hebrew]; 2016.
Spelten ER, Sprangers MA, Verbeek JH. Factors reported to influence the return to work of cancer survivors: a literature review. Psychooncology 2002;11(2):124–131.
Kennedy F, Haslam C, Munir F, Pryce J. Returning to work following cancer: a qualitative exploratory study into the experience of returning to work following cancer. Eur J Cancer Care. 2007;16(1):17–25.
Frazier LM, Miller VA, Horbelt DV, Delmore JE, Miller BE, Averett EP. Employment and quality of survivorship among women with cancer: domains not captured by quality of life instruments. Cancer Control. 2009;16(1):57–65.
Mujahid MS, Janz NK, Hawley ST, Griggs JJ, Hamilton AS, Graff J, Katz SJ. Racial/ethnic differences in job loss for women with breast cancer. J Cancer Surviv. 2011;5(1):102–111.
Remennick L. The challenge of early breast cancer detection among immigrant and minority women in multicultural societies. Breast J. 2006;12(Suppl 1):S103–S110.
Acknowledgements
Appreciation is expressed to the PhD advisory committee and all breast cancer survivors who participated in this study. We are grateful to Dr. Natan Kahan for his assistance and support with data acquisition and study approval.
Funding
Funding of this study was in part provided by a grant from the Council for Higher Education (Grant No. 11658745) in collaboration with the Graduate Studies Authority at the University of Haifa (Grant No. 11658760).
Author information
Authors and Affiliations
Contributions
RH had full access to all of the data in the study, performed the statistical analysis, interpreted the data, and drafted the manuscript. HH participated in the study concept and design, helped in data acquisition, evaluated the manuscript, and acted as the corresponding author. IM was responsible for data acquisition, participated in the statistical analysis, and helped to evaluate and edit the manuscript. LKB had substantial contribution to the study concept, its formalization and development, interpreted the data, and assisted in the drafting and refinement of the manuscript. All authors take responsibility for the integrity of the data and the accuracy of the data analysis, have read and approved the final manuscript. This work has been done in partial fulfillment of the requirements for a PhD degree of RH (supervised by LKB) in the School of Public health, in the University of Haifa.
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflicts of interest.
Ethical Approval
All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional review boards of LHS and University of Haifa and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Disclaimer
The results, conclusions, view and opinions contained herein are those of the authors and not to be construed as the official policy of Israel’s Ministry of Health, or of Leumit Health Organization.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Hamood, R., Hamood, H., Merhasin, I. et al. Work Transitions in Breast Cancer Survivors and Effects on Quality of Life. J Occup Rehabil 29, 336–349 (2019). https://doi.org/10.1007/s10926-018-9789-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10926-018-9789-3