Abstract
Prolonged bleeding is a general complication that occurs after tooth extraction or oral surgery. Thus, patients must apply pressure and use absorbable wound dressings to stop bleeding and prevent blood loss. This method stops bleeding and causes clotting of blood. However, some people have bleeding disorders or cannot stop bleeding with applied pressure after oral surgery. Therefore, haemostatic foam dressing is an interesting material that can be used to stop bleeding without hindering blood clotting in the wound site. In this study, foam was prepared using a blend of starch with carboxymethyl chitosan and glyoxal as a crosslinking agent. The foam was formed by freeze-drying. Carboxymethyl chitosan/starch foam absorbed water rapidly and held it, as analysed by a blood clotting assay and maximum swelling. Thus, carboxymethyl chitosan/starch foam (CM/starch foam) made with a 1:4 ratio and with 1% glyoxal also absorbed blood very well and exhibited suitable properties. Cytotoxic studies using human dermal fibroblast cells, as determined by MTT assay, confirmed that CM/starch foam was non-toxic and had good mechanical properties in a wet environment.









Similar content being viewed by others
References
Naalla R, Bhushan S, Ul Abedin M, Bichpuriya A, Singhal M (2020) Closed incisional negative pressure wound therapy at flap suture line: an innovative approach for improving outcomes in suboptimal wound conditions. ciNPWT 53:90–96
Larjava H (2012) Oral wound healing: cell biology and clinical management. Wiley, New York
Hsu S-H, Hung K-C, Chen C-W (2016) Biodegradable polymer scaffolds. J Mater Chem B 4:7493–7505
Liu J, Li Y, Hu Y, Cheng G, Ye E, Shen C, Xu F (2018) Hemostatic porous sponges of cross-linked hyaluronic acid/cationized dextran by one self-foaming process. Mater Sci Eng C 83:160–168
Anisha BS, Sankar D, Mohandas A, Chennazhi KP, Nair SV, Jayakumar R (2013) Chitosan–hyaluronan/nano chondroitin sulfate ternary composite sponges for medical use. Carbohydr Polym 92:1470–1476
Aderibigbe BA (2021) Chapter 6-Efficacy of polymer-based wound dressings in chronic wounds modeling and control of drug delivery systems. Academic Press, London, pp 79–110
Shivakumar P, Gupta MS, Jayakumar R, Gowda DV (2021) Prospection of chitosan and its derivatives in wound healing: Proof of patent analysis (2010–2020. Int J Biol 184:701–712
Wang Y, Liu G, Wu L, Qu H, Song D, Huang H, Wu C, Xu M (2020) Rational design of porous starch/hyaluronic acid composites for hemostasis. Int J Biol 158:1319–1329
Tan HW, Abdul Aziz AR, Aroua MK (2013) Glycerol production and its applications as a raw material: a review. Renew Sustain Energy Rev 27:118–127
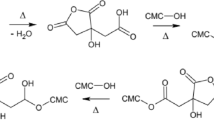
Uslu M-K, Polat S (2012) Effects of glyoxal cross-linking on baked starch foam. Carbohydr Polym 87:1994–1999
Igberase E, Osifo PO (2019) Application of diethylenetriamine grafted on glyoxal cross-linked chitosan composite for the effective removal of metal ions in batch system. Int J Biol 134:1145–1155
Singh B, Kumar A (2021) Rohit, Gamma radiation formation of sterculia gum-alginate-carbopol hydrogel dressing by grafting method for use in brain drug delivery. Chem Phys Lett 779:138875
Leonés LP, Lieblich M, Benavente R, Fiori S (2020) In vitro degradation of plasticized PLA electrospun fiber mats: morphological, thermal and crystalline evolution. Polymers 12:2–18
Moeini A, Pedram P, Makvandi P, Malinconico M, Ayala G (2020) Wound healing and antimicrobial effect of active secondary metabolites in chitosan-based wound dressings: a review. Carbohydr Polym 233, 115839
Castro-Cesena AB, Camacho-Villegas TA, Lugo-Fabres PH, Novitskaya EE, McKittrick J, Licea-Navarro A (2016) Effect of starch on the mechanical and in vitro properties of collagen-hydroxyapatite sponges for applications in dentistry. Carbohydr Polym 148:78–85
Li W, Zhou J, Xu Y (2015) Study of the in vitro cytotoxicity testing of medical devices (Review). Biomed Rep 3:617–620
Garcia SN, Gutierrez L, McNulty A (2013) Real-time cellular analysis as a novel approach for in vitro cytotoxicity testing of medical device extracts. J Biomed Mater Res A 101A(7):2097–2106
Boutrand J (2019) Biocompatibility and performance of medical devices. Woodhead Publishing, Sawston, pp 1–586
Chen W, Li X, Zeng L, Pan H, Liu Z (2021) Allicin-loaded chitosan/polyvinyl alcohol scaffolds as a potential wound dressing material to treat diabetic wounds: an in vitro and in vivo study. J. Drug Deliv. Sci. Technol. 65:102734
Kaczmarek-Szczepanska B, Miłek O, Michalska-Sionkowska M, Osyczka AM (2021) Bio-studies of scaffolds based on chitosan/tannic acid cross-linked by glyoxal. Mater Lett 292:129667
Raza M, Lim Y, Lee S, Seralathan K, Park S (2021) Synthesis and characterization of hydrogels based on carboxymethyl chitosan and poly(vinylpyrrolidone) blends prepared by electron beam irradiation having anticancer efficacy, and applications as drug carrier for controlled release of drug. Carbohydr Polym 258:117718
Naureen B, Haseeb ASMA, Basirun WJ, Muhamad F (2021) Synthesis and degradation of 3D biodegradable polyurethane foam scaffolds based on poly (propylene fumarate) and poly [(R)-3-hydroxybutyrate]. Mater. Today Commun. 28:102536
Singha G, Nayal A, Malhotra S, Koul V (2020) Dual functionalized chitosan based composite hydrogel for haemostatic efficacy and adhesive property. Carbohydr Polym 247:116757
Tai N, Ghasemlou M, Adhikari R, Adhikari B (2021) Starch-based isocyanate- and non-isocyanate polyurethane hybrids: A review on synthesis, performance and biodegradation. Carbohydr Polym 265:118029
Chen Y, Qian J, Zhao C, Yang L, Ding J, Guo H (2019) Preparation and evaluation of porous starch/chitosan composite crosslinking. Hemostatic Eur Polym J 118:17–26
Zhang Y, Chang Z, Luo W, Gu S, Li W (2015) An J. Effect of starch particles on foam stability and dilational viscoelasticity of aqueous-foam. Chin J Chem Eng 23:276–280
Li X, Wu J, Li D, Zou Q, Man Y, Zou L, Li W (2021) Pro-osteogenesis and in vivo tracking investigation of a dental implantation system comprising novel mTi implant and HYH-Fe particles. Bioact Mater 6:2658–2666
Ouyang Q, Hou T, Li C, Hu Z, Liang L, Li S, Zhong Q, Li P (2019) Construction of a composite sponge containing tilapia peptides and chitosan with improved hemostatic performance. J Int J Biol 139:719–729
Mani M, Ebenezer V, Balakrishnan R (2014) Impact of hemostatic agents in oral surgery. BJR Suppl 7:215–219
Chen K, Tong C, Yang J, Cong P, Liu Y, Shi X, Liu X, Zhang J, Zou R, Xiao K, Ni Y, Xu L, Hou M, Jin H, Liu Y (2021) Injectable melatonin-loaded carboxymethyl chitosan (CMCS)-based hydrogel accelerates wound healing by reducing inflammation and promoting angiogenesis and collagen deposition. J Mater Sci Technol 63:236–245
Li H, Cheng F, Wei X, Yi X, Tang S, Wang Z, Zhang Y, He J, Huang Y (2021) Injectable, self-healing, antibacterial, and hemostatic N,O-carboxymethyl chitosan/oxidized chondroitin sulfate composite hydrogel for wound dressing. Mater Sci Eng C 118:111324
Acknowledgements
The authors acknowledge financial support received from the Research Pyramid, Rachadaphiseksomphot Endowment Fund (GCURP_58_02_63_01) of Chulalongkorn University. This work was supported in part by (1) the Petroleum and Petrochemical College, Chulalongkorn University, (2) the 90th Anniversary of Chulalongkorn University Fund (Rachadaphiseksomphot Endowment Fund) (3) the Center of Excellence for Petroleum, Petrochemicals, and Advanced Materials (CE-PPAM) (4) The Royal Government of Thailand Scholarship 2562 and (5) Herbal Extracts-infused Advanced Wound Dressing Research Unit, Rachadaphiseksomphot Endowment Fund, Chulalongkorn University.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Jungprasertchai, N., Chuysinuan, P., Ekabutr, P. et al. Freeze-Dried Carboxymethyl Chitosan/Starch Foam for Use as a Haemostatic Wound Dressing. J Polym Environ 30, 1106–1117 (2022). https://doi.org/10.1007/s10924-021-02260-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10924-021-02260-w