Abstract
The new and ground-breaking real-time remote monitoring in triage and priority-based sensor technology used in telemedicine have significantly bounded and dispersed communication components. To examine these technologies and provide researchers with a clear vision of this area, we must first be aware of the utilised approaches and existing limitations in this line of research. To this end, an extensive search was conducted to find articles dealing with (a) telemedicine, (b) triage, (c) priority and (d) sensor; (e) comprehensively review related applications and establish the coherent taxonomy of these articles. ScienceDirect, IEEE Xplore and Web of Science databases were checked for articles on triage and priority-based sensor technology in telemedicine. The retrieved articles were filtered according to the type of telemedicine technology explored. A total of 150 articles were selected and classified into two categories. The first category includes reviews and surveys of triage and priority-based sensor technology in telemedicine. The second category includes articles on the three-tiered architecture of telemedicine. Tier 1 represents the users. Sensors acquire the vital signs of the users and send them to Tier 2, which is the personal gateway that uses local area network protocols or wireless body area network. Medical data are sent from Tier 2 to Tier 3, which is the healthcare provider in medical institutes. Then, the motivation for using triage and priority-based sensor technology in telemedicine, the issues related to the obstruction of its application and the development and utilisation of telemedicine are examined on the basis of the findings presented in the literature.
Similar content being viewed by others
Introduction
Since the 1970s, telemedicine has become an essential element in the utilisation of modern information and communication technologies for health services. The earliest mention of telemedicine in cardiology dates to the early twentieth century when electrocardiographic data were first transmitted over telephonic wires [1]. Telemedicine is a remote medical practice that allows coordination among different individuals and facilitates their collaboration efforts in diagnosing or treating a disease through information technologies and telecommunication [2]. Thus, this domain needs multidisciplinary advancements, particularly in the use of telecommunication, computer science and instrumentation for the exchange and administration of medical data [3]. A related concept is telehealth, which usually refers to clinical and non-clinical services, such as education, management or research [4]. Telemedicine is hardly included in legislation, yet national regulation and healthcare control affect the strategy of healthcare assistance in several countries, such as France. The French government had characterised some demonstrations of telemedicine in announcement no. 2010–1229 (19 October 2010), as follows:
-
Remote advisement: A doctor provides a remote recommendation to sick people who might be helped by health professionals.
-
Remote proficiency: A doctor remotely requests a different physician for checking and managing conditions.
-
Medicinal telemonitoring: Caregivers monitor and decode the therapeutic indications of the sick person. Such tasks can be accomplished by either hand or self-regulating mode.
-
Medicinal teleassistance: A doctor remotely helps another doctor in performing a therapeutic demonstration.
-
Medical coordination of emergency [5].
Currently, telemedicine has attracted considerable attention in research owing to the development of new technologies [2]. Telemedicine is a proficient tool that allows coordinated efforts among doctors and offers numerous benefits (e.g., enhanced care, cost investment funds, improved arrival and real-time responses). Similar to medicinal training, telemedicine is used for diagnosis; the conduct of preventive or post-curative medicinal checking and monitoring and therapeutic procedures; the prescription of medications and the provision of services [2]. Telemedicine offers empowerment and superior personal satisfaction and reduces the costs of treatments for chronic diseases, such as cardiovascular infection, diabetes, chronic respiratory malady and cancer [6]. Unfortunately, despite these benefits, telemedicine still suffers from several problems associated with the administration of learning resources, enhancement of safety construction and hazard administration in the context of persistent amelioration of healthcare aides [5]. Moreover, telemedicine application has many domains, such as disaster relief, schools and industrial health [2]. Meanwhile, increasing healthcare costs and the growing population of the elderly have spurred the development of telemedicine networks for the delivery of several healthcare services [7]. In particular, a general three-tiered ubiquitous telemedicine system based on wireless body area network (WBAN) has been used for real-time and constant healthcare monitoring. In Tier 1, users obtain their vital signs through sensors, such as electrocardiogram (ECG) for the graphic measurement of heartbeat and oxygen saturation (SpO2) for the measurement of oxygen concentration in the blood. In Tier 2, the obtained readings are transmitted to personal gateways, such as handheld apparatus, personal digital assistants (PDAs) and personal computer, all of which use local area network (LAN) protocols (Bluetooth and Zigbee) and WBAN. Medical data are the sent from Tier 2 to Tier 3 through extensive area wireless connection protocols or Internet services. Tier 3 involves healthcare providers in medical institutes (MIs) who apply a certain procedure and generate services that are sent back as responses to users. The entire process of the system is shown in Fig. 1 [4].
Three-tiered architecture of a WBAN telemedicine system for healthcare monitoring [4]
Without a telemedicine system, users (patients) go to hospitals to obtain healthcare services. The increasing number of patients poses challenges to healthcare service providers, specifically challenges related to the prioritisation of emergency cases and the limited medical resources. These problems are often addressed by triaging patients to the emergency department (ED). Triage is the system of sorting patients by order of treatment necessity during a large-scale emergency and involves the assessment and prioritisation of all patients and casualties [4]. Modern healthcare systems have the following triage stages: pre-hospital triage, in which an emergency vehicle is sent and pre-hospital resources are prepared; triage on site by the earliest available doctor managing the sick person and triage at the entrance to the hospital [8]. A primary aim of triage in the ED is to identify patients who can safely wait and those who cannot [4]. The crucial portion of triage in the ED is the monitoring of patients’ vital signs, by which the severity of their conditions are determined [9]. The ED is a place where many people have to be taken care of in a short time period and where urgent cases can emerge. As soon as a patient arrives at the ED, the medical staff present must implement the triage process to identify the severity of the patient’s condition for prioritisation. In actual practice, triage is often untimely implemented, and this situation increases the risk of critical health complications [9]. In mass-casualty incidents (MCIs), people need prompt medical care, and their health situations must be documented for additional evaluation. The number of patients often taxes the ability of healthcare practitioners to provide medical care competently. Healthcare practitioners generally design triage such that patients are treated according to the severity of their conditions. Constant monitoring of vital signs is essential to the assessment of a patient’s clinical situation, and effective triage and actual-time estimation are essential to conditions in which many patients need medical care, particularly during a catastrophe or disaster scenarios, or to conditions in which healthcare resources are limited. The assessment of vital signs aids the estimation of the general physical well-being of patients, and the actual monitoring of the vital signs affects the prioritisation of medical help in emergency conditions [10]. Vital signs are important in triage and prioritisation setting because they provide a thematic complement to nurses’ experienced judgment and optimise inter-rater consistency [4]. Meanwhile, on the basis of the recent progress in autonomous sensor technology, a new class of intelligent network, called WBAN, has been developed [11]. Sensors in a telemedicine system (Fig. 1) enable real-time healthcare monitoring and are affixed to or inserted into the human body for the observation of vital signs through WBAN. That is, the system ensures the constant and reliable monitoring of extreme defects and conditions in a human body; thus, it is preferred both by sick and healthy people [12]. Healthcare implementations dependent on sensors are increasingly gaining popularity in the medical field. In WBANs, sensing data are collected from a group of knots on a patient’s body and transmitted to a main server [13]. Meanwhile, sensors for wellness monitoring have been used for a long time in healthcare networks. Whether these signal-anticipating instruments are used for the diagnosis and prevention of diseases or situations in which patients are immobile, they have a vital role in new healthcare services [14]. In this study, we review the achievements of several studies on modern technology, systematise the studies of smartphone malware from the literature into a coherent taxonomy, determine the various characteristics that differentiate this developing field and show the distribution of these articles with reference to database type, country of production, smartphone operating system and year of publication. The benefits of the targeted goals are elaborated. Moreover, issues and concerns are presented to identify the gaps in the literature. Recommendations for different directions are presented to assist researchers, providers and end users with regard to smartphone malware.
Method
The scope of this study is covered by the most important keywords, namely, ‘telemedicine’, ‘triage’, ‘priority’ and ‘sensor’. Our study is limited to English-language studies. The following digital databases were selected to search for target papers: (1) ScienceDirect, which provides access to papers and articles on science and technology in highly reliable journals; (2) the IEEE Xplore digital database of scholarly and technical literature, which provides the abstracts and complete texts of papers on computer science, electrical engineering and electronics and (3) the Web of Science (WoS) database, which provides cross-disciplinary research on social science, science, technologies, humanities and the arts. These databases cover scientific and technical literature and provide extensive insights into researchers’ efforts in a wide yet relevant area of disciplines. Studies were selected by searching literature sources, then screening and filtering were performed in three iterations. In the first iteration, duplicate articles were excluded, and only articles published in the past six years (2012–2017) were collected using the Mendeley software. In the second iteration, the articles were filtered according to their titles and abstracts, and articles outside of the scope of our domain were excluded. In the third iteration, the articles were filtered by reading the full text and excluding articles outside of the scope of our domain and which do not meet our criteria, as shown in Fig. 2. The same eligibility criteria were applied in all three iterations by three authors who performed the screening and were reviewed by four other authors. The search was conducted on the ScienceDirect, IEEE Xplore and WoS databases in January 2017. A mix of keywords in different forms were used, such as ‘medical system’, ‘telemonitoring’, ‘e-health’, ‘telemedicine’, ‘telehealth’, ‘healthcare services’, ‘remote monitoring’ and ‘mobile doctor’, combined with the ‘OR’ and ‘AND’ operators followed by ‘triage’ and ‘priority’ or combined with the ‘OR’ and ‘AND’ operators followed by ‘sensor’. The explicit query text is shown at the top of Fig. 2. We used other additional options in the search engines of the three databases to ignore the chapters of books and reports. We excluded journals and conference articles because we considered these two venues to be the most likely to include up-to-date and appropriate scientific works pertinent to our survey.
Eligibility criteria
The articles that satisfied our criteria shown in Fig. 2 were included in our work. The initial target was to map the research scope into a general and coarse-grained taxonomy that consists of two categories derived from a previous study of the literature with no restrictions (we used Google Scholar to learn the directions in the literature). After removing duplicate papers between databases, we excluded the articles through three iterations of filtering and screening when the articles did not meet our eligibility criteria. Articles were excluded if (1) they are not written in English, (2) they focus on a particular aspect of telemedicine technology and (3) their target is general telemedicine technology. Our work focuses on healthcare services, patient prioritisation, patient triage, disaster management, network failure, sensors in telemedicine and security of telemedicine.
Data collection process
For the simplification of the filtering process, all included articles were read, analysed and summarised according to their initial categories and saved as Microsoft Word and Excel files. The authors performed full-text reading on all articles. Numerous highlights and notes on the surveyed works and a running classification of all the articles enabled us to create the proposed taxonomy. The comments were recorded as hard or soft copy versions according to each author’s style. This process was followed by another process of characterisation, description, tabulation and conclusion of the essential findings. These findings are provided in the supplementary materials as a complete reference for the results that will be described in the subsequent section.
Result
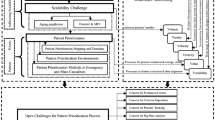
The results of the initial query search of 3064 articles are as follows: 911 articles from ScienceDirect, 1496 articles from IEEE Xplore and 657 articles from WoS from 2007 to 2017. We were unable to download two scientific articles from WoS because of accessibility issues. The articles were filtered according to the sequence that was adopted in this research and using two categories: 1612 papers were published in the past six years (from 2012 to 2017) and 65 papers appeared in all three databases, thereby resulting in 1547 papers. After a full scan of the titles and abstracts of the papers, 1264 more papers were excluded. Then, 133 papers were excluded after the final full-text reading. The final set consisted of 150 papers, which were divided into two major categories. The first category, which contained 31 articles (20.66%), was survey and review, in which researchers described and provided a general overview of triage and priority-based sensor technology in telemedicine. The second category was three-tiered telemedicine architecture. Tier 1 represented the users who obtained their vital signs through sensors and sent them to a personal gateway or Tier 2 through LAN protocols and WBAN. Medical data were sent from Tier 2 to Tier 3, which was the healthcare provider in MIs. This category contained 119 articles (79.33%) and had three sections. The first section, containing 44 out of 119 articles, was the sensor-based gateway (Tier 1) and described and summarised the issues and sensor technologies in telemedicine, which provided continuous and reliable healthcare monitoring. The articles in this section were divided into six subsections: (1) energy efficiency (11/44 articles), (2) evaluation-and-assessment-based sensors (4/44 articles), (3) ontology-based sensors (1/44 articles), (4) quality of service (QoS) (5/44 articles), (5) security-and-privacy-based sensors (5/44 articles) and (6) reliability (18/44 articles). Reliability comprised four subsections: congestion control (5/18 articles), electromagnetic interference (EMI; 2/18 articles), false alarm detection (1/18 articles) and link quality and packet transmission delay (10/18 articles). The second section was mobile health (mHealth) and gateway and included 32 articles. In this section, the tasks, fields and several areas of mHealth and gateway technology were described and summarised. Gateway technology was considered responsible for aggregating and analysing data collected from all monitoring devices equipped with sensors and for transmitting these data to a server on the basis of the telemedicine architecture. This section had eight subsections, namely, ambient assisted living (AAL) (4/32 articles), integration and aggregation (5/32 articles), disaster management (6/32 articles), treatment support and disease surveillance (9/32 articles), evaluation-and-assessment-based mHealth and gateway (1/32 articles), mobile user interface (MUI) adaptation (1/32 articles), network management (4/32 articles) and decision support system (DSS) (2/32 articles). The third section was server based, with 43 out of 119 articles. In this section, the server-based aspect (Tier 3) were described and summarised and healthcare provider in medical centres or MIs through wireless wide area network or Internet services were considered. The healthcare providers on the server side support the monitoring of patients and apply certain processes to generate services to patients as responses, as shown in Fig. 3. This tier also provides support to professionals and manages the environment. This section had six subsections as follows: (1) analysis process (2/43 articles); (2) environmental management (3/43 articles); (3) evaluation-and-assessment-based server (3/43 articles); (4) security-and-privacy-based server (2/43 articles); (5) collaboration fields (7/43 articles), which is further divided into cooperative environment (2/7 articles) and tele-expertise between professionals (5/7 articles); and (6) remote monitoring (26/43 articles), which is further divided into three subsections: patient prioritisation (2/26 articles), patient triage (8/26 articles) and providing services to the patient (16/26 articles). We observed these patterns, rounded up the general categories of articles and refined the classification into literature taxonomy, as shown in Fig. 3. Several subcategories were identified in the main classes, although overlaps emerged. The subsequent sections describe the observed categories, and simple concomitant statistics are provided in the figures.
Reviews and surveys
The primary aim of review and survey articles on telemedicine is to understand current thinking in this field and justify the need for future research on related topics that have been overlooked or understudied. Of the 150 selected articles, 31 were review and survey articles (20.66%). A survey of the framework was conducted in [15] for the classification of different types of emergency and non-emergency healthcare facilities with regard to location management. A review of robots in home healthcare, where sociotechnical factors are critical in explaining the adoption intention of home healthcare robots, was presented in [16]. A systematic review of mixed-methods research using the PRISMA methodology on human factors and ergonomics in healthcare was presented in [17]. A survey on e-health, research projects and comparative studies that introduced the standard components of telemonitoring systems for the exploration of telemonitoring architecture and its main issues was conducted in [3]. In [18], a systematic review of digital health innovation ecosystems was performed for the exploration of digital health, innovation and digital ecosystems and for the creation of a conceptual framework. A study on national domain and quality was conducted and provided an overview of the US population health, access to care, status of healthcare quality and disparities in care experienced by different socioeconomic, racial and ethnic groups [19]. Of the 31 studies, 13 reviewed the most important implementations of techniques and methods for telemedicine applications and mobile technologies and considered the integration of mobile technologies in the diagnosis and treatment of various diseases, such as heart failure, acute cardiac disease and acute stroke, and in cardiac rehabilitation services. Many reviews emphasised the home blood glucose testing market, that is, diabetes and glucose sensing, and focused on an automatic early stress recognition system and mHealth technology for military mental health, diagnoses and treatment of disorders to improve the quality of care [1, 6, 20,21,22,23,24,25,26,27,28,29,30]. Other reviews (5/31 articles) covered various topics and specifically focused on mHealth services and applications. A review of emerging technologies in emergency medical services (EMS) that highlighted studies and resources supported by the EMS for children was presented in [31]. A survey of mHealth solutions in Brazil provided insights into how the initiatives of mHealth are beginning to be used and developed in emerging countries [32]. Related works identified the need for mHealth in China and presented major mHealth products and technologies in this country [33]. A comprehensive review and a thorough analysis of novel mHealth services and applications proposed were conducted for the survey and review of state-of-the-art mHealth services and applications [34]. In [35], a review of the tools of mHealth was conducted to provide a new research scope for compatible biomarkers in concert with different types of data (e.g. global positioning and self-report system data). Other works (3/31 articles) focused on the aging population from different aspects, and a systematic review was conducted to evaluate the maturity of technology among elderly people and provide evidence for home healthcare monitoring technologies and smart homes [36]. The strategies and effective measures for the promotion of information and communications technology (ICT)-enabled innovations in Japan were investigated [37]. A review of the aging population (TigerPlace) in Missouri-sponsored population aging facilities and the development of sensor technologies was presented in [38]. Other works (2/31 articles) focused on the sensing technologies and WBAN applications in telemedicine classification and the suitability requirements of sensor technology for activity recognition [7, 39]. Out of 31 articles in this category, 2 reviewed home-based consumer and healthcare technologies for smart homes and research opportunities in the era of wellness medicine [40, 41].
Telemedicine architecture
The second category is telemedicine architecture, which consists of three tiers. In Tier 1, patients can measure their vital signs through sensors (i.e. ECG, EEG and SpO2) and send these signals to Tier 2, which is a personal gateway (e.g. handheld devices, PDAs and laptops) that uses LAN protocols (e.g. Zigbee and Bluetooth) and WBAN. Medical data are sent from Tier 2 to Tier 3, which is the healthcare provider in MIs. This category contained 119 out of the 150 articles (79.33%) and was divided into sensor based, gateway and mHealth and server based.
Sensor based
This section describes and summarises the issues and technologies of sensors that can provide constant and reliable healthcare monitoring. WBANs consist of small wireless sensors that transfer and gather information on a patient’s vital signs [42]. This section contained 44 out of the 150 articles and was divided into five subsections according to the issues and technologies in sensor-based telemedicine. Of the 44 articles, 1 focused on the ontology-based sensor and extended topology principles that characterise wearable sensor platforms and composed of mainstream magnetic and inertial measurement units (MIMUs) [43].
Reliability
WBANs transmit physical data from patients throughout a network and to a remote data centre and thus require reliable connection. Biosensors with varying bandwidth allocations need the simultaneous transmission of vital data, and this mode of transmission leads to network congestion [44, 45]. This subsection contained 18 out of 44 articles, one of which focused on false alarm detection, particularly on systems detecting and minimising false alarms generated by monitoring sensors and ensuring that the smart alarm systems of sensors have optimum performance in terms of accuracy and efficiency [46]. The other articles covered congestion control, link quality and packet delay and EMI perspective.
Link quality and packet delay
This subsection consisted 10 out of 18 articles and focused on link quality and packet delay in sensors. One article developed real-time publish–subscribe (RTPS) middleware through healthcare systems. RTPS guarantees real-time and simultaneous data transmission while preserving QoS [47]. The second article focused on decision planners and investigated multi-attribute decision-making methods [48]. The third article proposed two new scheduling algorithms capable of overcoming the starvation mode of the packets without the highest priority and satisfying the QoS requirements in WBAN networks [49]. The fourth article investigated an architecture for handling dynamic behaviour and heterogeneous traffic in WBAN for healthcare systems [11]. The fifth article examined a new traffic critical WBAN using queueing discipline with non-preemptive priority [50]. The sixth article proposed the use of medium access control (MAC) protocol for the inclusion of the priorities of bio signals with various attributes; the purpose of this method is to guarantee data effectiveness and arrange least packet deferment period in order [51]. The seventh article focused on the health surveillance scheme and a sensor structure with simulation outcomes [52]. The eighth article presented an infrastructure that depends on a technique ameliorating telehealth programme characteristics through the control of the characteristics and distribution of the Internet traffic among linked devices in a home area network (HAN) environment [53]. The ninth article improved the MAC protocol of WBANs by adjusting resource allocations and prioritising traffic depending on the channel and health conditions of the user [54]. The last article presented a compositional probabilistic response time evaluation approach to probabilistic actual systems in body area sensor networks with fixed-priority pre-emptive scheduling [55].
Congestion control
Congestion control is a challenge in healthcare WBAN. Changeable traffic load, many-to-one connection type and restricted bandwidth positions are among the main causes of congestion in such applications [44, 45]. This issue is familiar in any data network, such as wireless sensor networks (WSNs), and results in packet loss, expanding end-to-end lag and considerable energy consumption because of repeated transmissions [56]. This subsection contained five articles. Two articles focused on control protocol and congestion detection for remote surveillance of patients’ health status using WBANs [44, 45]. Two other articles presented a congestion control protocol for adoption in healthcare implementations in WSNs [56, 57]. One article proposed that priority depends on a congestion avoidance hybrid schema for WSNs, which not only prevents congestion but also provides an efficient mechanism for energy conservation [58].
Electromagnetic interference
Wireless connection enables mobility and provides reliable service for various e-health implementations, such as telemedicine, mobile hospital information system and remote patient monitoring [59]. A crucial problem in using wireless connections for healthcare scenarios is EMI caused by radio frequency transmission. A high EMI level can result in crucial defects in medicinal sensors. In such instance, few clients who are not transferring urgent data would need to lessen their transfer capacity or even disconnect from the network for a short time to allow the regular operation of medicinal sensors and the transfer of urgent data [60]. Two article included in this study focused on EMI. One article proposed a method that reduces the number of clients compelled to disconnect from the network while maintaining the EMI of medicinal sensors at an agreeable level [60]. The other article introduced a priority scheme for medical and non-medical devices to support an effective wireless healthcare service system [59].
Energy efficiency
Directional antenna technology provides additional possible options for the enhancement of energy efficiency and reliable data transfer in wireless networks, particularly in battery-operated networks [12, 61]. This subsection contained 11 articles, which were divided into traffic routing and data transmission packet perspectives. Ten articles focused on data packet transmission, and six articles focused on ensuring high energy efficiency and robust data transmission by prolonging the network lifetime, reducing energy consumption and ensuring that tasks are completed without delay by expanding the predictability of a system [12, 14, 61,62,63,64]. Three articles presented a priority-based time slot allocation scheme for WBANs by using slot allocation schemes for prioritisation and achieving energy efficiency for the WBAN [65,66,67]. One article presented a green cloud-assisted healthcare service on WBAN and determined the sensing frequency of the physical signs of different body parts and the data transportation between sensor knots of WBAN [68]. Only one article focused on the traffic routing perspective, which guarantees dependable traffic dissemination and personalised channel access to human body connections [69].
Quality of service
As the natural and physical data gathered by multimodal sensors have various levels of importance, the deployment of sensory data QoS in WBAN is a critical issue [70]. This subsection contained five articles, which focused on QoS for WBANs and provided parameters, such as delay, queue length, packet loss rate and throughput, to extract QoS execution measures [42, 70,71,72,73].
Security-and-privacy-based sensor
The security of gathered and transferred data from medicinal sensors is critical regardless of whether the data are located in the system or stored in the main server. Efficient and secure data gathering is essential because it ensures the integrity of data delivery and the privacy of such data [74]. This subsection contained five articles that focused on security-and-privacy-based sensor. The first article implemented a model biomedical sensor application that uses TinyECC to secure wireless communication among sensor knots and assessed the feasibility of using TinyECC in a real-time sensor network [75]. The second article focused on the secure logging of information collected by knots in a WSN [13]. The third article provided numerous levels of security through encryption and a distance bounding test to prevent long-distance attacks; the method is generally used in body area networks for medicinal devices where security is imperative [76]. The fourth article described a process in which compressed data are encrypted and integrity is protected by a cryptographic hash algorithm to maintain data integrity [74]. The fifth article proposed the comprehensive Integrating the Healthcare Enterprise (IHE) initiative based on X73PHD expansion composed of additive layers adapted to various e-health/mHealth applications after analysing the characteristics of X73PHD (particularly its built-in security), IHE profiles related to these implementations and other studies [77].
Evaluation-and-assessment-based sensor
This subsection presents evaluation and assessment studies of the sensor side of telemedicine. Out of 44 articles, 4 cover this topic. One article evaluated the performance of the IEEE 802.15.6 standard in terms of latency, energy consumption, packet delivery rate and packet breakdown at the MAC layer while satisfying the ISO/IEEE 11073 requirements [78]. Another article evaluated the performance of the IEEE 802.15.6 standard when used in various sensors of the Cane Network eHealth Project [79]. Another article assessed the efficiency of wearable health surveillance devices in decreasing elementary care patient load and improved the connections across different healthcare units [80]. The last article evaluated the miniature wireless vital signs monitor for potential shock triage in an intensive care unit [81].
mHealth and gateway based
mHealth or gateway is a general term for the use of mobile phones (or any handheld device) and other wireless technology and communication devices for disseminating information about preventive healthcare services. This section contained 32 out of 150 articles and was divided into six subsections, as detailed below. A context-based and rule-based approach for designing adaptable MUIs in mHealth was proposed in [82]. Meanwhile, an evaluation study was conducted on the technical feasibility of medical alert dissemination in an urban environment through a mobile device during congestion or failure tolerance in a network infrastructure [83].
Treatment support and disease surveillance
The main roles of both topics is to predict, observe, monitor and minimise the harm caused by outbreak, epidemic and pandemic situations and increase knowledge on exacerbating factors. This subsection contained 9 articles. Two articles proposed the concept of allowing patients to monitor and manage chronic diseases and vital signs, such as heart rate, body temperature and blood pressure (BP), either through the use of biometrics, such as (e.g. mobile machine learning model), or through an Arduino Mega micro-system device [84, 85]. Two articles presented applications that can be adapted to other diseases (e.g., high or low blood pressure and diabetes) through biometric devices, such as glucometers, tensiometers and thermometers [86, 87]. Two articles described a social media system, such as a mobile application or software, for the monitoring of vaccination coverage among children in rural communities [88]. A new system for detecting and preventing dengue in Sri Lanka and in the rest of Southeast Asia regions was developed in [89]. A mechanism for personalised and adaptive daily interactive sessions (daily living) for the treatment of major depression was developed in [90]. Continuous, non-invasive and wireless monitoring of patients with Parkinson’s disease was presented in [91]. A new approach on personal coaching systems (PCSs) for body sensing systems and integrated with smart reasoning and context-aware feedback was proposed in [92].
Disaster management
Disaster management is the organisation and management of resources and responsibilities for dealing with humanitarian aspects of emergencies (i.e., preparedness, response and recovery) for the reduction or minimisation of the negative effects of all hazards determined by an mHealth management system for natural disasters. This subsection contained six articles. Two articles used the mHealth system in a tsunami disaster scenario and proposed a platform for field accidents and a monitoring system for an intelligent emergency centre [93, 94]. A real-time system for patient assessment and monitoring via crowdsourcing through mobile electronic triage and sensor-detected information was demonstrated in [95]. Another proposed system provided situational awareness (SA) in indoor and outdoor settings for urban search-and-rescue operations [96]. A process of tracking the safety of pilgrims in holy regions in case of a natural disaster was presented in [97]. Project Ripple was conducted for the production of an medical body area network (MBAN) of sensors that can be used in realistic disaster scenarios and that facilitates patient triaging and modern physiological data collection [98].
Integration and aggregation
The integration of information from multiple heterogeneous and distributed data sources enables the use of healthcare data in medical and clinic centres and allows mobile operators to create solutions that connect healthcare providers with patients. Otherwise, at the mobile aggregation centre, data at the mobile aggregation centre are accumulated. This approach ensures the scalability and flexibility of the telemedicine system. This subsection contained 5 out of the 32 articles. Linear sequential data modelling with an expert-centric priority-based approach was proposed in [99]. A theory-based approach and highlights of the design decisions among technology, architecture and algorithmic solutions were presented in [100]. Healthcare environments in virtual organisations were integrated in [101]. Data were aggregated either by using a cloud-assisted WBAN-based architecture in [102] or by using a priority-based health data aggregation scheme for cloud-assisted WBANs with privacy preservation in [103].
Network management
Mobile phones and wireless technologies support mHealth objectives, including the development and enhancement of mobile healthcare network management, through text messaging, wireless devices and mobile phone applications. Four articles are included in this subsection. Of these articles, two focused on an aspect beyond WBAN communications either by introducing a priority-aware pricing-based capacity sharing scheme for a radio resource allocation scheme [104] or by proposing an incentive-compatible mechanism in e-health networks for transmission scheduling with the delay sensitivity of medical packets [105]. A multi-user sharing scheme with diverse medical information was proposed in [106]. In the approach presented in [107], the reliability of communication was enhanced through the classification of challenges and by using a mobile ad hoc network for the monitoring of patients.
Ambient-assisted living
AAL allows the monitoring and tracking of patients that lives alone at their homes, are treated in hospitals and have decreasing independence. This subsection contained four articles. An ubiquitous system that uses audio and video for the detection of falls of patients was developed in [108]. The design and implementation of a semantic, data-driven and cloud-based backend platform through information and knowledge-based services was conducted in [109]. In [110], the activities of a single patient at home were modelled for the simulation of daily activity. Developments in ICTs, such as Internet of Things (IoT) and cyber-physical systems (CPS) with more intelligent and prediction capabilities both for daily life (home/office) and in hospitals, were reported in [111].
Decision support system
DSS is a computer-based system that aids the decision-making process to ensure correct diagnosis of any disease or illness. This subsection contained two articles. A model for developing the quality of decisions in mHealth; this model was found to enhance context awareness and processing and improve the presentation of information to healthcare professionals [112]. A lightweight rule-based reasoning system was designed and optimised in [113] for the structuring of the knowledge base of DSSs that can be embedded efficiently in mobile devices.
Server based
The third section of articles on telemedicine architecture is server based (Tier 3). Server-based telemedicine uses a remote computer for real-time monitoring. A remote monitoring server can help medical professionals analyse data in real time to provide compatible services to patients, as well as and perform management, organising and support functions for professionals in telemedicine. Server-based telemedicine includes the MI server, patient history and database, and service generation [4]. This section contains 43 out of 119 articles and is divided into six subsections according to the features and contributions of server-based telemedicine architecture. All these subsections are briefly described below.
Analysis process
This subsection provides insights into data analysis in telemedicine. In general, data analytics services can monitor and detect vital signs and other measurements, which can be provided to physicians or healthcare providers for diagnosis [114]. Two studies analysed the process of telemedicine servers. One of them focused on big data analytics for sensing technologies; this approach considerably improved the efficiency and effectiveness of healthcare services [114]. While another focused on activity pattern mining and showed that extracting frequent patterns for the history log of smart home sensors can contribute to activity pattern mining, which can facilitate the creation of an activity database [115].
Environmental management
This subsection presents the management of environment and medical facilities. A focus on the management of health institutions is important because of dynamic processes, distributed hospital organisation and long waiting times in EDs, which may lead to death. Therefore, health institutions must review the process of managing emergency facilities and implement measures to preserve the quality of care for patients [11]. This section consisted of three articles, two of which focused on the management of sensors and data collection for health monitoring of elderly people in hospitals [116, 117]. One article focused on the approach of supporting doctors for the enhancement of management and prediction of problems caused by patient overcrowding [118].
Evaluation and assessment-based server
This subsection presents evaluation and assessment studies on healthcare systems based on the server side of telemedicine. This subsection contained three articles. Two studies evaluated the features and effectiveness of common telehealthcare systems, which aim to set up a widespread, user-friendly and centred patient system for patients and healthcare providers, on the basis of clinical guidelines and integrated personal electronic health records (EHRs) [119, 120]. Another study investigated the efficiency of a Web-based healthcare system that allows users to record their systolic BP, diastolic BP and body weight and the number of steps they walked in a day [121].
Security and privacy-based server
This subsection presents the security and privacy issues faced by servers in telemedicine architecture and contained only two articles. One article focused on the security of medical data collected from medical sensor networks by proposing a mechanism that ensures integrity, confidentiality and fine-grained access control over medical data [122]. The second article focused on the security of an e-Healthcare society by using a proposed security system called low-cost and secure (LCS) communication system, which allows various actors of the e-Healthcare society to communicate securely [123].
Collaboration fields
This subsection reviews and describes various activities and collaboration fields in the telemedicine server. This subsection included seven articles and was divided into two subsections, namely, cooperative environment and tele-expertise among professionals.
Cooperative environment
Cooperative environment involves ubiquitous healthcare (u-healthcare) environments in virtual organisations. In particular, each individual in a physical environment can share and exchange information and medical data collected from the medical sensors, medical devices and desktop computer over LANs. This subsection contained two articles. One article focused on decentralised data, wherein electronic health records (EHRs) and personal health records (PHRs) can be saved in distributed data centres, and decentralised data can be accessed from other distributed data centres with a high level of performance [124]. The second article focused on enhancing healthcare information systems and providing high-quality information anytime and anywhere and offered distributed and heterogeneous resource access solutions that meet user requirements in different contexts [125].
Tele-expertise between professionals
This subsection presents the collaboration and exchange of experience among physicians or professionals for the formulation of appropriate decisions for diagnosis and treatment. This subsection contains five articles, all of which focused on tele-expertise or the sharing of knowledge and expert advice among health and/or medical professionals; this approach facilitates the decision-making process for diagnosis and treatment [2, 5, 126,127,128].
Remote monitoring (telemonitoring)
This subject is the largest section in the server-based category and provides clarifications on telemonitoring in the telemedicine domain. The Heart Rhythm Society defined remote monitoring as automatic data transmission based on a pre-alert on device functionality, clinical events and clinical status of patients [4]. In remote monitoring, medical professionals remotely monitor and interpret a patients’ medical parameters, analyse data in real time, and provide instant feedback [4]. Patients’ data can be recorded and transmitted automatically by the patients themselves or with the assistance of a healthcare professional [2]. This section contained 26 articles and was divided into three subsections.
Patient prioritisation
This subsection presents the prioritisation of patients. Patients are listed in order of severity of condition before their treatment and transport to hospitals. Two articles focused on remote prioritisation, which indicates triaging patients for treatment and transportation to hospitals by assessing their vital signs. Patients’ conditions should be the primary assessment tool in determining the priority category according to the medical guidelines [129, 130].
Patient triage
‘Triage’ comes from the French word trier, which means ‘to sort’. The concept of triage was first applied in warfare when a system was needed for the prioritisation of casualties and provision of instant care to the most seriously injured. In the hospital domain, triage has traditionally depended on the ability of nurses to prioritise the status of patients. Triaging involves the initial sorting of patients who arrive at the ED and quick recognition of patients who require instant care because of urgent and life-threatening conditions [4]. This subsection contained eight articles, which are divided into two perspectives as follows: inside ED triage, which was discussed in three articles [9, 10, 131] and outside ED triage, which was discussed in five articles [4, 8, 132,133,134].
Provide services to patient
Providing services to patient is a key part of telemedicine because this is the patient treatment process. Personalisation means understanding the needs of each individual/user and addressing these needs in a given context [4]. Personalisation mainly consists of two steps, namely, user modelling/profiling and content/service recommendation according to user profile [4]. This subsection contained 16 articles, six of which focused on the support for alert emergency service generated when the vital signs of a patient becomes abnormal. The alert is generated to emergency medical teams for fast response [135,136,137,138,139]. Five articles presented services such as telehealth consultation, drug prescriptions, tips, recommendations and suggestions [140,141,142,143,144]. Two articles suggested the selection of the nearest and appropriate specialised hospital and available doctor depending on the patient’s status [145, 146]. One article studied the provision of healthcare services on the fly among vehicles that seek access to healthcare services while travelling [147]. One article focused on providing first aid in an ambulance [148]. Another article presented a novel telehealth eldercare service that connects the clinic of a remote physical therapist and the home of a senior; this service provides verbal, auditory and visual cues to the elderly individual to enable him or her to perform the correct exercise movements [149]. One study presented a method for the management of prescribed medication for patients with visual difficulties through notifications on doses and drugs [150].
Distribution results
Figure 4 shows that many papers were published by the three digital databases. The review and survey of this work consisted of two primary categories, namely, review and survey papers and telemedicine architecture, which consisted of three tiers as follows: sensor based, mHealth and gateway based and server based.
WoS published 30 articles in different categories, which are composed of review papers (3), sensor based (12), mHealth and gateway based (5), and server based (10). IEEE Xplore published 36 papers, which ware composed of sensor based (19), mHealth and gateway based (8) and server based (9). ScienceDirect published 84 articles, which were composed of review papers (28), sensor based (13), mHealth and gateway based (19) and server based (24).
Distribution by publication years of articles
Figure 5 presents the number of included papers in the four categories according to the year of publication. The distribution of the scientific papers from 2012 to 2017 is shown below.
Nearly 46 papers have been published since 2015. Four papers were published in 2012. Five papers have been published since 2017. Twenty-four papers have been published since 2013, 34 since 2016, and 37 since 2014.
Distribution by nationality of author
Figure 6 shows that 33 countries and nationalities implemented triage and used priority-based sensor technology. We observed that the literature studies were conducted in certain countries or they covered cases in these countries.
The nationality distribution of the 150 telemedicine technologies papers in numbers and percentages shows that the most productive authors are from the United States (27), followed by India (12); China and France (11 each); Saudi Arabia, Tunisia, Canada and Korea (7 each); Belgium, Australia and Spain (6 each); Iran (4); the United Kingdom, Italy, Malaysia, Japan, Indonesia, and Portugal (3 each); Germany, Taiwan, Algeria, Columbia, Russia, Holland, and Turkey (2 each); and Switzerland, Hungary, Bangladesh, Brazil, Singapore, Cyprus and South Africa (1 each).
Discussion
This study aims to present updated and state-of-the-art triage and priority technologies inspired by the use of sensors in telemedicine technologies. This study also aims to highlight the research trends in this area. This survey is different from previous reviews because of its relevance, and it focuses on the telemedicine application literature rather than on the applications themselves. A taxonomy of the related literature is proposed. Developing the taxonomy of the literature in a research area, particularly an emerging one, can provide several benefits. Firstly, a taxonomy of the published works organises publications. A new researcher who is studying triage and priority-based sensor technology in telemedicine may be overwhelmed by the large number of papers on the subject without any kind type of structure and may fail to obtain an overview in this area. Various articles address the topic from an introductory perspective. Other works examine a selected number of existing telemedicine technologies, whereas some may contribute real techniques to the field. A taxonomy of the related literature, as shown in Fig. 3, helps systematise these different studies and activities into a meaningful, manageable and coherent layout. Secondly, the structure introduced by the taxonomy provides researchers with important insights into the subject in several ways. Such structure outlines the potential research directions in the field. For example, the taxonomy of telemedicine technologies in this work shows that researchers are inclined to propose and develop healthcare service systems in hospitals for monitoring and analysing vital signs collected from patients to perform processes, generate services, provide support to professionals and manage the environment. Other areas include sensor technologies and mechanisms and their use at home and in the medical environment for reliable health monitoring. These sensors detects vital signs from patients for transmission to remote monitoring systems. Other research directions identified in this taxonomy include the development of mHealth applications and the enhancement of the features and capability of mHealth in tracking and monitoring diseases. A taxonomy can also reveal the gaps in telemedicine technologies. Mapping the works on telemedicine technologies into distinct categories highlights the weak and strong spots of research coverage. For example, the taxonomy in this article shows how groups of individual technologies are receiving considerable attention in terms of review and telemedicine architecture (as reflected by the proliferation of their categories) at the expense of integrated solutions and frameworks and development efforts. In a survey on an adequate and representative sample of the literature, the taxonomy also highlights the lack of studies on developing telemedicine technologies. Our taxonomy highlights some of the fundamental aspects of telemedicine technologies, such as monitoring devices, and those of mHealth and healthcare service systems that have received more attention from researchers compared with traditional technologies. Researchers working on an area of interest adopt a certain taxonomy by developing a common language through which future works are shared and discussed. For example, For example, for medical institute server that aims to classify patients and provide personalised healthcare services from appropriate hospital according to triage level of a patient with chronic heart disease; for mHealth process of classifying patients according to emergency level to provide personalised healthcare services in case of medical institute server failure happens by selecting an appropriate hospital, and in case of network failure happens by providing a tips to patient; patients with multi-chronic disease can be prioritised as well. Related works could can take the form of a development paper, a comparative study or an overview. Statistical data on individual categories of the taxonomy identifies involved sectors in telemedicine technologies to adapt with new trends and strengthen less active areas. Similar to taxonomies in other fields, a common language is developed among researchers to communicate and discuss emerging works, such as development papers, comparative studies and reviews on telemedicine technologies. On the basis of the survey, three aspects of the literature content are identified, namely, the motivations behind developing telemedicine technologies, the challenges to the successful utilisation of these technologies and recommendations to alleviate these difficulties.
Motivations
The field of telemedicine has been developed rapidly because it offers obvious and compelling benefits. In this section, we present its benefits as described in the literature, which are organised into six categories according to related benefits. The corresponding references are presented for further discussion (Fig. 7).
Benefits to healthcare security
Data security and privacy are serious requirements in different applications. Securing medical information between health stations and sensing nodes (SNs) is important to patients and health professionals. Security is crucial to the successful implementation of telemedicine applications. Poor security and privacy may reduce the quality of care, lead to a lack of trust in healthcare services for both users and providers and cause legal liability. The security and privacy of medical data collected from patients should be guaranteed during transmission to the medical centre and during storage [13, 74, 122]. Long-distance attacks can be prevented by implementing multiple levels of security protocol, including encryption and distance bounding tests. [76]. The X73PHD-IHE model ensures secure connections to mobile aggregators and private sharing among different personal health device users [77]. Furthermore, a biomedical real-time sensor network can use TinyECC (public key cryptography algorithm) to secure communication between sensors and gateways [75]. Machine-to-machine (M2M) LCS communication systems use intelligent authentication by using a random distributive key management scheme, electronic certificate distribution and modified realm Kerberos to guarantee secure interactions in M2M electronic healthcare systems [123].
Benefits to quality of network service
QoS for sensor data in WBANs is an important issue. This section lists the benefits of improving the quality of network services in terms of priority scheduler, congestion control, packet loss, drop, delay, jitter and throughput. In WBANs, priority scheduler is important because some biological signals are more significant than others. Furthermore, health data are of different types, which have corresponding priorities. Therefore, emergency data packets should be transmitted with minimum delay. [42, 49, 50, 54, 66, 70, 102,103,104]. Infrastructure-based solutions for HAN management in case of multiple devices are connected to the same HANs by prioritising the bandwidth of HANs [53]. Hospital networks are mostly grouped into wireless medical devices and wireless non-medical devices. Spectrum-aware cluster-based network architecture and EMI-aware communications protocols prioritise wireless medical devices during transmission, thereby contributing to the improvement of QoS and network efficiency [59]. Overcoming issues such as packet loss, drop, delay, jitter and throughput can improve the QoS of the WBAN network [11, 47, 48, 51, 69, 71, 73, 105]. Signal quality for physiological signal extraction can be enhanced by a low-cost reflective photoplethysmography (PPG) system for the postprocessing digital filter process [14]. The failure rate of services for non-real-time consumer calls can be minimised for service quality enhancement by using a multi-user sharing scheme in the mobile healthcare system [106]. Overcoming congestion control in the network can increase efficiency and improve QoS because congestion control is one of the main concerns in the WBANs of healthcare applications. Congestion detection and control protocol for WBAN with multiple biosensors is important in enhancing the quality of network service [44, 45, 56,57,58].
Benefits to power efficiency
Increasing power efficiency is one of the most critical issues in WBANs in the development of technologies for wireless medical devices. Such devices do not need to be accessed over a long time period to conserve their power, and power consumption limits are needed to sustain the devices over many years. Many strategies for limiting power consumption increase the lifetime of a network with battery-powered sensor nodes. The lifetime of the node can be extended by easing power consumption and integrating a scheduled access mechanism and directional antenna technology in the lifetime extended directional approach (LEDA MAC) protocol [12, 61]. Moreover, implementing a sleep time for sensor nodes can increase power efficiency [62, 68]. A slot allocation scheme for the MAC protocol can achieve energy efficiency for WBANs [65, 67], and energy consumption can be reduced and the lifetime of the network can be extended by decreasing transmitting frequency and maximising the sleep times of WBAN nodes [63]. Medical data transmitted by users can be scheduled with a joint power and admission control algorithm; this approach reduces the number of users required to disconnect from the network and maintains the EMI levels of medical sensors at an acceptable level [60]. The AAEEPMPM protocol for body sensor networks has been designed and implemented in a hardware platform for power efficiency and improves network lifetime. AAEEPMPM conserves the battery power of a sensor by using the activity context of the wearer [32, 64]. A fog computing-based solution can be used for the enhancement of the energy efficiency of IoT architectures used in healthcare applications [111].
Benefits to patient
EDs are places where a large number of people must be attended in a short time and where critical situations are expected to emerge. When a patient arrives at the ED, they need to be classified according to the seriousness of their conditions for prioritisation. A healthcare application remotely recognises patients with the most acute emergency case; the patient with the most acute emergency case is the first to obtain a response from the server [4, 9, 129, 130]. This system offers other benefits during natural disasters and MCIs, such as tracking and monitoring the situations of the casualties in case of rapid destruction of the telecommunication infrastructure. Communicating the state and location of injured individuals is necessary during medical emergencies. During the congestion/failure of infrastructure-based communication networks, mobile/wireless (ad hoc) networks can be used for the tracking and monitoring of health conditions and sending an alert to hospitals or medical field personnel [83, 93]. Mobile ad hoc networks can optimise the network coverage area and transmit from an area without coverage from infrastructure-based networks [107]. ZigBee is used for the monitoring and/or tracking of pilgrims in areas hit by a natural disaster and sends heartbeat signals to medical personnel. Healthcare systems can ensure the safety of seniors and people with decreasing independence at home by automatically detecting falls and distress situations to call for help [91, 108]. The OCarePlatform intelligent healthcare service system assists elderly people who have chronic illnesses and are staying at home for a prolonged period [109], and smart homes allow elders with Alzheimer’s disease to stay in their home at a long time because they can automatically receive real-time support for their daily activities [115]. Home healthcare robots can make clinical information available to patients at the right place and time, thereby decreasing error and increasing quality and safety [16]. Meanwhile, the PTaaS system connects a clinic with an elderly person at home and allows the therapist to monitor a patient’s condition and provide oral, auditory and vision cues for implementation of correct practice movements [149]. A healthcare monitoring system can be used for health monitoring, particularly of the elderly and persons with disabilities and provide them with a service-oriented emergency response when they suffer abnormal health conditions [119, 136]. SERVANDO encourages the self-management of diseases generated during the monitoring by the patients through the inculcation of supervised exercises in the home of patients [150]. The INCASA architecture combines telehealth and telecare monitoring, enables the deployment of services during follow-ups, monitor the suitability of in-house environmental conditions and determine deviations from their regular activities [137]. A nursing home system is useful in promoting early diagnosis and treatment [138], and telemedicine improves the management and monitoring of various diseases, especially chronic disease, by using information and communication technologies. Some systems can monitor patients with diabetes and generate recommendations and services [20, 86, 87, 99], while other systems monitor vital parameters of patient and generate alerts to the caregivers in case of abnormal values, thus ensuring the safety of patients with chronic diseases [24, 113, 135, 139]. DSS can support ambulance cars and EMS responding to emergencies involving acute coronary syndrome [145]. PCSs support people with chronic conditions in developing and maintaining healthy habits [92]. Jeev tracks the vaccination of children [88]. High-quality and evidence-based mHealth programs that can support self-management of diseases and adjust education distribution [23] provide clinical services to patients with mental illness [33]. Mo-Buzz, a mobile-based dengue communication system, sends customised health messages to promote preventive behaviours and health awareness [89]. A high level of personalisation of personal health systems based on users’ needs is necessary to support the remote treatment of people who are recovering from a major depressive disorder [90]. A diagnosis and monitoring system based on real-time and predictive data processing is proposed for patients with mental disorders [143]. An automatic early stress recognition system is important to detect stress in its early stages to for preventing stress from becoming chronic and resulting in irreversible damage [21]. A platform in which digital technologies facilitate patients’ participation in the healthcare delivery process has been developed [18]. An on-the-fly e-healthcare system is needed to provide healthcare services to patients on the move because; providing prompt medical services can save millions of lives [147]. A first-aid system in ambulances has been developed [148]. Meanwhile, measuring vital signs generally requires the superficial attachment of physically or logistically obtrusive sensors to subjects, thereby irritating the skin or adversely influencing the subject. Thus, an approach that monitors vital signs internally from the gastrointestinal tract is needed for patient comfort [144]. An SOA framework has been developed to improve the QoS for decision making and timely alert generation by providing clinical and non-clinical services; this framework guarantees the availability of services to patients with reduced throughput and response time [141]. A system that enables the analysis of data collected from sensors in real time can significantly improve user safety monitoring and the accuracy of the event prediction process [114]. Telemedicine services can effectively improve the quality of healthcare in large centres and deliver these services to unserved and underserved areas. A healthcare system can be used to recognise and decrease morbidity by providing health consultations in unreached areas [32, 140, 146].
Benefits to medical organisations
Managing healthcare organisations is complex owing to the dynamic operations and distribution of hospitals. Thus, healthcare institutions must focus on this issue to meet the requirements of patients. Multi-agent systems (MASs) manage and enhance the function of paediatric emergency departments (PEDs) experiencing stochastic arrival of patients and service overcrowding [118]. Organisations can integrate real-time RFID/sensor data into current and future IT applications to increase SA, edge-based management, and dynamic capabilities [100]. MAS is used in indoor medical environments for the management of medical sensors and collection and storage of medical data in databases [117], and it offers other benefits to medical organisations linked to acquire patient information, such as PHRs and EHRs, anytime and anywhere. The ontology-oriented framework for pervasive applications and services (ONOF-PAS) is used for the intelligent management of the tasks, processes, resources, and messages among different medical organisations [125]. A distributed system uses data coherence protocol, wherein PHRs can be stored and accessed by distributed medical data centres [124]. A u-healthcare agent system enables patient information retrieval and inter- or intra-management of healthcare workflow, disease progress monitoring or tracking and remote access of patient information for multi-attribute decision making during an emergency [101].
Benefits to physicians
In a mass casualty situation, the emphasis shifts from ensuring the best potential outcome for each individual patient to ensuring the best potential outcome for the greatest number of patients, helping medical teams acquire real-time information of multiple casualties for timely and accurate treatment and enabling rapid and optimal resource assignment according to the seriousness of the status of the patients’ status [8, 10, 94, 95, 98, 131,132,133,134]. Incident commanders and responders can communicate by using DIORAMA, which helps responders gain real-time SA of the incident sites [96]. Tele-expertise can assist knowledge sharing and decision support among physicians across organisational and geographical boundaries. Such a task is complex and important, and it is the core of the cooperation among telehealth, health professionals, and medical professionals; this cooperation enables them to make suitable decisions for patient diagnosis or treatment and effectively manage the medical information of their patients [2, 5, 126,127,128]. Mobile technologies can facilitate the work of healthcare professionals by improving the presentation of information to healthcare professionals and increasing the speed of decision making, especially during emergencies. Context-based and rule-based approaches for designing adaptable MUI in mHealth provide the best possible means that increases the efficiency of healthcare professionals [82]. In healthcare applications, a doctor should monitor and observe patients regardless of time and place, and an efficient smart alarm healthcare alarm system can detect and minimise false alarms generated by patient-monitoring sensors [46, 112]. The M4CVD system presents relevant and summarised information on the status of a patient from all the acquired data; it classifies a patient as ‘continued risk’ or ‘no longer at risk’ for cardiovascular disease (CVD) [84]. Cloud computing enables physicians and healthcare workers to recognise and treat non-communicable diseases in rural and remote communities in Bangladesh through an e-health consultancy system called On-Cloud Healthcare Clinic [142].
Challenges
Many developers and researchers have conducted studies on the various fields of telemedicine. Unfortunately, the studies have no perfect solutions for the issues regarding the healthcare service delivery in many other domains. By surveying these studies, we found that researchers are concerned about the challenges in telemedicine related to sensors in WBAN, smartphone applications, and servers in medical healthcare centres. The main challenges in the adoption of telemedicine are listed below, along with citations to references for further discussion. Figure 8 shows the classification of challenges according to their nature.
Concerns on network optimisation
The most persistent and critical challenges in telemedicine are related to network optimisation. Various challenges, such as QoS, congestion, interference, data priority, transmitting data, traffic management, failure tolerance and reliability, exist and must be classified. For QoS provisioning of the delivery of sensor data at multiple levels in WBANs, issues, such as like packet loss, drop, delay, jitter and throughput should be addressed and WBAN performance must be improved. In this regard, many researchers have proposed various means, such as designing a reliable and efficient MAC protocol, establishing traffic during emergencies, modelling various traffic generated from various events, response time analysis, and data dissemination and medium access in WBAN [11, 51, 54, 55, 69, 71, 72]. Several other problems are related to QoS, particularly interoperability and subjectivity [73]; telemedicine and interoperability among devices, such as laptops, desktops and mobile devices [126]; reduced handover [48] and lack of sensory data delivery at multiple levels in WBAN [70]. Congestion control is a major challenge in network optimisation; existing congestion control protocols do not focus on signals carried in WBANs and thus cannot be applied directly in WBAN [44, 45, 56,57,58]. Challenges exist in data transmission during a critical medical situation or between gateways and remote medical centres [66, 104, 105, 116]. Other issues, such as medical band and EMI in biomedical devices and the delay-sensitive scheduling for wireless transmission beyond the environment of mobile hospitals also exist [59, 60, 63]. Moreover, WBANs are inadequately implemented with respect to data priority issue and the effect of user priorities on the monitoring of cardiac patients, and non-linear and dynamic changes in slot allocation schemes with data priority persist [50, 65, 78]. An Internet traffic management system that enables telehealth applications to acquire higher priority and achieve long-term monitoring with limited battery power is lacking [53, 106]. Challenges also exist with regard to the state and position of injured and wounded people in crucial situations or crowd aggregations during urgent care and medical emergencies [83]. Lastly, enhancing the reliability of communicating the status of individuals with the use of a mobile ad hoc network remains difficult [107].
Concerns on disease monitoring
Disease monitoring is a major issue in telemedicine. Most studies addressed the challenges of monitoring patients with CVD diseases by using algorithms to analyse heart rate signals in real time for processing and summarising raw data; these algorithms help healthcare professionals to make correct decisions when the patient is outside the medical setting [9, 84, 85]. Diabetes monitoring is ideal for a patient who has diabetes and needs constant monitoring during normal activities. [86, 87] aimed to develop a practical e-health solution for diabetic patients in rural and remote communities in Bangladesh by using cloud computing technologies to enhance healthcare services [142]. Psychological issues, such as stress, loneliness and anxiety, are not included in the design of e-healthcare systems [123]. The issue of effective monitoring of a patient with mental disorders in the community and in a smart-psychiatric intensive care unit has been raised [143]. Moreover, the delivery and management of critical information on patients with conditions, such as major depression, is lacking [90]. Patients with Parkinson’s disease can also be monitored while they are at home; this approach minimises the risk of fall and injury and enables the monitoring of the effects of dosage changes [91].
Other reported challenges include the need for an integrated mHealth system that classifies limitations and enables the prediction and prevention of diseases, such as dengue fever, through the optimisation of social media [89, 121]. A vast majority of military trauma deaths occur prehospital, and a significant proportion of in-hospital mortality occurs in patients with no vital signs in the field. Thus, significant opportunities exist for reducing trauma mortality through innovation in the prehospital setting [81]. In developing countries, the need to strengthen immunisation monitoring and surveillance for the reduction of childhood deaths has been emphasised by the World Health Organization (WHO) and UNICEF [88]. The complex problem of monitoring activities and drawing suitable conclusions on the basis of low-level sensor information was raised by [110]. The problem of morbidity (poor health) in unreached communities and the manner by which an e-health system can reduce this problem has also been stated [140]. Low-profile external vital signs of monitoring systems and extended monitoring in non-wearable formats have been gradually developed [144]. Finally, in the Western world, the challenges of healthcare services have been addressed substantially during the last decades. Quality and quantity have to increase to meet healthcare requirements in terms of care monitoring, especially for cases with chronic diseases [92].
Concerns on general healthcare services
Current healthcare services face major challenges for which health professionals should be prepared. Such challenges vary in their concepts. Optimisation problems can be solved by using the PSO algorithm, which has been used for real-time applications in a changing environment; its use can create solutions that optimise traditional health systems, thereby increasing availability without requiring health professionals to exert additional efforts [129, 139]. Challenges, such as scalability, mobility, reliability, scalability and energy efficiency in healthcare systems can be addressed by the recent development of ICT technologies. Cloud computing, sensor technologies, IoT (activity recognition domain to model wearable sensor networks) and big data analytics systems are emerging technologies [43, 111, 114]. Dynamic environment problems can be addressed by vehicular networks that provide healthcare services on the fly and capable of delivering multiple real-time video streams during an emergency to a medical centre for efficient mHealth teleconsultation [147, 148]. Limited facilities and human resources challenges can be addressed by providing smart healthcare services to elderly people who are distributed in a particular location on a large scale [130, 149]. The WHO stated that MUI adaptability is a major problem in e-health tools and services, including mHealth [82]. Problems in ubiquitous environments include a large number of computing devices, informal operation modes and non-standard privacy of healthcare devices, which does not support compatibility across many devices [101]. Various challenges in telemedicine systems exist, such as medical action scheduling, communication between a patient and a hospital, knowledge management during monitoring, and enhancement of security and risk management [5, 150]. Various benefits of healthcare system technologies cannot be accessed by developing countries because of their limited resources and infrastructure [128]. The dynamic reliability management approach uses health information to determine the remaining useful lifetime of processor cores in MP-SoC. [52]. The weaknesses of CSMA/CA are emphasised in the management of fairly heterogeneous traffic and considering important data rates [79].
Concerns on healthcare data management
Several challenges exist in this field, including integration, aggregation, big data, managing data and data fusion, exist in this field. The integration of vital signs monitoring (telehealth) with behaviour analysis on the basis of home care sensors (telecare) has not yet been addressed on a large scale [137]. However, most challenges in the development of heterogeneous integration systems and relevant data from other devices can be smoothly shared [47]. Although few CPS healthcare architectures have been proposed for healthcare application, they all lack efficient false alarm detection [46]. One issue is sensor integration and radio frequency device (RFID tags) data in information technology applications [100]. The context of body area network context presents new problems for scheduling. Modern healthcare systems do not integrate the mechanisms of inter-WBAN data scheduling and aggregation [42]. No scheduler of priority frame aggregation is currently available for WBAN/WLAN bridging modules [49]. Data should be aggregated effectively and delivered to the cloud platform with minimal delay during disasters scenarios [102]. Thus, efficient aggregation of different kinds of data in WBAN to the cloud server remains crucial [103]. In the medical context, the current telehealth system does not consider the relevance and timeliness of a large data system. A large amount of real-time data are stored and sent to data and medical centres, respectively [124]. The collection, retrieval, storage and analysis of the vital signs of patients and the management, collection and storage of these data in a database remain difficult during the processing large data [117]. The problem of using multiple clinical guidelines to handle frequently collected data is addressed by COMPOSE in [127]. Data fusion is difficult, particularly when input data are heterogeneous [4]. Another concern is the acquisition of a unified dataset by fusing multiple heterogeneous datasets for various types of high-level analysis, knowledge acquisition and reasoning [99].
Concerns on power consumption (or) energy efficiency
Power consumption concerns exist, especially in a WBAN that needs to be classified. Limited battery life remains an issue in wearable sensors for continuous monitoring systems. Maximising the lifetime of a network with energy constraints on battery-powered sensor nodes and ensuring a reasonable battery life are necessary to any sensor system that senses, transmits and processes data in a critical medical situation and to the minimisation of the sleep mode current [61, 62, 64, 66,67,68]. However, most MAC protocols adopt omnidirectional antennas, which are a disadvantageous for power consumption. Directional antenna and scheduled access mechanisms in the EDAMAC protocol are adopted for the minimisation of power consumption for the extension of node’s lifetime [12]. Signals received at the photodetector circuit cannot be guaranteed because the signal-to-noise ratio is negatively affected by short LEDs, and the process continuously minimises average energy consumption [14].
Concerns on decision support system
The integration of DSS into telemedicine clinical practice is increasingly important. In a telemedicine system, accurate data, applicable knowledge and appropriate problem-solving skills are some challenges in decision making. Remote monitoring applications are also faced with the problem of embedding knowledge-based decision support components for seamless and ubiquitous management of chronically ill patients [113]. Challenges related to mobile computing, information quality, healthcare professionals and interoperability should be addressed for the enhancement of mHealth quality [112]. In PEDs, the multi-skill healthcare task scheduling problem has been addressed by an agent-based decision-making support system [118]. The traceability of the decision-making process to deal with tele-expertise opinions is another issue [2]. Coordination and decision-making support challenges require the integration and processing of various data sources within a single solution in cardiological ambulance control [145]. Shortcomings during decision making exists in non-predefined scenarios, and the decision making process is required to meet the different needs of users in different contextual situations [125]. An ubiquitous, user-friendly and patient-centred mobile DSS has been implemented; it enables patients and their caregivers to apply online for clinical guidelines and obtain semantically integrated electronic health records [119]. Creating systems that facilitate decision making for problems and knowledge sharing among physicians across geographical boundaries and organisations is essential to telehealth [120].
Concerns on triage
Accurate and rapid triaging (assess, sort and count) of individuals who need quick assistance is critical to MCIs [120]. Paper triage tag is inefficient and insufficient because it cannot provide health updates [8]. Major problems, such as the distribution and coordination of available caregiver staff, medical devices and transport services, exist in MCIs. Moreover, alerting potentially essential additional forces becomes complicated because an overview of all available information is not provided to the EEP [132]. Efficient healthcare services cannot be provided when victims outnumber responders. A problem is the automatic tagging of a large number of casualties with various disorders after critical incidents and before the arrival of paramedics [133]. Researchers have suggested the use of wireless sensor tags for pulse monitoring [10, 131]. Supporting triage by continuous monitoring remains a challenge in the planning stages of rescue operation procedures [134].
Concerns on security and privacy
Security and privacy challenges continue to adversely affect the quality of telemedicine systems because of the expanded use of new communication technologies, such as WBAN. Rapid development in network technologies and sensor web enablement (SWE) allowed anytime–anywhere data access for healthcare systems, although several challenges remain with regard to security, privacy and scalability [76, 141]. Secure logging problems in WSN remain an issue [13]. A fully secured mobile phone application that uses public key cryptography is necessary to a computationally efficient overhead. Remote sensors are incapable of pre-sharing because of their restricted computational resources [75]. Moreover, designing a secure and efficient system for MWSNs is a complicated task owing to the high number of security requirements and security mechanisms [74]. However, e-health or mHealth applications in fitness and remote healthcare monitoring, assisted living and disease management (i.e., the X73PHD domains) require features, such as secure connection to mobile aggregators, device sharing across many individuals with privacy and interoperability with certain IHE-compliant healthcare systems [77]. Developing a secure and reliable remote healthcare system is essential to data privacy when a multi-communication network integration technology is used [138].
Concerns on disaster and emergency management
Emergency management for medical WSNs is another challenge in the triage process and general physiological data collection during disasters [98, 122]. In [94], more than 24 academic and commercial body-worn healthcare monitoring systems were analysed and found to have no highly synchronised multi-channel auscultation. A cloud computing system for rural emergency healthcare is required for the reduction of deaths due to time delays during patient transportation and to delayed first aid treatment [146]. Urban search-and-rescue poses important challenges to emergency responders and caregivers, such as search and rescue of individuals, and to building structural assessment and initial medical stabilisation of trapped patients [96]. Challenges with regard to disaster recovery exist in an environment that lacks functional telecommunication services [45, 93]. Problems also exist in tracking and monitoring pilgrims in holy areas, such as Uttrakhand and Mecca. In modern rescue operations, GPS technologies are frequently used for locating an individual but become ineffective when they encounter problems with wireless networks and weather conditions [97].
Concerns on ambient assisted living
The daily living challenges faced by elderly people pose problems for telemedicine systems. One of the major challenges is the need for assistance at home as few people can provide care for their elderly or disabled relatives. Numerous caregivers and organisations offer such assistance [109, 136]. Reducing primary care patient load, enhancing the communication through many healthcare units [80] and encouraging the elderly to stay home have become of great importance in emergent countries owing to economic and societal motivations (support to well-being and autonomy, healthcare and assistance) [108]. Patients with cognitive dysfunction, such as Alzheimer’s disease, are rapidly becoming the main focus of improved healthcare delivery systems [115].
Recommendations
We briefly provide some recommendations from the literature that aim to mitigate the challenges faced by developers, researchers, physicians and patients in the various fields of telemedicine. The recommendations are categorised categorized according to their nature (Fig. 9).
Recommendations to designers/developers
Owing to the development of different systems, designers and developers must follow most of the recommendations to formulate solutions that can assist physicians and patients encountering technical problems regarding the use various medical devices. A queuing prototype that includes various polling schemes and a vast range of new applications related to wireless multimedia sensor networks that ensure QoS for all types of implementations in WBAN must be explored [71, 72]. The optimisation of the EDA-MAC protocol and inclusion of all the access stages refine communication and enable the implementation of IEEE 802.15.6 and LEDA MAC experiments on a large-scale WBAN with multiple sensor knots [12, 61]. The sensitivity of the sensor should be increased for the enhancement of the health monitoring prognostics of the target Xentium processor [52]. Mainstream magnetic and inertial measurement unit (MIMU)-Wear, an extensible ontology-based system that is represented by wearable sensor platforms that comprise mainstream MIMUs, should be improved in terms of weight; such improvements are critical for wearable systems. Locations on the user body could be extended to make them more granular. or Alternatively, the orientation of the MIMU for applications that require precise assessment of the 3D situation of the sensor should be included in the model for applications that require a precise assessment of the 3D situation of the sensor [43]. Data security through encryption with less overhead should be improved and made efficient for multiple patient environments in terms of energy consumption and battery life [64]. The development and design of an advanced and strong editor that addresses multiple file formats should be considered for the expansion of a system’s usability [99], and decision table techniques can be used as bases for the design of complete and consistent MUI context adaptation rules for mobile applications with other user categories [82]. This framework is used as a guide for designers, aiding to aid the min the many complex design decisions, and provides the tools needed to design and implement effective and efficient sensor-based IT solutions in healthcare applications [100]. A secure architecture that enhances cloud computing technology should be used for the distribution of attribute-based encryption multi-healthcare authorities [122]. A convenient and inexpensive BP-detecting technique [9] must be developed. This approach can be applied to many real-world projects, and the feedback and cooperation of hospitals should be obtained. Hidden Markov model can be used for the consolidation of the estimation of bandwidth performance [124]. The following major directions require focus: (1) the development of modern services for monitoring the elderly on the basis of a sensor network infrastructure at home in an ambient and intelligence context and (2) the development of clinical trials in adherence to protocols and the advancement of self-administration [150]. The implementation of the proposed MSHA in an actual application in the entire architecture of wireless healthcare telemonitoring systems [4], and an adequate programme that can facilitate the analytics processes for various healthcare-related complex data sources (e.g. images, streams) are needed [114].
Recommendations to researchers
This section provides recommendations to researchers in this particular field of healthcare. We recommend determining how other services can be added to a priority-dependent compressed data gathering scheme while maintaining integrity to improve the efficiency of the collection of various types of health data is recommended to be investigated [74]. Future studies should cover modern techniques and methods to enhance HANs and facilitate telehealth applications [53]. In this research, we recommend the investigation of the efficiency of optimised congestion management protocol for healthcare WSNs when mobile patients are in the city or in a hospital [56]. Researchers should conduct a pilot test of Jeev to track the inoculation coverage of children in rural Haiti, research its efficiency, and identify socio-cultural issues that must be addressed during large-scale deployment [88]. Researchers should also study a wire-based medical and monitoring environment to derive an enhanced approach that guarantees stable QoS in a dynamic environment [51]. Furthermore, studies should focus on the combined effect of remote management at the patient’s local environment and that of enhanced quality of care, which may result in significant cost savings in the future because of reduced complications, hospitalisations and clinical visits [119]. Researchers should also investigate social factors, including aging population and cost and implications of medical insurance, to improve the effectiveness of remote healthcare monitoring systems [121]. In the health community, the impact of threats on the decision process, particularly those that determine the security flexibility of LCS, should be analysed, and how LCS can be incorporated into other application domains, such as smart home, smart grid and industrial automation, should be studied [123]. Researchers can also study complicated healthcare quality problems to extend their content on research techniques to include mixed techniques research on human factors and ergonomics research on healthcare [17]. The application of the components of the digital health innovation ecosystems conceptual framework in developed and developing countries can also be examined [18]. Other randomised trials of telehealth interventions, the high-quality evaluation of ongoing telehealth services for CVD, and the high-quality evaluation of ongoing telehealth services for CVD are required [27]. Technologies that aid the modern models of person-centric auspices for the self-management of health by older adults, social support and self-reported health measures incorporated into personal health records PHRs, community health registries, and electronic medical records can be examined [40].
Recommendations to physicians/medical organisations
Patients with different types of diseases require recommendations from physicians, who are critical to the treatment and diagnosis of various diseases. RTPS middleware can be used for the integration of diverse medicinal devices in a WAN [47]. The implementation of a priority-based cross-layer routing protocol for healthcare applications in a real WBAN-based environment is required [69], and using a false alarm detection architecture in a healthcare scenario and exploring security issues are also recommended [46]. Meanwhile, the heterogeneity criterion of data for aggregation should be considered. The installation of health data collected from body sensors can be used to make the data more significant and informative for medical professionals [102]. Semantic interoperability issue and argumentative reasoning for explaining medical decisions in research require attention [126]. State-of-the-art machine learning mechanisms, such as cooperative filtering, can be used for data mining on alert outcomes and for the automatic provision of recommendations [137]. Sensors that can monitor vital parameters and send alerts to caregivers and medical emergency teams are needed by people who need constant monitoring, especially patients with Alzheimer’s disease or diabetes [142]. As a scientific approach that supports the assessment and diagnosis of data and medicinal histories from intermediary healthcare workers or community clinics is imperative [142], an electronic triage system should be deployed in EDs, and possible issues that may emerge when the system is incorporated to the triage workflow in a hospital should be determined [8]. Furthermore, exploring practice-centred metrics, as a quantifiable measure, is needed for assessment systems that aid work, cooperation and decision making [128].
Recommendations to patients and users
Many users with different diseases need advice and recommendations that can direct them to follow safe and healthy practices in their daily lives. Users need personalised services, taking into account interoperability requirements and investigating new strategies for information storage, to enrich the relationship between collective knowledge and territorial intelligence by adding new data sources, such as emergent smart sensors [87]. A system presents recommendations for the analysis of collected big data and the transformation of a database into a knowledge base so that patients, researchers and ordinary users can use the system as a beneficial source of information [140]. Web services can be used for uploading sensor data into the cloud, and an optimal scheduling technique that increases service capacity, such as a global standard service, a service interface for sensor data monitoring, sensor tuning and alert notificationcan be created [141]. An IoT-based patient surveillance system is useful in assisting patients with chronic diseases because it enables measurements through sensors and provides advice on workout routines and eating habits [135]. Expanded home experiments can support systems that can revolutionise diabetes care and improve the daily lives of patients with diabetes easier [30].
Conclusion
The number of studies on telemedicine continues to increase. However, these studies have some limitations that remain unaddressed. Telemedicine is an emerging topic that warrants further investigation. The main contribution of this article is a comprehensive survey and classification of works related to the topic. Some Specific patterns in the literature are observed. The retrieved articles are grouped into two categories, namely, telemedicine architecture and review and survey. We comprehensively analysed some articles to highlight the challenges, benefits, and recommendations related to triage and priority-based sensor technology in telemedicine and found some gaps. Several recommendations in handling and controlling these components are provided accordingly. These instructions must be followed by developers, researchers, physicians, and patients in various fields of telemedicine. These recommendations provide future research with solutions to the many challenges that are related to triage and priority-based sensor technology in telemedicine. Most of these challenges are linked to network optimisation, disease monitoring, general healthcare services, healthcare data management, power consumption (or) energy efficiency, DSS, triage, security and privacy, disaster and emergency management and AAL. This review also summarises the ideas presented in the related literature, thereby providing a valuable reference for researchers. Topics related to telemedicine need should be updated.
Contribution
This work contribute to the body of knowledge on the subject. Future researchers could use this taxonomy to extract the gaps in telemedicine.
References
Raikhelkar, J., and Raikhelkar, J. K., The impact of telemedicine in cardiac critical care. Crit. Care Clin. 31(2):305–317, 2015.
Doumbouya, M. B., Kamsu-Foguem, B., Kenfack, H., and Foguem, C., A framework for decision making on teleexpertise with traceability of the reasoning. IRBM 36(1):40–51, 2015.
Hamdi, O., Chalouf, M. A., Ouattara, D., and Krief, F., eHealth: Survey on research projects, comparative study of telemonitoring architectures and main issues. J. Netw. Comput. Appl. 46:100–112, 2014.
Salman, O. H., Rasid, M. F. A., Saripan, M. I., and Subramaniam, S. K., Multi-sources data fusion framework for remote triage prioritization in telehealth. J. Med. Syst. 38(9):103, 2014.
Sene, A., Kamsu-foguem, B., and Rumeau, P., Telemedicine framework using case-based. Comput. Methods Prog. Biomed. 121(1):21–35, 2015.
Rajan, S. P., Review and investigations on future research directions of mobile based telecare system for cardiac surveillance. J. Appl. Res. Technol. Universidad Nacional Autónoma de México, Centro de Ciencias Aplicadas y Desarrollo Tecnológico 13(4):454–460, 2015.
Negra, R., Jemili, I., and Belghith, A., Wireless body area networks: Applications and technologies. Procedia Comput. Sci. 83:1274–1281, 2016.
Niswar, M., et al. The design of wearable medical device for triaging disaster casualties in developing countries. In: 2015 5th International Conference on Digital Information Processing and Communications, ICDIPC 2015, 2015, pp. 207–212.
Moreno, S., Quintero, A., Ochoa, C., Bonfante, M., Villareal, R., and Pestana, J., Remote monitoring system of vital signs for triage and detection of anomalous patient states in the emergency room. In: 2016 XXI Symposium on Signal Processing, Images and Artificial Vision (STSIVA), 2016, pp. 1–5.
Dos Santos, J. R. B., Blard, G., Oliveira, A. S. R., and De Carvalho, N. B., Wireless sensor tag and network for improved clinical triage. In: 2015 Euromicro Conference on Digital System Design, 2015, pp. 399–406.
Gambhir, S., and Kathuria, M., DWBAN: Dynamic priority based WBAN architecture for healthcare system. 2016 3rd International Conference on Computing for Sustainable Global Development (INDIACom), 2016, pp. 3380–3386.
Yuan, X., Li, C., Song, Y., Yang, L., and Ullah, S., On energy-saving in e-healthcare: a directional MAC protocol for WBAN. In: 2015 IEEE Globecom Workshops, GC Wkshps 2015 - Proceedings, 2015.
de la Piedra, A., Braeken, A., Touhafi, A., and Wouters, K., Secure event logging in sensor networks. Comput. Math Appl. 65(5):762–773, 2013.
Rodrigues, E. M. G., Godina, R., Cabrita, C. M. P., and Catalão, J. P. S., Biomedical signal processing and control experimental low cost reflective type oximeter for wearable health systems. Biomed. Signal Process. 31:419–433, 2017.
Ahmadi-javid, A., Seyedi, P., and Syam, S. S., Computers & operations research a survey of healthcare facility location. Comput. Oper. Res. 79:223–263, 2017.
Alaiad, A., and Zhou, L., The determinants of home healthcare robots adoption: An empirical investigation. Int. J. Med. Inform. 83(11):825–840, 2014.
Carayon, P., Kianfar, S., Li, Y., Xie, A., Alyousef, B., and Wooldridge, A., Review article a systematic review of mixed methods research on human factors and ergonomics in health care. Appl. Ergon. 51:291–321, 2015.
Ejehiohen, G., Herselman, M., and Botha, A., Digital health innovation ecosystems: From systematic literature review to conceptual framework. Procedia - Procedia Comput. Sci. 100:244–252, 2016.
Point, C., Accreditation, E., and Benton, D., Health care delivery. J. Nurs. Regul. 7(4):S12–S16, 2017.
Aggidis, A. G. A., Newman, J. D., and Aggidis, G. A., Investigating pipeline and state of the art blood glucose biosensors to formulate next steps. Biosens. Bioelectron. 74:243–262, 2015.
Alberdi, A., Aztiria, A., and Basarab, A., Towards an automatic early stress recognition system for office environments based on multimodal measurements: A review. J. Biomed. Inform. Elsevier Inc 59:49–75, 2016.
Albert, N. M., A systematic review of transitional-care strategies to reduce rehospitalization in patients with heart failure. Hear. Lung. J. Acute Crit. Care 45(2):100–113, 2016.
Brian, R. M., and Ben-Zeev, D., Mobile health (mHealth) for mental health in Asia: Objectives, strategies, and limitations. Asian J. Psychiatr. Elsevier B.V 10(2014):96–100, 2014.
Finet, P., Le Bouquin Jeannès, R., Dameron, O., and Gibaud, B., Review of current telemedicine applications for chronic diseases. Toward a more integrated system? IRBM 36(3):133–157, 2015.
Hu, J. et al., Portable microfluidic and smartphone-based devices for monitoring of cardiovascular diseases at the point of care. Biotechnol. Adv. 34(3):305–320, 2016.
Shore, J. H., Aldag, M., McVeigh, F. L., Hoover, R. L., Ciulla, R., and Fisher, A., Review of mobile health technology for military mental health. Mil. Med. 179(8):865–878, 2014.
Wade, V., and Stocks, N., The use of telehealth to reduce inequalities in cardiovascular outcomes in Australia and New Zealand: A critical review. Hear. Lung. Circ. 26(4):331–337, 2017.
Tripathi, K. M., Kim, T., Losic, D., and Tung, T. T., Recent advances in engineered graphene and composites for detection of volatile organic compounds (VOCs) and non-invasive diseases diagnosis. Carbon N Y 110:97–129, 2016.
Schulmeister, L., Technology and the transformation of oncology care. Semin. Oncol. Nurs. 32(2):99–109, 2016.
Renard, E., Cobelli, C., and Kovatchev, B. P., Closed loop developments to improve glucose control at home. Diabetes Res. Clin. Pract. 102(2):79–85, 2013.
Gross, T. et al., New technologies in emergency medical services for children. Clin. Pediatr. Emerg. Med. 15(1):67–78, 2014.
Sakuragui, R. R. M., Rebelo, M. S., Gutierrez, M. A., Näslund, M., and Håkansson, P., Mobile health in emerging countries: A survey of research initiatives in Brazil. Int. J. Med. Inform. 82(5):283–298, 2013.
Li, H., Zhang, T., Chi, H., Chen, Y., Li, Y., and Wang, J., Mobile health in China: Current status and future development. Asian J. Psychiatr. 10(2014):101–104, 2014.
Silva, B. M. C., Rodrigues, J. J. P. C., de la Torre Díez, I., López-Coronado, M., and Saleem, K., Mobile-health: A review of current state in 2015. J. Biomed. Inform. 56:265–272, 2015.
Adams, Z. W., McClure, E. A., Gray, K. M., Danielson, C. K., Treiber, F. A., and Ruggiero, K. J., Mobile devices for the remote acquisition of physiological and behavioral biomarkers in psychiatric clinical research. J. Psychiatr. Res. 85:1–14, 2017.
Liu, L., Stroulia, E., Nikolaidis, I., Miguel-cruz, A., and Rios, A., Smart homes and home health monitoring technologies for older adults: A systematic review. Int. J. Med. Inform. 91:44–59, 2016.
Obi, T., Ishmatova, D., and Iwasaki, N., Promoting ICT innovations for the ageing population in Japan. Int. J. Med. Inform. 82(4):e47–e62, 2013.
Rantz, M. J. et al., Sensor technology to support aging in place. J. Am. Med. Dir. Assoc. 14(6):386–391, 2013.
Woznowski, P., Kaleshi, D., Oikonomou, G., and Craddock, I., Classification and suitability of sensing technologies for activity recognition. Comput. Commun. 89–90:34–50, 2016.
Reeder, B., Meyer, E., Lazar, A., Chaudhuri, S., Thompson, H. J., and Demiris, G., Framing the evidence for health smart homes and home-based consumer health technologies as a public health intervention for independent aging: A systematic review. Int. J. Med. Inform. 82(7):565–579, 2013.
Phillips, S. A., Martino, S., and Arena, R., Research opportunities and challenges in the era of healthy living medicine: Unlocking the potential. Prog. Cardiovasc. Dis. 59(5):498–505, 2017.
Bradai, N., Charfi, E., Fourati, L. C., and Kamoun, L., Priority consideration in inter-WBAN data scheduling and aggregation for monitoring systems. Trans. Emerg. Telecommun. Technol. 27(4):589–600, 2016.
Villalonga, C., Pomares, H., Rojas, I., and Banos, O., MIMU-wear: Ontology-based sensor selection for real-world wearable activity recognition. Neurocomputing 250(2017):76–100, 2017.
Ghanavati, S., Abawaji, J., and Izadi, D., A congestion control scheme based on fuzzy logic in wireless body area networks. In: 2015 I.E. 14th International Symposium on Network Computing and Applications, 2015, pp. 235–242.
Ghanavati, S., Abawajy, J., and Izadi, D., ECG rate control scheme in pervasive health care monitoring system. In: 2016 I.E. International Conference on Fuzzy Systems (FUZZ-IEEE), 2016, pp. 2265–2270.
Haque, S. A., and Aziz, S. M., False alarm detection in cyber-physical systems for healthcare applications. AASRI Procedia 5:54–61, 2013.
Almadani, B., Saeed, B., and Alroubaiy, A., Healthcare systems integration using Real Time Publish Subscribe (RTPS) middleware. Comput. Electr. Eng. 50:67–78, 2016.
Ben Elhadj, H., Elias, J., Chaari, L., and Kamoun, L., Multi-attribute decision making handover algorithm for wireless body area networks. Comput. Commun. 81:97–108, 2016.
Bradai, N., Fourati, L. C., and Kamoun, L., Ad hoc networks WBAN data scheduling and aggregation under WBAN / WLAN healthcare network. 25:251–262, 2015.
Gündoğdu, K., and Çalhan, A., An implementation of wireless body area networks for improving priority data transmission delay. J. Med. Syst. 40(3):75, 2016.
Kim, R. H., Kim, P. S., and Kim, J. G., An effect of delay reduced MAC protocol for WBAN based medical signal monitoring. In: 2015 I.E. Pacific Rim Conference on Communications, Computers and Signal Processing (PACRIM), 2015, vol. 2015–Novem, pp. 434–437.
Zhao, Y., and Kerkhoff, H. G., Design of an embedded health monitoring infrastructure for accessing multi-processor SoC degradation. In: 2014 17th Euromicro Conference on Digital System Design, 2014, pp. 154–160.
Shah, M. A., Kim, J., Khadra, M. H., and Feng, D., Home area network for optimizing telehealth services- empirical simulation analysis. 36th Annu. Int. Conf. IEEE Eng. Med. Biol. Soc., 2014, pp. 1370–1373.
Rezvani, S., and Ghorashi, S. A., Context aware and channel-based resource allocation for wireless body area networks. IET Wirel. Sens. Syst. 3(1):16–25, 2013.
Ren, J., Wu, G., Li, X., Pirozmand, P., and Obaidat, M. S., Probabilistic response-time analysis for real-time systems in body area sensor networks. 2145–2166, 2015.
Rezaee, A. A., Yaghmaee, M. H., and Rahmani, A. M., Optimized congestion management protocol for healthcare wireless sensor networks. Wirel. Pers. Commun. 75(1):11–34, 2014.
Rezaee, A. A., Yaghmaee, M. H., Rahmani, A. M., and Mohajerzadeh, A. H., HOCA: Healthcare aware optimized congestion avoidance and control protocol for wireless sensor networks. J. Netw. Comput. Appl. 37(1):216–228, 2014.
Kaur, J., Saini, K. S., and Grewal, R., Priority based congestion avoidance hybrid scheme for wireless sensor network. In: 2015 1st International Conference on Next Generation Computing Technologies (NGCT), 2015, pp. 158–165.
Al Mamoon, I., Muzahidul-Islam, A. K. M., Baharun, S., Komaki, S., and Ahmed, A., Architecture and communication protocols for cognitive radio network enabled hospital. In: 2015 9th International Symposium on Medical Information and Communication Technology (ISMICT), 2015, vol. 2015–May, pp. 170–174.
Lin, D., Labeau, F., Yao, Y., Vasilakos, A. V., and Tang, Y., Admission control over internet of vehicles attached with medical sensors for ubiquitous healthcare applications. IEEE J. Biomed. Heal. Informatics 20(4):1195–1204, 2016.
Li, C., Yuan, X., Yang, L., and Song, Y., A hybrid lifetime extended directional approach for WBANs. Sensors 15(12):28005–28030, 2015.
Hwang, T. H., Kim, D. S., and Kim, J. G., An on-time power-aware scheduling scheme for medical sensor SoC-based WBAN systems. Sensors (Switzerland) 13(1):375–392, 2013.
Li, N., Lin, K., Yong, S., Chen, X., Wang, X., and Zhang, X., Design and implementation of a MAC protocol for a wearable monitoring system on human body. In: 2015 I.E. 11th International Conference on ASIC (ASICON), 2015, pp. 1–4.
Sudha, G. F., Karthik, S., and Kumar, N. S., Activity aware energy efficient priority based multi patient monitoring adaptive system for body sensor networks. Technol. Health Care 22(2):167–177, 2014.
Kong, R., Chen, C., Yu, W., Yang, B., and Guan, X., Data priority based slot allocation for wireless body area networks. In: 2013 International Conference on Wireless Communications and Signal Processing, 2013, pp. 1–6.
Misra, S., and Sarkar, S., Priority-based time-slot allocation in wireless body area networks during medical emergency situations: An evolutionary game-theoretic perspective. IEEE J. Biomed. Heal. Informatics 19(2):541–548, 2015.
Puri, T., Challa, R. K., and Sehgal, N. K., Energy efficient QoS aware MAC layer time slot allocation scheme for WBASN. In: 2015 International Conference on Advances in Computing, Communications and Informatics (ICACCI), 2015, pp. 966–972.
Chiang, H., Lai, C., and Huang, Y., A green cloud-assisted health monitoring service on wireless body area networks. Inf. Sci. (Ny) 284:118–129, 2014.
Ben Elhadj, H., Elias, J., Chaari, L., and Kamoun, L., A priority based cross layer routing protocol for healthcare applications. Ad Hoc Netw. 42:1–18, 2016.
Hu, L., Zhang, Y., Feng, D., Hassan, M. M., Alelaiwi, A., and Alamri, A., Design of QoS-aware multi-level MAC-layer for wireless body area network. J. Med. Syst. 39(12):192, 2015.
Iftikhar, M., and Ahmad, I., A novel analytical model for provisioning QoS in body area sensor networks. Procedia Comput. Sci. 32:900–907, 2014.
Iftikhar, M., Al Elaiwi, N., and Aksoy, M. S., Performance analysis of priority queuing model for low power Wireless Body Area Networks (WBANs). Procedia Comput. Sci. 34:518–525, 2014.
Sevin, A., Bayilmis, C., and Kirbas, I., Design and implementation of a new quality of service-aware cross-layer medium access protocol for wireless body area networks. Comput. Electr. Eng. 56:145–156, 2016.
Perera, C., Zaslavsky, A., Christen, P., and Georgakopoulos, D., Sensing as a service model for smart cities supported by internet of things. Trans. Emerg. Telecommun. Technol. 25(1):81–93, 2014.
Baehr, D., McKinney, S., Quirk, A., and Harfoush, K., On the practicality of elliptic curve cryptography for medical sensor networks. In: 2014 11th Annual High Capacity Optical Networks and Emerging/Enabling Technologies (Photonics for Energy), 2014, pp. 41–45.
Hedin, D. S., Kollmann, D. T., Gibson, P. L., Riehle, T. H., and Seifert, G. J., Distance bounded energy detecting ultra-wideband impulse radio secure protocol. In: 2014 36th Annual International Conference of the IEEE Engineering in Medicine and Biology Society, 2014, vol. 2014, pp. 6619–6622.
Rubio, Ó. J., Trigo, J. D., Alesanco, Á., Serrano, L., and García, J., Analysis of ISO/IEEE 11073 built-in security and its potential IHE-based extensibility. J. Biomed. Inform. 60:270–285, 2016.
Benmansour, T., Ahmed, T., and Moussaoui, S., Performance evaluation of IEEE 802.15.6 MAC in monitoring of a cardiac patient. In: 2016 I.E. 41st Conference on Local Computer Networks Workshops (LCN Workshops), 2016, pp. 241–247.
Fourati, H., Idoudi, H., Val, T., Van Den Bossche, A., and Saidane, L. A., Performance evaluation of IEEE 802.15.6 CSMA/CA-based CANet WBAN. In: 2015 IEEE/ACS 12th International Conference of Computer Systems and Applications (AICCSA), 2015, pp. 1–7.
Radhakrishnan, S., Duvvuru, A., and Kamarthi, S. V., Investigating discrete event simulation method to assess the effectiveness of wearable health monitoring devices. Procedia Econ. Financ. 11(14):838–856, 2014.
Meizoso, J. P. et al., Evaluation of miniature wireless vital signs monitor in a trauma intensive care unit. Mil. Med. 181(5S):199–204, 2016.
Alnanih, R., Ormandjieva, O., and Radhakrishnan, T., Context-based and rule-based adaptation of mobile user interfaces in mHealth. Procedia Comput. Sci. 21:390–397, 2013.
Fratini, A., and Caleffi, M., Medical emergency alarm dissemination in urban environments. Telemat. Informatics 31(3):511–517, 2014.
Boursalie, O., Samavi, R., and Doyle, T. E., M4CVD: Mobile machine learning model for monitoring cardiovascular disease. Procedia Comput. Sci 63(Icth):384–391, 2015.
Fezari, M., Rasras, R., and El Emary, I. M. M., Ambulatory health monitoring system using wireless sensors node. Procedia Comput. Sci 65(Iccmit):86–94, 2015.
Villarreal, V., Fontecha, J., Hervas, R., and Bravo, J., Mobile and ubiquitous architecture for the medical control of chronic diseases through the use of intelligent devices: Using the architecture for patients with diabetes. Futur. Gener. Comput. Syst. 34:161–175, 2014.
Sebillo, M., Tortora, G., Tucci, M., Vitiello, G., Ginige, A., and Di Giovanni, P., Combining personal diaries with territorial intelligence to empower diabetic patients. J. Vis. Lang. Comput. 29:1–14, 2015.
Katib, A., Rao, D., Rao, P., Williams, K., and Grant, J., A prototype of a novel cell phone application for tracking the vaccination coverage of children in rural communities. Comput. Methods Prog. Biomed. 122(2):215–228, 2015.
Lwin, M. O. et al., A 21st century approach to tackling dengue: Crowdsourced surveillance, predictive mapping and tailored communication. Acta Trop. 130:100–107, 2014.
Bresó, A., Martínez-Miranda, J., Fuster-García, E., and García-Gómez, J. M., A novel approach to improve the planning of adaptive and interactive sessions for the treatment of major depression. Int. J. Hum. Comput. Stud. 87:80–91, 2016.
Chakraborty, S., Ghosh, S. K., Jamthe, A., and Agrawal, D. P., Detecting mobility for monitoring patients with parkinson’s disease at home using RSSI in a wireless sensor network. Procedia Comput. Sci. 19:956–961, 2013.
Hermens, H., op den Akker, H., Tabak, M., Wijsman, J., and Vollenbroek, M., Personalized coaching systems to support healthy behavior in people with chronic conditions. J. Electromyogr. Kinesiol. 24(6):815–826, 2014.
Adibi, S., A mobile health network disaster management system. In: 2015 Seventh International Conference on Ubiquitous and Future Networks, 2015, pp. 424–428.
Beck, C., and Georgiou, J., A wearable, multimodal, vitals acquisition unit for intelligent field triage. In: 2016 I.E. International Symposium on Circuits and Systems (ISCAS), 2016, vol. 2016–July, pp. 1530–1533.
Besaleva, L. I., and Weaver, A. C., Mobile electronic triaging for emergency response improvement through crowdsourced and sensor-detected information. In: Proceedings of the 2013 IEEE/ACM International Conference on Advances in Social Networks Analysis and Mining - ASONAM ‘13, 2013, pp. 1092–1093.
Ganz, A., Schafer, J. M., Tang, J., Yang, Z., Yi, J., and Ciottone, G., Urban search and rescue situational awareness using DIORAMA disaster management system. Procedia Eng. 107:349–356, 2015.
Gunasekaran, S., and Suresh, M., A novel control of disaster protection (NCDP) for pilgrims by pan technology. In: 2014 I.E. 8th International Conference on Intelligent Systems and Control (ISCO), 2014, pp. 103–107.
Renner, A., et al., RIPPLE: Scalable medical telemetry system for supporting combat rescue. In: NAECON 2014 - IEEE National Aerospace and Electronics Conference, 2014, vol. 2015–Febru, pp. 228–232.
Ali, R. et al., GUDM: Automatic generation of unified datasets for learning and reasoning in healthcare. Sensors 15(12):15772–15798, 2015.
Gaynor, M., and Waterman, J., Design framework for sensors and RFID tags with healthcare applications. Heal. Policy Technol. 5(4):357–369, 2016.
Kim, H.-K., Convergence agent model for developing u-healthcare systems. Futur. Gener. Comput. Syst. 35:39–48, 2014.
Misra, S., and Chatterjee, S., Social choice considerations in cloud-assisted WBAN architecture for post-disaster healthcare: Data aggregation and channelization. Inf. Sci. (Ny) 284:95–117, 2014.
Zhang, K., Liang, X., Baura, M., Lu, R., and Shen, (Sherman) X., PHDA: A priority based health data aggregation with privacy preservation for cloud assisted WBANs. Inf. Sci. (Ny). 284:130–141, 2014.
Yi, C., Zhao, Z., Cai, J., Lobato de Faria, R., and Zhang, (Michael) G., Priority-aware pricing-based capacity sharing scheme for beyond-wireless body area networks. Comput. Netw. 98:29–43, 2016.
Yi, C., Alfa, A. S., and Cai, J., An incentive-compatible mechanism for transmission scheduling of delay-sensitive medical packets in e-Health networks. IEEE Trans. Mob. Comput. 15(10):2424–2436, 2016.
Yi, Z., et al., Emergency treatment in smart terminal-based e-healthcare networks. In: 2015 4th International Conference on Computer Science and Network Technology (ICCSNT), 2015, no. Iccsnt, pp. 1178–1181.
Sneha, S., and Varshney, U., A framework for enabling patient monitoring via mobile ad hoc network. Decis. Support. Syst. 55(1):218–234, 2013.
Bouakaz, S. et al., CIRDO: Smart companion for helping elderly to live at home for longer. IRBM 35(2):100–108, 2014.
De Backere, F., Bonte, P., Verstichel, S., Ongenae, F., and De Turck, F., The OCarePlatform: A context-aware system to support independent living. Comput. Methods Prog. Biomed. 140:111–120, 2017.
Kormanyos, B., and Pataki, B., Multilevel simulation of daily activities: Why and how? In: 2013 I.E. International Conference on Computational Intelligence and Virtual Environments for Measurement Systems and Applications (CIVEMSA), 2013, pp. 1–6.
Rahmani, A. M. et al., Exploiting smart e-Health gateways at the edge of healthcare Internet-of-Things: A fog computing approach. Futur. Gener. Comput. Syst. 78:641–658, 2017.
Varshney, U., A model for improving quality of decisions in mobile health. Decis. Support. Syst. 62:66–77, 2014.
Minutolo, A., Esposito, M., and De Pietro, G., Design and validation of a light-weight reasoning system to support remote health monitoring applications. Eng. Appl. Artif. Intell. 41:232–248, 2015.
Sakr, S., and Elgammal, A., Towards a comprehensive data analytics framework for smart healthcare services. Big Data Res. 4:44–58, 2016.
Moutacalli, M. T., Marmen, V., Bouzouane, A., and Bouchard, B., Activity pattern mining using temporal relationships in a smart home. In: 2013 I.E. Symposium on Computational Intelligence in Healthcare and e-health (CICARE), 2013, pp. 83–87.
Bharatula, S., and Meenakshi, M., Design of cognitive radio network for hospital management system. Wirel. Pers. Commun. 90(2):1021–1038, 2016.
Vaidehi, V., Vardhini, M., Yogeshwaran, H., Inbasagar, G., Bhargavi, R., and Hemalatha, C. S., Agent based health monitoring of elderly people in indoor environments using wireless sensor networks. Procedia Comput. Sci 19(Ant):64–71, 2013.
Ben Othman, S., Zgaya, H., Hammadi, S., Quilliot, A., Martinot, A., and Renard, J., Agents endowed with uncertainty management behaviors to solve a multiskill healthcare task scheduling. J. Biomed. Inform. 64:25–43, 2016.
Peleg, M. et al., Assessment of a personalized and distributed patient guidance system. Int. J. Med. Inform. 101:108–130, 2017.
Tawfik, H., and Anya, O., Evaluating practice-centered awareness in cross-boundary telehealth decision support systems. Telemat. Informatics 32(3):486–503, 2015.
Tamura, T. et al., Assessment of participant compliance with a Web-based home healthcare system for promoting specific health checkups. Biocybern. Biomed. Eng. 34(1):63–69, 2014.
Lounis, A., Hadjidj, A., Bouabdallah, A., and Challal, Y., Healing on the cloud: Secure cloud architecture for medical wireless sensor networks. Futur. Gener. Comput. Syst. 55:266–277, 2016.
Saleem, K., Derhab, A., Al-Muhtadi, J., and Shahzad, B., Human-oriented design of secure machine-to-machine communication system for e-Healthcare society. Comput. Hum. Behav. 51:977–985, 2015.
Wang, J., Qiu, M., and Guo, B., Enabling real-time information service on telehealth system over cloud-based big data platform. J. Syst. Archit. 72:69–79, 2017.
Nageba, E., Rubel, P., and Fayn, J., Towards an intelligent exploitation of heterogeneous and distributed resources in cooperative environments of eHealth. IRBM 34(1):79–85, 2013.
Doumbouya, M. B., Kamsu-Foguem, B., Kenfack, H., and Foguem, C., Telemedicine using mobile telecommunication: Towards syntactic interoperability in teleexpertise. Telemat. Informatics 31(4):648–659, 2014.
Urovi, V., Jimenez-del-Toro, O., Dubosson, F., Ruiz Torres, A., and Schumacher, M. I., COMPOSE: Using temporal patterns for interpreting wearable sensor data with computer interpretable guidelines. Comput. Biol. Med. 81:24–31, 2017.
Tegegne, T., and van der Weide, (Theo) T. P., Enriching queries with user preferences in healthcare. Inf. Process. Manag.. 50(4):599–620, 2014.
Ganapathy, K., Vaidehi, V., Kannan, B., and Murugan, H., Hierarchical particle swarm optimization with ortho-cyclic circles. Expert Syst. Appl. 41(7):3460–3476, 2014.
Hindia, M. N., Rahman, T. A., Ojukwu, H., Hanafi, E. B., and Fattouh, A., Enabling remote health-caring utilizing iot concept over LTE-femtocell networks. PLoS One 11(5):e0155077, 2016.
Niswar, M., et al., Performance evaluation of ZigBee-based wireless sensor network for monitoring patients’ pulse status. In: 2013 International Conference on Information Technology and Electrical Engineering (ICITEE), 2013, pp. 291–294.
Paulus, A., Meisen, P., Meisen, T., Jeschke, S., Czaplik, M., and Hirsch, F., AUDIME: Augmented disaster medicine. In: 2015 17th International Conference on E-health Networking, Application & Services (HealthCom), 2015, pp. 342–345.
Ullah, F., Khelil, A., Sheikh, A. A., Felemban, E., and Bojan, H. M. A., Towards automated self-tagging in emergency health cases. In: 2013 I.E. 15th International Conference on e-Health Networking, Applications and Services (Healthcom 2013), 2013, no. Healthcom, pp. 658–663.
Rodriguez, D., Heuer, S., Guerra, A., Stork, W., Weber, B., and Eichler, M., Towards automatic sensor-based triage for individual remote monitoring during mass casualty incidents. In: 2014 I.E. International Conference on Bioinformatics and Biomedicine (BIBM), 2014, pp. 544–551.
Gómez, J., Oviedo, B., and Zhuma, E., Patient monitoring system based on internet of things. Procedia Comput. Sci 83(Ant):90–97, 2016.
Hussain, A., Wenbi, R., da Silva, A. L., Nadher, M., and Mudhish, M., Health and emergency-care platform for the elderly and disabled people in the Smart City. J. Syst. Softw. 110:253–263, 2015.
Lamprinakos, G. C. et al., An integrated remote monitoring platform towards Telehealth and Telecare services interoperability. Inf. Sci. (Ny) 308:23–37, 2015.
Sung, W., and Chang, K., Health parameter monitoring via a novel wireless system. Appl. Soft Comput. 22:667–680, 2014.
Mendes, J., Simões, H., Rosa, P., Costa, N., Rabadão, C., and Pereira, A., Secure low-cost solution for elder’s eCardio surveillance. Procedia Comput. Sci 27(Dsai 2013):46–56, 2014.
Zanjal, S. V., and Talmale, G. R., Medicine reminder and monitoring system for secure health using IOT. Procedia Comput. Sci. 78(3):471–476, 2016.
Ganapathy, K., Priya, B., Priya, B., Dhivya, Prashanth, V., and Vaidehi, V., SOA Framework for geriatric remote health care using wireless sensor network. Procedia Comput. Sci 19(Fams):1012–1019, 2013.
Miah, S. J., Hasan, J., and Gammack, J. G., On-cloud healthcare clinic: An e-health consultancy approach for remote communities in a developing country. Telemat. Informatics 34(1):311–322, 2017.
Moore, P., Thomas, A., Qassem, T., Bessis, N., and Hu, B., Monitoring patients with mental disorders. In: 2015 9th International Conference on Innovative Mobile and Internet Services in Ubiquitous Computing, 2015, pp. 65–70.
Traverso, G. et al., Physiologic status monitoring via the gastrointestinal tract. PLoS One 10(11):e0141666, 2015.
Kovalchuk, S. V., Krotov, E., Smirnov, P. A., Nasonov, D. A., and Yakovlev, A. N., Distributed data-driven platform for urgent decision making in cardiological ambulance control. Futur. Gener. Comput. Syst. 79:144–154, 2016.
Rajkumar, R., and Sriman Narayana Iyengar, N. C., Dynamic integration of mobile JXTA with cloud computing for emergency rural public health care. Osong Public Heal Res Perspect 4(5):255–264, 2013.
Kumar, N., Kaur, K., Jindal, A., and Rodrigues, J. J. P. C., Providing healthcare services on-the-fly using multi-player cooperation game theory in Internet of Vehicles (IoV) environment. Digit Commun. Networks 1(3):191–203, 2015.
Moretti, S., Cicalò, S., Mazzotti, M., Tralli, V., and Chiani, M., Content/context-aware multiple camera selection and video adaptation for the support of m-Health services. Procedia Comput. Sci. 40:206–213, 2014.
Calyam, P. et al., Synchronous big data analytics for personalized and remote physical therapy. Pervasive Mob. Comput. 28:3–20, 2016.
Teijeiro, T., Félix, P., Presedo, J., and Zamarrón, C., An open platform for the protocolization of home medical supervision. Expert Syst. Appl. 40(7):2607–2614, 2013.
Funding
This study was funded by UPSI grant No: 2017–0179–109-01.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
This article is part of the Topical Collection on Systems-Level Quality Improvement
Rights and permissions
About this article
Cite this article
Albahri, O.S., Albahri, A.S., Mohammed, K.I. et al. Systematic Review of Real-time Remote Health Monitoring System in Triage and Priority-Based Sensor Technology: Taxonomy, Open Challenges, Motivation and Recommendations. J Med Syst 42, 80 (2018). https://doi.org/10.1007/s10916-018-0943-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10916-018-0943-4