Abstract
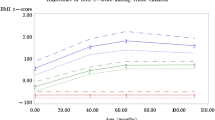
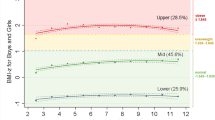
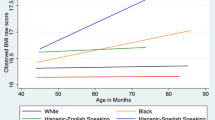
A large body of research has documented racial/ethnic disparities in childhood obesity in the United States (US) but less work has sought to understand differences within racial groups. Longitudinal studies are needed to describe BMI trajectories across development, particularly for Black children from immigrant families who have been underrepresented in childhood obesity research. The current study utilizes BMI data collected longitudinally from ages 5 to 8 years and growth mixture modeling to (1) identify and visualize growth patterns among Black children from primarily Caribbean immigrant families, and (2) to compare these patterns to growth trajectories among Black children from US-born families. First, we identified four classes or trajectories of growth for Black children from immigrant families. The largest trajectory (70% of the sample) maintained non-overweight throughout the study period. A second trajectory developed overweight by age 8 (25%). Two small trajectory groups demonstrated high rates of moderate and severe obesity–i.e., specifically, a trajectory of accelerated weight gain ending in moderate/severe obesity (3%), and a trajectory of early severe obesity with BMI decreasing slightly with age (2%). We identified a very similar four class/trajectory model among Black children from US-born families, and compared the model to the one for children from immigrant families using multi-group growth mixture modeling. We found that the patterns of growth did not differ significantly between the populations, with two notable exceptions. Among Black children from immigrant families, ∼ 5% were classified into the two heavier BMI trajectories, compared to ∼ 11% of children from US-born families. Additionally, among children with an accelerated weight gain trajectory, children from immigrant families had lower BMIs on average at each time point than children from US-born families. These findings describe the multiple trajectories of weight gain among Black children from immigrant families and demonstrate that although these trajectories are largely similar to those of Black children from US-born families, the differences provide some evidence for lower obesity risk among Black children from immigrant families compared to Black children from US-born families. As this study is the first to describe BMI trajectories for Black children from immigrant families across early and middle childhood, future work is needed to replicate these results and to explore differences in heavier weight trajectories between children from immigrant and US-born families.

Similar content being viewed by others
Data Availability
The datasets generated during and/or analyzed during the current study cannot be shared by the study authors. Requests for data would need to be made directly to the NYC Department of Education (DOE).
Code Availability
Analysis code is available upon reasonable request.
References
Isong IA, Richmond T, Avendano M, Kawachi I. Racial/Ethnic disparities: a longitudinal study of growth trajectories among US Kindergarten Children. J Racial Ethn Health Disparities. 2018;5(4):875–84. https://doi.org/10.1007/s40615-017-0434-1.
Anderson SE, Whitaker RC. Prevalence of obesity among US preschool children in different racial and ethnic groups. Arch Pediatr Adolesc Med. 2009;163(4):344–8. https://doi.org/10.1001/archpediatrics.2009.18.
Min J, Wen X, Xue H, Wang Y. Ethnic disparities in childhood BMI trajectories and obesity and potential causes among 29,250 US children: findings from the early childhood longitudinal study-birth and kindergarten cohorts. Int J Obes (Lond). 2018;42(9):1661–70. https://doi.org/10.1038/s41366-018-0091-4.
Skinner AC, Ravanbakht SN, Skelton JA, Perrin EM, Armstrong SC. Prevalence of obesity and severe obesity in US children, 1999–2016. Pediatrics. 2018;141(3). https://doi.org/10.1542/peds.2017-3459.
Baker EH, Rendall MS, Weden MM. Epidemiological Paradox or immigrant vulnerability? Obesity among Young Children of immigrants. Demography. 2015;52(4):1295–320. https://doi.org/10.1007/s13524-015-0404-3.
Messiah SE, Atem F, Lebron C, Ofori A, Mathew MS, Chang C, et al. Comparison of early life obesity-related risk and protective factors in non-hispanic black subgroups. Matern Child Health J. 2020;24(9):1130–7. https://doi.org/10.1007/s10995-020-02979-3.
Crosby DA, Dunbar AS. Patterns and predictors of school readiness and early childhood success among young children in black immigrant families. Washington, DC: Migration Policy Institute. 2012. https://www.migrationpolicy.org/research/patterns-and-predictors-school-readiness-and-early-childhood-success-among-young-children. Accessed 20 March 2023.
Singh GK, Kogan MD, Yu SM. Disparities in obesity and overweight prevalence among US immigrant children and adolescents by generational status. J Community Health. 2009;34(4):271–81. https://doi.org/10.1007/s10900-009-9148-6.
Van Hook J, Balistreri KS, Baker E. Moving to the Land of Milk and cookies: obesity among the children of immigrants. Migration Inform Source. 2009.
Mattsson M, Maher GM, Boland F, Fitzgerald AP, Murray DM, Biesma R. Group-based trajectory modelling for BMI trajectories in childhood: a systematic review. Obes Rev. 2019;20(7):998–1015. https://doi.org/10.1111/obr.12842.
Rollins BY, Francis LA. Off the Charts: Identifying and Visualizing Body Mass Index Trajectories of Rural, Poor Youth. J Pediatr. 2021;228. https://doi.org/10.1016/j.jpeds.2020.09.007. :147 – 54 e2.
Van Hook J, Baker E. Big boys and little girls: gender, acculturation, and weight among young children of immigrants. J Health Soc Behav. 2010;51(2):200–14. https://doi.org/10.1177/0022146510372347.
Carter RC. The impact of public schools on childhood obesity. JAMA. 2002;288(17):2180. https://doi.org/10.1001/jama.288.17.2180-JMS1106-6-1.
Fried EJ, Nestle M. The growing political movement against soft drinks in schools. JAMA. 2002;288(17):2181. https://doi.org/10.1001/jama.288.17.2181-JMS1106-7-1.
Solomons NW. Diet and long-term health: an African diaspora perspective. Asia Pac J Clin Nutr. 2003;12(3):313–30.
Misra A, Ganda OP. Migration and its impact on adiposity and type 2 diabetes. Nutrition. 2007;23(9):696–708. https://doi.org/10.1016/j.nut.2007.06.008.
Ifatunji MA, Faustin Y, Lee W, Wallace D. Black Nativity and Health disparities: a Research paradigm for understanding the Social Determinants of Health. Int J Environ Res Public Health. 2022;19(15). https://doi.org/10.3390/ijerph19159166.
Bennett GG, Wolin KY, Askew S, Fletcher R, Emmons KM. Immigration and obesity among lower income blacks. Obes (Silver Spring). 2007;15(6):1391–4. https://doi.org/10.1038/oby.2007.166.
Hamilton E, Cardoso JB, Hummer RA, Padilla YC. Assimilation and emerging health disparities among new generations of U.S. children. Demographic Res. 2011;25(25):783–818. https://doi.org/10.4054/DemRes.2011.25.25.
Li C, Goran MI, Kaur H, Nollen N, Ahluwalia JS. Developmental trajectories of overweight during childhood: role of early life factors. Obes (Silver Spring). 2007;15(3):760–71. https://doi.org/10.1038/oby.2007.585.
Brotman LM, Dawson-McClure S, Calzada EJ, Huang KY, Kamboukos D, Palamar JJ, et al. Cluster (school) RCT of ParentCorps: impact on kindergarten academic achievement. Pediatrics. 2013;131(5):e1521–9. https://doi.org/10.1542/peds.2012-2632.
Brotman LM, Dawson-McClure S, Kamboukos D, Huang K-Y, Calzada EJ, Goldfeld K, et al. Effects of ParentCorps in prekindergarten on child mental health and academic performance: follow-up of a randomized clinical trial through 8 years of age. JAMA Pediatr. 2016;170(12):1149–55. https://doi.org/10.1001/jamapediatrics.2016.1891.
Borjas GJ. Poverty and program participation among immigrant children. Future Child. 2011;21(1):247–66. https://doi.org/10.1353/foc.2011.0006.
Ursache A, Kiely Gouley K, Dawson-McClure S, Barajas-Gonzalez RG, Calzada EJ, Goldfeld KS, et al. Early emotion knowledge and later academic achievement among children of Color in historically disinvested neighborhoods. Child Dev. 2020;91(6):e1249–66. https://doi.org/10.1111/cdev.13432.
Centers for Disease Control and Prevention (CDC). Defining Childhood Weight Status. Centers for Disease Control and Prevention 2022. Updated 14 December 2022. https://www.cdc.gov/obesity/basics/childhood-defining.html. Accessed 20 March 2023.
Muthén L, Muthén B. Mplus user’s guide (version 8.0). Mplus user’s guide. 2017:1-950.
Jung T, Wickrama KAS. An introduction to latent class growth analysis and growth mixture modeling. Soc Pers Psychol Compass. 2008;2(1):302–17. https://doi.org/10.1111/j.1751-9004.2007.00054.x.
Berkey CS, Colditz GA. Adiposity in adolescents: change in actual BMI works better than change in BMI z score for longitudinal studies. Ann Epidemiol. 2007;17(1):44–50. https://doi.org/10.1016/j.annepidem.2006.07.014.
Cole TJ, Faith MS, Pietrobelli A, Heo M. What is the best measure of adiposity change in growing children: BMI, BMI %, BMI z-score or BMI centile? Eur J Clin Nutr. 2005;59(3):419–25. https://doi.org/10.1038/sj.ejcn.1602090.
Kass RE, Raftery AE. Bayes Factors. J Am Stat Assoc. 1995;90(430):773–95. https://doi.org/10.1080/01621459.1995.10476572.
Schwarz G. Estimating the dimension of a model. Ann Stat. 1978;6(2):461–4. https://doi.org/10.1214/aos/1176344136.
Sterne JA, White IR, Carlin JB, Spratt M, Royston P, Kenward MG, et al. Multiple imputation for missing data in epidemiological and clinical research: potential and pitfalls. BMJ. 2009;338:b2393. https://doi.org/10.1136/bmj.b2393.
Francis LA, Rollins BY, Bryce CI, Granger DA. Biobehavioral Dysregulation and its Association with obesity and severe obesity trajectories from 2 to 15 years of age: a longitudinal study. Obes (Silver Spring). 2020;28(4):830–9. https://doi.org/10.1002/oby.22762.
Hudda MT, Nightingale CM, Donin AS, Fewtrell MS, Haroun D, Lum S, et al. Body mass index adjustments to increase the validity of body fatness assessment in UK Black African and south Asian children. Int J Obes (Lond). 2017;41(7):1048–55. https://doi.org/10.1038/ijo.2017.75.
Stern C. Why BMI is a flawed health standard, especially for people of color. The Washington Post. 2021. https://www.washingtonpost.com/lifestyle/wellness/healthy-bmi-obesity-race-/2021/05/04/655390f0-ad0d-11eb-acd3-24b44a57093a_story.html. Accessed 20 March 2023.
Brotman LM, Dawson-McClure S, Huang KY, Theise R, Kamboukos D, Wang J, et al. Early childhood family intervention and long-term obesity prevention among high-risk minority youth. Pediatrics. 2012;129(3):e621–8. https://doi.org/10.1542/peds.2011-1568.
Acknowledgements
We would like to express our deep gratitude to the schools and families who participated in the study.
Funding
Supported by US Department of Education, Institute of Education Sciences Grant R305F050245 and by the National Institute of Mental Health grant R01 MH077331-04 to the senior (last) author and by the National Heart, Lung, and Blood Institute grant K01HL138114 to the first author. Funding sources were not involved in the study design or in the decision to submit the article for publication. The content is solely the responsibility of the authors and does not necessarily represent the official views of the funders.
Author information
Authors and Affiliations
Contributions
AU- conceptualization, writing-original draft preparation. BR- conceptualization, formal analysis, writing- review & editing. AC- conceptualization, writing- review & editing. SDM- conceptualization, supervision. LMB- conceptualization, resources, supervision, writing- review & editing. All authors approved the final manuscript.
Corresponding author
Ethics declarations
Ethics Approval
Approval was granted by the institutional review boards of New York University School of Medicine and the NYC Department of Education (DOE). The procedures used in this study adhere to the tenets of the Declaration of Helsinki.
Consent to Participate
Written informed consent for child and parent participation in this study was obtained from parents.
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ursache, A., Rollins, B.Y., Chung, A. et al. BMI Growth Profiles Among Black Children from Immigrant and US-Born Families. J Immigrant Minority Health (2024). https://doi.org/10.1007/s10903-024-01596-4
Accepted:
Published:
DOI: https://doi.org/10.1007/s10903-024-01596-4