Abstract
Blood pressure (BP) is a bio-physiological signal that can provide very useful information regarding human’s general health. High or low blood pressure or its rapid fluctuations can be associated to various diseases or conditions. Nowadays, high blood pressure is considered to be an important health risk factor and major cause of various health problems worldwide. High blood pressure may precede serious heart diseases, stroke and kidney failure. Accurate blood pressure measurement and monitoring plays fundamental role in diagnosis, prevention and treatment of these diseases. Blood pressure is usually measured in the hospitals, as a part of a standard medical routine. However, there is an increasing demand for methodologies, systems as well as accurate and unobtrusive devices that will permit continuous blood pressure measurement and monitoring for a wide variety of patients, allowing them to perform their daily activities without any disturbance. Technological advancements in the last decade have created opportunities for using various devices as a part of ambient assisted living for improving quality of life for people in their natural environment. The main goal of this paper is to provide a comprehensive review of various methodologies for continuous cuff-less blood pressure measurement, as well as to evidence recently developed devices and systems for continuous blood pressure measurement that can be used in ambient assisted living applications.






Similar content being viewed by others
References
Klabunde, R. (2011). Cardiovascular physiology concepts. Lippincott Williams & Wilkins.
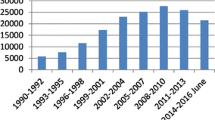
Centers for Disease Control and Prevention (CDC), Vital signs: prevalence, treatment, and control of hypertension--United States, 1999-2002 and 2005-2008. MMWR. Morb. Mortal. Wkly Rep. 60(4):103, 2011.
Mitchell, G. F., Arterial stiffness and hypertension. Hypertension 64(1):13–18, 2014.
Rosendorff, C., Lackland, D. T., Allison, M., Aronow, W. S., Black, H. R., Blumenthal, R. S. et al., Treatment of hypertension in patients with coronary artery disease: a scientific statement from the American Heart Association, American College of Cardiology, and American Society of Hypertension. J. Am. Coll. Cardiol. 65(18):1998–2038, 2015.
World Health Organization (2013), A global brief on Hypertension, WHO/DCO/WHD/2013.2 http://www.who.int/cardiovascular_diseases/publications/global_brief_hypertension/en/ Retrieved: August 2018.
Sawicka, K., Szczyrek, M., Jastrzebska, I., Prasal, M., Zwolak, A., and Daniluk, J., Hypertension–The silent killer. Journal of Pre-Clinical and Clinical Research, 5(2), 2011.
Marino, P. L., and Sutin, K. M., The ICU book (Vol. 2). Baltimore: Williams & Wilkins, 1998.
Chung, E., Chen, G., Alexander, B., and Cannesson, M., Non-invasive continuous blood pressure monitoring: a review of current applications. Frontiers of Medicine 7(1):91–101, 2013.
Mauck, G. W., Smith, C. R., Geddes, L. A., and Bourland, J. D., The meaning of the point of maximum oscillations in cuff pressure in the indirect measurement of blood pressure—part ii. J. Biomech. Eng. 102(1):28–33, 1980.
Ma, H. T., A blood pressure monitoring method for stroke management. BioMed Research International, 2014.
Drzewiecki, G. M., Melbin, J., and Noordergraaf, A., Arterial tonometry: review and analysis. J. Biomech. 16(2):141–152, 1983.
Peňáz, J., Photoelectric measurement of blood pressure, volume and flow in the finger'In: Digest of the 10th International Conference on Medical and Biological Engineering. Dresden, 104, 1973.
Koceska, N., Koceski, S., Sazdovski, V., and Ciambrone, D., Robotic Assistant for Elderly Care: Development and Evaluation. Int. J. Autom. Technol. 11(3):425–432, 2017.
Chandrasekaran, V., Dantu, R., Jonnada, S., Thiyagaraja, S., and Subbu, K. P., Cuffless Differential Blood Pressure Estimation Using Smart Phones. IEEE Trans. Biomed. Eng. 60(4):1080–1089, 2013.
McAdams, E., Krupaviciute, A., Gehin, C., Dittmar, A., Delhomme, G., Rubel, P., … & McLaughlin, J., Wearable electronic systems: Applications to medical diagnostics/monitoring. In Wearable monitoring systems (pp. 179–203). Boston: Springer, 2011.
Fayn, J., and Rubel, P., Toward a personal health society in cardiology. IEEE Trans. Inf. Technol. Biomed. 14(2):401–409, 2010.
McAdams, E., Nugent, C. D., McLaughlin, J. et al., Biomedical sensors for ambient assisted living. In: Chandra Mukhopadhyay, S., Lay-Ekuakille, A. (Eds), Advances in Biomedical Sensing Measurements, Instrumentation and Systems (pp 240–262). Berlin: Springer, Heidelberg, 2010.
Ahmad, S., Chen, S., Soueidan, K., Batkin, I., Bolic, M., Dajani, H., and Groza, V., Electrocardiogram-assisted blood pressure estimation. IEEE Trans. Biomed. Eng. 59(3):608–618, 2012.
McAdams, E. T., Gehin, C., Noury, N., Ramon, C., Nocua, R., Massot, B., … and McLaughlin, J., Biomedical sensors for ambient assisted living. In Advances in Biomedical Sensing, Measurements, Instrumentation and Systems (pp. 240–262). Berlin: Springer, 2010.
Thomas, S. S., Nathan, V., Zong, C., Akinbola, E., Aroul, A. L. P., Philipose, L., … and Jafari, R. , BioWatch—A wrist watch based signal acquisition system for physiological signals including blood pressure. In Engineering in Medicine and Biology Society (EMBC), 2014 36th Annual International Conference of the IEEE (pp. 2286–2289). IEEE, 2014.
Baek, H. J., Lee, H. B., Kim, J. S., Choi, J. M., Kim, K. K., and Park, K. S., Nonintrusive biological signal monitoring in a car to evaluate a driver’s stress and health state. Telemedicine and e-Health 15(2):182–189, 2009.
Gu, W. B., Poon, C. C. Y., Leung, H. K., Sy, M. Y., Wong, M. Y. M., and Zhang, Y. T., A novel method for the contactless and continuous measurement of arterial blood pressure on a sleeping bed. In Engineering in Medicine and Biology Society, 2009. EMBC 2009. Annual International Conference of the IEEE (pp. 6084–6086). IEEE, 2009.
Kim, J., Park, J., Kim, K., Chee, Y., Lim, Y., and Park, K., Development of a nonintrusive blood pressure estimation system for computer users. Telemedicine and e-Health 13(1):57–64, 2007.
Wu, C. M., Chuang, C. Y., Chen, Y. J., and Chen, S. C., A new estimate technology of non-invasive continuous blood pressure measurement based on electrocardiograph. Advances in Mechanical Engineering 8(6):1687814016653689, 2016.
Parák, J., and Havlík, J., ECG signal processing and heart rate frequency detection methods. Proceedings of Technical Computing Prague. 8, 2011.
Ubeyli, E. D., Feature extraction for analysis of ECG signals. In Engineering in Medicine and Biology Society, 2008. EMBS 2008. 30th Annual International Conference of the IEEE (pp. 1080–1083). IEEE, 2008.
AlMahamdy, M., and Riley, H. B., Performance study of different denoising methods for ECG signals. Procedia Computer Science 37:325–332, 2014.
Diab, M.K., Masimo Corp., Plethysmograph pulse recognition processor. U.S. Patent 7,044,918, 2006.
Pilt, K., Ferenets, R., Meigas, K., Lindberg, L. G., Temitski, K., and Viigimaa, M., New photoplethysmographic signal analysis algorithm for arterial stiffness estimation. The Scientific World Journal, 2013.
Elgendi, M., Norton, I., Brearley, M., Abbott, D., and Schuurmans, D., Detection of a and b waves in the acceleration photoplethysmogram. Biomed. Eng. Online 13(1):139, 2014.
Bagha, S., and Shaw, L., A Real Time Analysis of PPG Signal for Measurement of SpO2 and Pulse Rate. Int. J. Comput. Appl. 36(11):45–50, 2011.
Joseph, G., Joseph, A., Titus, G., Thomas, R. M., and Jose, D., Photoplethysmogram (PPG) signal analysis and wavelet de-noising. In Emerging Research Areas: Magnetics, Machines and Drives (AICERA/iCMMD), 2014 Annual International Conference on (pp. 1–5). IEEE, 2014.
Sharma, M., Barbosa, K., Ho, V., Griggs, D., Ghirmai, T., Krishnan, S. K., Hsiai, T. K., Chiao, J. C., and Cao, H., Cuff-Less and Continuous Blood Pressure Monitoring. A Methodological Review Technologies 5(2):21, 2017.
Goli, S., and Jayanthi, T., Cuff less continuous non-invasive blood pressure measurement using pulse transit time measurement. Int J Recent Dev Eng Technol 2:86–91, 2014.
Poon, C. C. Y., and Zhang, Y. T., Cuff-less and noninvasive measurements of arterial blood pressure by pulse transit time. In Engineering in Medicine and Biology Society, 2005. IEEE-EMBS 2005. 27th Annual International Conference of the (pp. 5877–5880). IEEE, 2006.
He, X., Goubran, R. A., and Liu, X. P., Evaluation of the correlation between blood pressure and pulse transit time. In Medical Measurements and Applications Proceedings (MeMeA), 2013 IEEE International Symposium on (pp. 17–20). IEEE, 2013.
Gao, M., Olivier, N. B., and Mukkamala, R., Comparison of noninvasive pulse transit time estimates as markers of blood pressure using invasive pulse transit time measurements as a reference. Phys. Rep. 4(10):e12768, 2016.
Chen, Y., Wen, C., Tao, G., and Bi, M., Continuous and noninvasive measurement of systolic and diastolic blood pressure by one mathematical model with the same model parameters and two separate pulse wave velocities. Ann. Biomed. Eng. 40(4):871–882, 2012.
Li, P., Liu, M., Zhang, X., Hu, X., Pang, B., Yao, Z., and Chen, H., Novel wavelet neural network algorithm for continuous and noninvasive dynamic estimation of blood pressure from photoplethysmography. SCIENCE CHINA Inf. Sci. 59(4):042405, 2016.
Zhang, Q., Zhou, D., and Zeng, X., Highly wearable cuff-less blood pressure and heart rate monitoring with single-arm electrocardiogram and photoplethysmogram signals. Biomed. Eng. Online 16(1):23, 2017.
Mukkamala, R., Hahn, J. O., Inan, O. T., Mestha, L. K., Kim, C. S., Toreyin, H., and Kyal, S., Toward ubiquitous blood pressure monitoring via pulse transit time: theory and practice. IEEE Trans Biomed Engineering 62(8):1879–1901, 2015.
Buxi, D., Redouté, J. M., and Yuce, M. R., A survey on signals and systems in ambulatory blood pressure monitoring using pulse transit time. Physiol. Meas. 36(3):R1, 2015.
Cattivelli, F. S., and Garudadri, H., Noninvasive cuffless estimation of blood pressure from pulse arrival time and heart rate with adaptive calibration. In Wearable and Implantable Body Sensor Networks, 2009. BSN 2009. Sixth International Workshop on (pp. 114–119). IEEE, 2009.
Mottaghi, S., Moradi, M. H., and Roohisefat, L., Cuffless blood pressure estimation during exercise stress test. International Journal of Bioscience, Biochemistry and Bioinformatics 2(6):394, 2012.
Payne, R. A., Symeonides, C. N., Webb, D. J., and Maxwell, S. R. J., Pulse transit time measured from the ECG: an unreliable marker of beat-to-beat blood pressure. J. Appl. Physiol. 100(1):136–141, 2006.
Mazaheri, S., and Zahedi, E., A comparative review of blood pressure measurement methods using pulse wave velocity. In Smart Instrumentation, Measurement and Applications (ICSIMA), 2014 IEEE International Conference on (pp. 1–5). IEEE, 2014.
Pereira T, Sanches R, Reis P, Pego J, and Simoes R., Correlation study between blood pressure and pulse transit time. In: IEEE 4th Portuguese Meeting on bioengineering (ENBENG). p. 1–5, 2015.
Ye, S. Y., Kim, G. R., Jung, D. K., Baik, S. W., and Jeon, G. R., Estimation of systolic and diastolic pressure using the pulse transit time. World Academy of Science. Eng. Technol. 67:726–731, 2010.
Ghosh, S., Banerjee, A., Ray, N., Wood, P. W., Boulanger, P., and Padwal, R., Continuous blood pressure prediction from pulse transit time using ECG and PPG signals. In Healthcare Innovation Point-Of-Care Technologies Conference (HI-POCT), 2016 IEEE (pp. 188–191). IEEE, 2016.
Wibmer, T., Doering, K., Kropf-Sanchen, C., Rüdiger, S., Blanta, I., Stoiber, K. M., … & Schumann, C., Pulse transit time and blood pressure during cardiopulmonary exercise tests. Physiological Research, 63(3), 2014.
Esmaili, A., Kachuee, M., and Shabany, M., Nonlinear Cuffless Blood Pressure Estimation of Healthy Subjects Using Pulse Transit Time and Arrival Time. IEEE Trans. Instrum. Meas. 66(12):3299–3308, 2017.
Lin, H., Xu, W., Guan, N., Ji, D., Wei, Y., and Yi, W., Noninvasive and continuous blood pressure monitoring using wearable body sensor networks. IEEE Intell. Syst. 6:38–48, 2015.
Puke, S., Suzuki, T., Nakayama, K., Tanaka, H., & Minami, S., Blood pressure estimation from pulse wave velocity measured on the chest. In Engineering in Medicine and Biology Society (EMBC), 2013 35th Annual International Conference of the IEEE (pp. 6107–6110). IEEE, 2013.
Jain, M., Kumar, N., & Deb, S., An affordable cuff-less blood pressure estimation solution. In Engineering in Medicine and Biology Society (EMBC), 2016 IEEE 38th Annual International Conference of the (pp. 5294–5297). IEEE, 2016.
Kachuee, M., Mahdi Kiani, M., Mohammadzade, H., and Shabany, M., Cuffless Blood Pressure Estimation Algorithms for Continuous Health-Care Monitoring. IEEE Trans. Biomed. Eng. 64(4):859–869, 2017.
Kumar N, Agrawal A, and Deb, S., Cuffless BP measurement using a correlation study of pulse transient time and heart rate. In Int. Conf. Adv. Comp. Info. (ICACCI). IEEE, pp. 1538–1541, 2014.
Lameski, P., Zdravevski, E., Koceski, S., Kulakov, A., and Trajkovik, V., Suppression of Intensive Care Unit False Alarms Based on the Arterial Blood Pressure Signal. IEEE Access 5:5829–5836, 2017.
Ding, X., Yan, B. P., Zhang, Y. T., Liu, J., Zhao, N., and Tsang, H. K., Pulse transit time based continuous cuffless blood pressure estimation: A new extension and a comprehensive evaluation. Sci. Rep. 7(1):11554, 2017.
Heravi, Y., Amin, M., Keivan, V., and Sima, J., A New Approach for Blood Pressure Monitoring based on ECG and PPG Signals by using Artificial Neural Networks. Int. J. Comput. Appl. 103(12):36–40, 2014.
He, R., Huang, Z. P., Ji, L. Y., Wu, J. K., Li, H., and Zhang, Z. Q., Beat-to-beat ambulatory blood pressure estimation based on random forest. In Wearable and Implantable Body Sensor Networks (BSN), 2016 IEEE 13th International Conference on (pp. 194–198). IEEE, 2016.
Peter, L., Noury, N., and Cernya, M., A review of methods for non-invasive and continuous blood pressure monitoring: Pulse transit time method is promising? IRBM 35(5):271–282, 2014.
Muehlsteff J, Aubert X and Schuett M., Cuffless estimation of systolic blood pressure for short effort bicycle tests: the prominent role of the pre-ejection period in 2006 Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC'06), New York, pp. 5088–5092, IEEE, 2010.
Gesche, H., Grosskurth, D., Küchler, G., and Patzak, A., Continuous blood pressure measurement by using the pulse transit time: comparison to a cuff-based method. Eur. J. Appl. Physiol. 112(1):309–315, 2012.
Tabatabai, D., Cuff-less and calibration free blood pressure estimation using the pulse transit time method, ECE 699–002, Learning from Data Project, 2015.
Kachuee, M., Kiani, M. M., Mohammadzade, H., and Shabany, M., Cuff-less high-accuracy calibration-free blood pressure estimation using pulse transit time. In Circuits and Systems (ISCAS), 2015 IEEE International Symposium on (pp. 1006–1009). IEEE, 2015.
Jain, M., Kumar, N., Deb, S., and Majumdar, A., A sparse regression based approach for cuff-less blood pressure measurement. In Acoustics, Speech and Signal Processing (ICASSP), 2016 IEEE International Conference on (pp. 789–793). IEEE, 2016.
Wang, R., Jia, W., Mao, Z. H., Sclabassi, R. J., and Sun, M., Cuff-free blood pressure estimation using pulse transit time and heart rate, Int Conf Signal Process Proc. pp:115–118, 2014.
Chen, Y., Wen, C., Tao, G., Bi, M., and Li, G., Continuous and noninvasive blood pressure measurement: a novel modeling methodology of the relationship between blood pressure and pulse wave velocity. Ann. Biomed. Eng. 37(11):2222–2233, 2009.
Zheng, D., and Murray, A., Non-invasive quantification of peripheral arterial volume distensibility and its non-linear relationship with arterial pressure. J. Biomech. 42:1032–1037, 2009.
Arza, A., Lázaro, J., Gil, E., Laguna, P., Aguiló, J., and Bailon, R., Pulse transit time and pulse width as potential measure for estimating beat-to-beat systolic and diastolic blood pressure. In Computing in Cardiology Conference (CinC), 2013 (pp. 887–890). IEEE, 2013.
Sun, S., Bezemer, R., Long, X., Muehlsteff, X., and Aarts, R. M., Systolic blood pressure estimation using PPG and ECG during physical exercise, Physiol Meas, pp. 2154–2169, 2016.
Muehlsteff, J., Aubert, X. A., and Morren, G., Continuous cuff-less blood pressure monitoring based on the pulse arrival time approach: The impact of posture. In: Engineering in Medicine and Biology Society, 2008. EMBS 2008. 30th Annual International Conference of the IEEE (pp. 1691–1694). IEEE, 2008.
Shaltis, P. A., Reisner, A. T., and Asada, H. H., Cuffless blood pressure monitoring using hydrostatic pressure changes. IEEE Trans. Biomed. Eng. 55(6):1775–1777, 2008.
Shaltis, P. A., Reisner, A., and Asada, H. H., Wearable, cuff-less PPG-based blood pressure monitor with novel height sensor. In Engineering in Medicine and Biology Society, 2006. EMBS'06. 28th Annual International Conference of the IEEE (pp. 908–911), 2006.
Pielmuş, A. G., Pflugradt, M., Tigges, T., Klum, M., Feldheiser, A., Hunsicker, O., and Orglmeister, R., Novel computation of pulse transit time from multi-channel PPG signals by wavelet transform. Current Directions in Biomedical Engineering 2(1):209–213, 2016.
Pinheiro, E., Postolache, O., and Girão, P., Blood pressure and heart rate variabilities estimation using ballistocardiography. In Proceedings of the 7th Conf. on. Telecom (pp. 125–128), 2009.
Holz, C., and Wang, E. J., Glabella: Continuously sensing blood pressure behavior using an unobtrusive wearable device. Proceedings of the ACM on Interactive, Mobile, Wearable and Ubiquitous Technologies 1(3):58, 2017.
Ananth, S., and Sharath, S., Project milestone report for CS229: Blood Pressure detection from PPG, https://www.semanticscholar.org/paper/Project-milestone-report-for-CS229-Blood-Pressure-Ananth-Sharath/d85bc5b45f0c9c7099fdd5a0b9c4eb1a7cdb4afd Retrieved: August 2018, 2014.
Ruiz-Rodríguez, J. C., Ruiz-Sanmartín, A., Ribas, V., Caballero, J., García-Roche, A., Riera, J. et al., Innovative continuous non-invasive cuffless blood pressure monitoring based on photoplethysmography technology. Intensive Care Med. 39(9):1618–1625, 2013.
Kurylyak, Y., Lamonaca, F., and Grimaldi, D., A neural network-based method for continuous blood pressure estimation from a PPG signal, Instrumentation and Measurement Technology Conference (I2MTC), 2013 IEEE International. IEEE 2013:280–283, 2013.
He, X., Goubran, R. A., and Liu, X. P., Secondary Peak Detection of PPG Signal for Continuous Cuffless Arterial Blood Pressure Measurement. IEEE Trans. Instrum. Meas. 63(6):1431–1439, 2014.
Liu, M., Po, L. M., and Fu, H., Cuffless Blood Pressure Estimation Based on Photoplethysmography Signal and Its Second Derivative. International Journal of Computer Theory and Engineering 9(3):202, 2017.
Hassan, M. K. B. A., Mashor, M. Y., Nasir, N. M., and Mohamed, S., Measuring of systolic blood pressure based on heart rate. In 4th Kuala Lumpur International Conference on Biomedical Engineering 2008 (pp. 595–598). Berlin: Springer, 2008.
Nemati, E., Deen, M. J., and Mondal, T., A wireless wearable ECG sensor for long-term applications. IEEE Communications Magazine, 50(1), 2012.
Nonlinear Analysis for the ECG and Blood Pressure Signals, http://shodhganga.inflibnet.ac.in/bitstream/10603/7968/14/17_chapter7.pdf. Retrieved: August, 2018.
Monroy Estrada, G., Mendoza, L. E., and Molina, V., Relationship of blood pressure with the electrical signal of the heart using signal processing. Tecciencia 9(17):9–14, 2014.
He, X., Goubran, R. A., and Liu, X. P., Using Eulerian video magnification framework to measure pulse transit time. In Medical Measurements and Applications (MeMeA), 2014 IEEE International Symposium on (pp. 1–4). IEEE, 2014.
Al-Shaqi, R., Mourshed, M., and Rezgui, Y., Progress in ambient assisted systems for independent living by the elderly. SpringerPlus 5(1):624, 2016.
Linskell, J., Smart home technology and special needs reporting UK activity and sharing implemention experiences from Scotland. In Pervasive Computing Technologies for Healthcare (PervasiveHealth), 2011 5th International Conference on (pp. 287–291). IEEE, 2011.
Liu, H., Ivanov, K., Wang, Y., and Wang, L., Toward a smartphone application for estimation of pulse transit time. Sensors 15(10):27303–27321, 2015.
Chandrasekhar, A., Kim, C. S., Naji, M., Natarajan, K., Hahn, J. O., and Mukkamala, R., Smartphone-based blood pressure monitoring via the oscillometric finger-pressing method. Science Translational Medicine, 10(431), eaap8674, 2018.
Majumder, S., Mondal, T., and Deen, M. J., Wearable sensors for remote health monitoring. Sensors 17(1):130, 2017.
Pantelopoulos, A., and Bourbakis, N. G., A survey on wearable sensor-based systems for health monitoring and prognosis. IEEE Trans. Syst. Man Cybern. Part C Appl. Rev. 40(1):1–12, 2010.
Zhang, Q., Zeng, X., Hu, W., and Zhou, D., A machine learning-empowered system for long-term motion-tolerant wearable monitoring of blood pressure and heart rate with Ear-ECG/PPG. IEEE Access 5:10547–10561, 2017.
Shahriyar, R., Bari, M. F., Kundu, G., Ahamed, S. I., and Akbar, M. M., Intelligent mobile health monitoring system (IMHMS). In: International Conference on Electronic Healthcare (pp. 5–12). Berlin: Springer, 2009.
Wannenburg, J., and Malekian, R., Body sensor network for mobile health monitoring, a diagnosis and anticipating system. IEEE Sensors J. 15(12):6839–6852, 2015.
Wood, A. D., Stankovic, J. A., Virone, G., Selavo, L., He, Z., Cao, Q., … and Stoleru, R., Context-aware wireless sensor networks for assisted living and residential monitoring. IEEE Network, 22(4), 2008.
Espina, J., Falck, T., Muehlsteff, J., Jin, Y., Adán, M. A., and Aubert, X., Wearable body sensor network towards continuous cuff-less blood pressure monitoring. In: Medical Devices and Biosensors, 2008. ISSS-MDBS 2008. 5th International Summer School and Symposium on (pp. 28–32). IEEE, 2008.
Mouradian, V., Poghosyan, A., and Hovhannisyan, L., Noninvasive continuous mobile blood pressure monitoring using novel PPG optical sensor. In Biomedical Wireless Technologies, Networks, and Sensing Systems (BioWireleSS), 2015 IEEE Topical Conference on (pp. 1–3). IEEE, 2015.
Ilango, S., and Sridhar, P., A non-invasive blood pressure measurement using android smart phones. IOSR J Dent Med Sci 13:28–31, 2014.
Theodor, M., Fiala, J., Ruh, D., Foerster, K., Heilmann, C., Beyersdorf, F. et al., Implantable accelerometer system for the determination of blood pressure using reflected wave transit time. Sensors Actuators A Phys. 206:151–158, 2014.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Patient Facing Systems
Rights and permissions
About this article
Cite this article
Stojanova, A., Koceski, S. & Koceska, N. Continuous Blood Pressure Monitoring as a Basis for Ambient Assisted Living (AAL) – Review of Methodologies and Devices. J Med Syst 43, 24 (2019). https://doi.org/10.1007/s10916-018-1138-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10916-018-1138-8