Abstract
Background
Ecuador is a major host country for Colombians fleeing violence and Venezuelans escaping a complex humanitarian crisis, many of whom are pregnant women.
Methods
We used national birth registry data (2018–2020) to compare the maternal care and infant outcomes of Venezuelan and Colombian immigrants with Ecuadorian nationals.
Results
Venezuelan immigrants had a lower adjusted odds (AOR) for adequate prenatal care (AOR = 0.64;95%CI = 0.62,0.67) but a higher AOR for institutional (AOR = 2.68;95%CI = 1.84,3.93) and C-section delivery (AOR = 1.28;95%CI = 1.23,1.32) and birthing infants who were moderate-late preterm (AOR = 1.12;95%CI = 1.05,1.20), very preterm (AOR = 1.20;95%CI = 1.04,1.40), extremely pre-term (AOR = 1.65;95%CI = 1.27,2.14), low birthweight (LBW) (AOR = 1.11;95%CI = 1.05,1.17), very LBW (AOR = 1.35;95%CI = 1.12,1.62), and extremely LBW (AOR = 1.71;95%CI = 1.36,2.16). Colombians had decreased AORs for adequate prenatal care (AOR = 0.82;95%CI = 0.78,0.87) but increased AORs for institutional (AOR = 2.03;95%CI = 1.19,3.46) and C-section deliveries (AOR = 1.07;95%CI = 1.01,1.13) and birthing infants with moderate-late preterm (AOR = 1.17;95%CI = 1.05,1.30) but not LBW.
Discussion
The findings underscore the need to address the causes of adequate prenatal care, excess C-sections, and poorer infant outcomes among refugee and immigrant women, especially Venezuelans.
Similar content being viewed by others
Background
South America is home to millions of forcibly displaced persons from the same region including an estimated 7.0 million Colombians and 5.6 million Venezuelans [1, 2]. Ecuador is a major receiving country for both groups [2]. During the past four decades, armed conflicts in Colombia between governmental forces and guerilla groups (FARC, ELN), paramilitary organizations, and narco-traffickers resulted in an estimated 50,000-200,000 deaths and the displacement of millions more [3,4,5]. Although the Colombian government and FARC signed a peace accord in 2016, renewed armed conflict and criminal gang activities caused the security situation along the Colombian-Ecuador border to deteriorate in 2018. However, even with the advent of the Covid-19 epidemic causing frequent border shutdowns, an estimated 400–500 Colombians continued to cross into Ecuador each month to seek refuge [6]. Nearly 68,000 officially recognized Colombians currently reside in Ecuador and an estimated 236,000 others with “irregular” (undocumented) status are in the process of seeking asylum or legal refugee status [7].
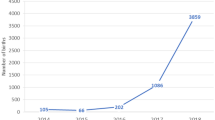
The ongoing exodus of Venezuelans from their home country is the second largest recorded population displacement in the world [1]. The origins of the country’s current complex humanitarian emergency date back more than a decade [8]. However, in recent years, the country’s economic, political, and human rights situation deteriorated even further as inflation soared, violence and crime increased, and shortages of food, medicine, vaccines, and basic services (e.g., water, electricity, health care) became more common. This situation contributed to high rates of malnutrition, infectious and chronic disease morbidity, and maternal-infant mortality [2, 8,9,10]. The number of Venezuelan refugees living in Ecuador has been increasing since 2016 and in 2018, surpassed those from Colombia. Ecuador presently hosts 430,000 legally recognized Venezuelan refugees [3, 8, 9] but many thousands more undocumented persons also are believed to be in the country [9].
Refugees and other forcibly displaced persons can have poor health due to the multiple physical and mental hardships they experience prior to, during, and/or after migration such as harsh environmental conditions, hunger, infectious diseases, exacerbation of pre-existing health conditions, physical violence, and stress, among others [11,12,13,14]. These exposures, coupled with reduced access to maternal and other health care, can increase maternal-fetal risk for adverse outcomes [15,16,17].
Few studies have reported on the maternal care and birth outcomes of pregnant Venezuelan refugees living in South American host countries and none have done so for Colombian refugees. These limited findings suggest that Venezuelan refugees giving birth in either Brazil [18, 19] or Colombia [20, 21] tend to have limited prenatal care and often deliver by Cesarean-section (C-section) [18,19,20]. Two Colombian studies also reported that low birth weight was more prevalent among the infants of Venezuelan refugees than local country nationals but disagreed with respect to preterm births and low Apgar scores [20, 21]. Examination of the specific maternal care challenges and infant birth outcomes of Venezuelan and Colombian immigrants, including those who are refugees, living in Latin American host countries and other immigrants has practical value for informing public health policy and interventions to improve maternal-child outcomes.
We analyzed Ecuadorian live birth registry data (2018–2020) to compare the maternal care and infant outcomes of Colombian and Venezuelan immigrants, most of whom are most likely refugees, with those of Ecuadorian nationals. Our working hypothesis was both immigrant groups would have poorer access to prenatal care, institutional deliveries, and skilled birth attendants compared to Ecuadorians because of migration-related barriers. We also hypothesized that they would be more likely to give birth by C-section and deliver infants with low birthweight (LBW), preterm birth (PTB), and low Apgar scores due to migration-related exposure to stressors that negatively impact maternal-fetal health.
Methods
Data Source and Participants
We analyzed the three most recent years of national live birth registry records collected and maintained by the Ecuadorian National Institute of Statistics and Census (Spanish acronym: INEC) [22]. The birth registry data were recorded on a standard form that was completed by the medical professional (institutional births) or a civil registry official/other authorized personnel (home/other non-institutional births). The de-identified database included all live births registered in Ecuador between January 1, 2018-December 31, 2020 (n = 845,814). We sequentially excluded multiple gestations (n = 12,304) and cases missing data on infant number (n = 20,312), gestational age (n = 8,690), infant birthweight (n = 832), prenatal care (n = 433), and maternal age, ethnicity, and other sociodemographic variables (n = 896). We also excluded foreign nationals whose reported nationality was other than Colombian or Venezuelan (n = 3,866) and as well as records missing data on nationality (n = 360). This resulted in a total of 798,121 cases available for the analyses: Venezuelans (n = 22,619), Colombians (n = 7,638), and Ecuadorian nationals (n = 767,864).
The United Nations High Commission on Refugees (UNHCR) defines refugees as, “people who have fled war, violence, conflict or persecution and have crossed an international border to find safety in another country” [23]. Based on circumstantial evidence from INEC migration statistics [24] and published reports from UNHCR and other refugee-serving organizations for the same time period suggests that the majority of the Venezuelan and Colombian immigrants whose birth were recorded in the INEC birth registry database were most likely refugees [2, 3, 8, 9, 25]. However, since the database did not provide information on the legal status of these women, in this paper, we refer them as “immigrants.”
Maternal Care and Infant Birth Outcomes
The database contained information on the number but not the timing of prenatal visits. Thus, we used a modification of WHO antenatal care recommendations [26] to classify prenatal care adequacy: delivery at weeks 21–23, (≥ 2 contacts), weeks 24–26 (≥ 3 contacts), weeks 27–30 (≥ 4 contacts), weeks 31–34 (≥ 5 contacts), weeks 35–36 (≥ 6 contacts), weeks 37–38 (≥ 7 contacts), and weeks 39–42 (≥ 8 contacts). Other maternal care outcomes analyzed in the study included birth attendant (skilled, unskilled), delivery mode (vaginal, C-section), and delivery site type (institutional, non-institutional). Institutional deliveries were defined as those that occurred in a public, private, or non-governmental health care facility and non-institutional deliveries were those that took place in a home or other non-health care setting. The Ministry of Public Health operates the single largest public health care system in Ecuador. It provides universal health care through its extensive network of hospitals and regional health clinics. The Ecuadorian Social Security Institute operates the second largest public health care system in the country. IESS hospitals and clinics provide services for its members and their families through employee and employer payroll deductions or through voluntary payments. The Guayaquil Welfare Board is a large non-profit non-governmental organization that operates several hospitals in Guayaquil, Ecuador’s largest city. Hospital and clinics run by the national armed forces, national police service, and municipal hospitals and clinics constitute other types of public health care entities in Ecuador. The private for-profit health care institutions were comprised of privately operated hospital, clinics, and medical offices. The two non-institutional delivery sites reported in the database were home (i.e., home births) and other locations where women gave birth such as public roadways, parks, and commercial centers.
Infant gestational age was classified as extremely preterm (< 28 wk), very preterm (28–32 wk), moderate-late preterm (32–36 wk), and term birth (≥ 37 wk). Birthweight was categorized as extremely low birthweight (< 1000 gm), very low birthweight (1000–1499 gm), low birthweight (1500–2499 gm), and average birthweight (2500–3999 gm). One- and 5-minute Apgar scores were categorized as low (< 7) or not low (≥ 7).
Data Analysis
Summary data are presented as number (%) or mean ± SD. Our initial analyses compared maternal nationality with maternal care and infant birth outcome variables using X2 or ANOVA, as appropriate. We used GLM to analyze the unadjusted and adjusted associations of maternal nationality (Venezuelan immigrant, Colombian immigrant, Ecuadorian national) with the average number of prenatal visits. The adjusted model included maternal age, ethnicity, education, marital status, urbanicity, parity, gestational age, birth year, and province region. Bivariate logistic regression models were constructed to analyze the association of maternal nationality with maternal care categorical indicators including prenatal care (adequate, inadequate), delivery site (institutional, non-institutional), delivery mode (vaginal, C-section), and birth attendant (skilled, unskilled). The bivariate regression models produced unadjusted (OR) and adjusted odds ratio (AOR) estimates with their 95% confidence intervals.
Multinomial logistic regression was used to analyze the association of maternal nationality with infant categorical outcomes: gestation length (extremely pre-term, very pre-term, moderate-late pre-term, term) and birthweight (extremely low birthweight, very low birthweight, low birthweight, average birthweight). Bivariate logistic regression analysis was used for the 1-and 5-minute Apgar scores (low, not low). The logistic regression models produced unadjusted (OR) and adjusted odds ratio (AOR) estimates with their 95% confidence intervals.
The maternal care and infant birth outcome models adjusted for conceptually relevant covariates including maternal age, ethnicity, education, marital status, parity, and urbanicity. In addition to these variables, the delivery mode model also adjusted for gestational age, prenatal care adequacy and delivery site while the Apgar score models also included gestational age. Furthermore, all of the multivariate models also adjusted for birth year and province region. The publicly available, de-identified live-birth registry database published by INEC was classified, as “Research not subject to human subjects regulations,” and was exempt from human subject review by the Indiana University Institutional Review Board (https://research.iu.edu/compliance/human-subjects/review-levels/index.html).
Results
Table 1 compares the characteristics of Venezuelan and Colombian women immigrants with the Ecuadorian reference group. As it indicates, the two immigrant groups differed from Ecuadorian nationals as well as from each other on maternal age, ethnicity, education, parity, and other sociodemographic and reproductive history characteristics.
Venezuelan (adj. mean = 5.4; 95% C.I.= 5.3, 5.4 visits) and Colombian immigrants (adj. mean = 5.9; 95% C.I.=5.8, 5.9 visits) reported fewer prenatal visits, on average, than Ecuadorians (6.0; 95% C.I.=6.0,6.0 visits) even after adjustment for parity, education, and other covariates (p = 0.0001). As Table 2 shows, Venezuelan and Colombian immigrants had an unadjusted OR for adequate prenatal care that was respectively reduced by 30% and 17% compared to the reference group. The addition of covariates to the adjusted model further reduced the odds of adequate prenatal care by 36% among Venezuelans and 18% among Colombians.
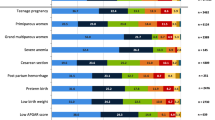
Figure 1 reports on the specific institutional health care and non-institutional sites where women delivered their pregnancies. 65% of all women in the study gave birth at a Ministry of Public Health facility with a significantly greater proportion of immigrant women doing so compared to the Ecuadorian reference group. In contrast, a greater proportion of Ecuadorians than immigrants delivered at facilities operated by private, for-profit entities, Guayaquil Welfare Board, Social Security Institute, or other public institutions. Relatively few women in the study gave birth at home or at another non-medical site (e.g., public roadway, park, commercial center). As Fig. 1 indicates, fewer than 60 of such births occurred among Venezuelan and Colombian immigrants compared to 2,500 recorded for Ecuadorians.
Delivery sites of who delivered a live-born singleton infant in Ecuador, 2018–2020: Colombian and Venezuelan immigrants vs. Ecuadorians. NOTES: [1] Colombian immigrants (n = 4); Venezuelan immigrants (n = 7); Ecuadorian nationals (n = 942). [2] Colombian immigrants (n = 16); Venezuelan immigrants (n = 31); Ecuadorian nationals (n = 1570)
The unadjusted odds of an institutional delivery by Venezuelan and Colombian immigrants was 2.0 and 1.3 times higher than that recorded for Ecuadorians (Table 2). After inclusion of covariates, the adjusted ORs for institutional delivery increased to 2.7 for Venezuelans and 2.0 for Colombians. As Table 2 also indicates, both the unadjusted and adjusted ORs for having a skilled birth attendant present at delivery were similar for both immigrant groups compared to Ecuadorians. Nearly half (47.4%) of all women delivered by C-section delivery. The unadjusted and adjusted ORs for C-section delivery among Venezuelans was around 25% higher than the Ecuadorian reference group. The unadjusted OR for delivering by C-section among Colombian immigrants was 11% lower than Ecuadorians. However, the addition of parity and other model covariates increased the odds of C-section birth by 9% compared to Ecuadorians.
Table 3 shows that infants born to the immigrant women in the study, especially Venezuelans, had generally less favorable birth outcomes compared to those born to the Ecuadorian reference group. For example, infants delivered by Venezuelans had unadjusted ORs for extremely preterm, very preterm, or moderate-to-late preterm birth that were 1.2 to 1.6 times higher than those of reference group women. After adding model covariates, the adjusted OR for extremely preterm birth increased only minimally while that of the other two preterm birth categories was slightly attenuated. Different from Venezuelan infants, those born to Colombian immigrant women exhibited a higher odds only for moderate-late preterm but not the other two preterm birth categories. The inclusion of covariates in the model minimally increased their unadjusted OR of 1.1 to 1.2 over that of the Ecuadorian reference group infants.
Infants delivered by Venezuelan but not Colombian immigrants had higher adjusted odds for low birthweight, very low birthweight, and extremely low birthweight that were increased 1.3 to 1.7 times over that of Ecuadorian infants. Adjustment for covariates produced only relatively minor changes in the adjusted ORs for all three low birthweight categories (Table 3). Finally, the infants of both immigrant groups had unadjusted ORs for low 1-minute and 5-minute Apgar scores that were increased by 1.3 times higher than those of infants born to the Ecuadorian reference group. The adjusted 1-minute and 5-minute ORs of infants born to Venezuelan immigrants showed only a small change after inclusion of the model covariates. The infants of Colombian immigrants showed a relatively small decrease in their adjusted OR for the 1-minute Apgar score different from their adjusted 5-minute Apgar score OR which was 1.7 times higher compared to Ecuadorian reference group infants.
Discussion
Ecuador is a major host country for Colombians fleeing violence and Venezuelans escaping a complex humanitarian crisis. Migration under these conditions is associated with significant challenges. Many experience physical hardships, emotional stress, physical violence, food insecurity, and other exposures and many have only limited or no access to health care, all of which can negatively impact their health and well-being [11,12,13,14, 27, 28]. Pregnant refuges and other immigrants are particularly vulnerable to the effects of migration-related stressor which can affect their access to maternal care services and negatively affect maternal-fetal outcomes [15,16,17].
To the best of knowledge, ours is the first study to examine these important issues in Venezuelan and Colombian immigrants in Ecuador, many whom the circumstantial evidence suggests are refugees [2, 3, 8, 9, 24, 25]. One of the major findings was that although Venezuelan and Colombian immigrants appeared have better or similar access to certain maternal care services institutional deliveries and skilled birth attendants compared to the Ecuadorian reference group, they were less likely to have adequate prenatal care. This is an important concern since adequate prenatal care is documented as one of the most cost-effective public health interventions for reducing the risk for adverse maternal-perinatal outcomes [26]. Although the prenatal care finding is consistent with the limited data reported for Venezuelan refugees living in other Latin American host countries, i.e., Brazil and Colombia [18,19,20,21], we are unable to compare our findings on those from Colombia due to a lack of published studies.
Refugees and other immigrants in Ecuador, regardless of their legal status or income, are eligible for free prenatal care and other health services through the Ministry of Public Health system [9, 29]. There are several possible reasons why the immigrant women in the study had a lower odds of adequate prenatal care compared to Ecuadorian nationals. One possibility is that some could have spent part or most of their pregnancy in their own home country or on the road prior to arriving in Ecuador. This could have impeded their prenatal care access but once in Ecuador, they were able to access labor and delivery services, primarily through the Ministry of Public Health system. It is also possible that some of the same barriers reported in a recent survey of Venezuelan refugees in Ecuador [9] also could have influenced prenatal care access. The two most common frequent health care barriers identified by Venezuelan refugees were difficulties in obtaining an appointment (40%) and excessive distance/lack of transportation to get to the appointment site (15%) rather than a lack of funds (11%) or legal documentation issues (2%) [9]. The same survey also reported that many refugees seemed to know their constitutional rights to medical attention or options for accessing health care services.
Other reports have suggested that medical appointment access has become more complicated in recent years due to an economic downturn in Ecuador coupled with the massive influx of Venezuelan refugees which severely taxed the ability of the public health system to provide routine services [30,31,32]. Further austerity measures adopted in the months prior to the covid-19 epidemic and the epidemic itself are reported to have negatively impacted health care services including population access to maternal care in Ecuador [33, 34]. Data from the present INEC birth registry database supports this notion since the prevalence of adequate prenatal care among the study women decreased from 2018 to 2020 with the largest declines occurring in Venezuelan immigrants (-31%), followed by Colombian immigrants (-17%), and Ecuadorian nationals (-15%).
Why the Venezuelan and Colombian immigrants in the study had less adequate prenatal care but better access to an institutional delivery than Ecuadorian nationals is unclear. One reason might be because both immigrant groups, particularly Venezuelans, are more likely to live in urban areas where most of the health care institutions in Ecuador are located and where urban transportation is easier to obtain to get to the hospital to deliver different from the situation in rural areas. It is possible that some of the Ecuadorians living in rural areas were unable to make it to the hospital on time. These geographic and other potential factors should be explored in future studies.
The higher odds for a C-section delivery identified among the immigrant women in our study, especially Venezuelans, is worrying. Although this finding is consistent with that reported for refugees from Venezuela who delivered in Brazil [22], it differs from another indicating that C-section births among Venezuelan refugees was slightly reduced compared to Colombian nationals [23].
The reasons for the excess C-section risk identified among immigrant women in the study, Especially Venezuelans, is uncertain. The database did not indicate as to whether these were emergency vs. elective C-sections nor if they were primary or repeat surgeries. The higher odds of preterm birth, low birthweight, and low Apgar scores identified for the infants of one or both immigrant groups suggests that many had high-risk pregnancies which could have increased their risk for a C-section delivery. Our analyses controlled for factors such as parity, prenatal care adequacy, birth site, and several other variables linked to higher C-section risk but could not do so for any potential maternal, fetal, placental or amniotic fluid pathologies since no information on these was included in the database. In any case, the excess C-section deliveries identified in this study for Venezuelan and Colombians immigrants in Ecuador is an important issue requiring further investigation. When medically justified, a C-section delivery can effectively reduce the risk for maternal-infant mortality and morbidity but it is, nevertheless, a surgical intervention associated with both short- and longer-term health risks for both mother and infant [35].
The excess of low birthweight identified among those of Venezuelans in our study is consistent with a study of Venezuelan refugees living in Colombia that analyzed birth registry data for 2016–2018 [21] and another based on the same data source for a single year (2017) [20]. The excess in preterm births identified for babies born to Venezuelans in our study also is consistent with the aforementioned 2016–2018 Colombian birth registry study [21] but differs from the single year study reporting a lack of association [20]. The lower 1- and 5-minute Apgar score odds identified for infants born to Venezuelan immigrants concurs with those reported by the single year Colombian birth registry study [20] but not that of the multiyear study [21]. The generally poorer birth outcomes identified for infants born to the immigrant mothers in our study has clinical and public health importance since those born too early or too small are at-risk for perinatal morbidity and mortality, postnatal growth and development perturbations, and future development of obesity, cardiometabolic and other chronic diseases, and premature mortality [36,37,38,39].
The limited information contained in the Ecuadorian live birth registry database used for the analyses did not permit the identification of proximate risk factors associated with preterm birth, low-birthweight, and low Apgar scores. Examples include undertreated pre-existing chronic and gestational conditions, specific stressors such as food insecurity, undernutrition, infectious diseases, intimate partner and other forms of violence that have been reported to impact Colombian [13, 40,41,42] and Venezuelan refugees living in Ecuador [9, 30,31,32]. Other reports indicate that refugees and other immigrants from these two countries often experience persistent social, economic, and political exclusion and discrimination, a situation that is reported to have worsened with the large recent influx of the latter into Ecuador [4, 9, 30,31,32]. Other reported sources of stress for these includes difficulties in obtaining formal paid employment, adequate housing, or schooling for children and other challenges caused by the Covid-19 epidemic [5, 9, 12, 32]. This is important since fetal exposure to maternal stress hormones, poor nutrition, and other environmental stressors can adversely affect fetal growth, development, and other fetal programming [43,44,45].
This study has some limitations. One is that its cross-sectional design allows for inference but not establishment of causal effects. Its findings are applicable only to women delivering live-born singleton infants. Thus, the prevalence of preterm birth, low birthweight, and/or low Apgar scores could be underestimated because of potential selection bias. In addition, the birth registry database did not contain data on stillbirth, postnatal mortality, and maternal mortality, all of which are important indicators for assessing maternal-infant health. The database specified the nationality of women but for foreign nationals, it did not specify their legal status, length of residence in Ecuador, nor reasons for migration. However, indirect evidence from INEC government migration statistics, and the data and reports published by the UNHCR and other refugee-serving organizations strongly suggests that most were either documented or undocumented refugees. Another limitation was that we were unable to adjust for certain conceptually relevant maternal, fetal, and other covariates in some models because they were not contained in the database. However, despite its limitations, our study contributes to the limited data identifying disparities in maternal care and clinically relevant infant birth outcome indicators in Colombian and Venezuelan refugees and immigrants living in a Latin American host country, in this case, Ecuador.
Conclusions
Our analysis of live birth registry data identified disparities in the prenatal care and infant outcomes of Colombian and Venezuelan immigrants compared to Ecuadorian nationals. Pregnant immigrants who delivered a liveborn singleton infant in Ecuador during 2018–2020 had fewer average prenatal visits and were less likely to have adequate prenatal care than Ecuadorian nationals although they had good access to institutional deliveries, particularly through the MSP public health system. Immigrant women were also more likely than Ecuadorians to give birth by C-section, deliver infants classified as moderate-late preterm, and had low 1- and 5-minute Apgar scores. Moreover, Venezuelan immigrants also delivered babies with more severe forms of prematurity as well as low birthweight. Future cohort design studies should be conducted to confirm our study findings. Mixed-methods investigations would also be useful to help better understand the specific challenges and concerns of refugee and other immigrant women as well as to identify the structural and other barriers that may contribute to their poorer prenatal care and infant outcomes. In turn, this can be used to inform public health policy and develop more effective interventions to improve maternal-child outcomes.
* p = 0.0001; ** linear association p = 0.04.
References
United Nations High Commissioner for Refugees. praises Latin America for its commitment to the inclusion of all those in need of protection 23 June 2021. Accessed at: https://www.unhcr.org/en-us/news/press/2021/6/60d2f8454/un-high-commissioner-refugees-praises-latin-america-its-commitment-inclusion.html.
Migration Data Portal. Regional Data Overview. Migration data in South America. 2021, Accessed at: https://www.migrationdataportal.org/regional-data-overview/migration-data-south-america#recent-trends.
United Nations High Commissioner for Refugees (UNHRC). Ecuador. Fact Sheet, Sept 2019. Accessed at: https://www.acnur.org/op/op_fs/5d8bd87e4/ecuador.
Pugh JD, Luis F, Jiménez, Latuff B. Welcome wears thin for Colombians in Ecuador as Venezuelans become more visible. MDPI. January 9, 2020. https://www.migrationpolicy.org/article/welcome-wears-thin-for-colombians-ecuador.
Pugh JD. Negotiating Identity and Belonging through the Invisibility Bargain: Colombian Forced Migrants in Ecuador. International Migration Review 52 (4): 978–1010. August 14, 2018. Accessed at: https://doi.org/10.1111/imre.12344.
Brown K. Colombian refugees in Ecuador trapped in loops of poverty and insecurity. The New Humanitarian, 3 January 2021. https://www.thenewhumanitarian.org/news-feature/2021/01/13/colombian-migrants-marginalised-ecuador-refugees.
Ledesma N. Ecuador Migration Trends. InterAmerican Dialog, April 5, 2019. http://www.thedialogue.org/wp-content/uploads/2019/04/Ecuador-Migration-Trends.pdf
International Organization for Migration (IOM). World Migration Report 2020. http://www.un.org/sites/un2.un.org/files/wmr_2020.pdf.
World Bank. (2020). Retos y oportunidades de la migración venezolana en Ecuador [Challenges and Opportunities of Venezuelan Migration in Ecuador]. World Bank, 1-2020. http://documents1.worldbank.org/curated/en/453941593004490155/pdf/Retos-y-Oportunidades-de-la-Migracion-Venezolana-en-Ecuador.pdf.
World Report. Human Rights Watch 2021. Venezuela. Events of 2020. Accessed at: https://www.hrw.org/world-report/2021/country-chapters/venezuela.
Pan American Health Organization (PAHO). Health of refugees and migrants. Regional situation analysis, practices, experiences, lessons learned and ways forward. WHO Region of Americas; 2018.
World Health Organization (WHO). Migration and health: key issues. Accessed at: https://www.euro.who.int/en/health-topics/health-determinants/migration-and-health/migration-and-health-in-the-european-region/migration-and-health-key-issues.
Keating C, Treves-Kagan S, Buller AM. Intimate partner violence against women on the Colombia Ecuador border: a mixed-methods analysis of the liminal migrant experience. Confl Health. 2021;15:24. https://doi.org/10.1186/s13031-021-00351-y.
Piérola MD. Marisol Rodríguez Chatruc. Migrants in Latin America: Disparities in Health Status and in Access to Healthcare. Interamerican Development Bank, Discussion paper no. IDP-DP-00784, June 11, 2020. Accessed at. http://Users/18123/AppData/Local/Temp/Migrants-in-Latin-America-Disparities-in-Health-Status-and-in-Access-to-Healthcare.pdf.
Heslehurst N, Brown H, Pemu A, Coleman H, Rankin J. Perinatal health outcomes and care among asylum seekers and refugees: a systematic review of systematic reviews. BMC Med. 2018 Jun 12;16(1):89. doi: https://doi.org/10.1186/s12916-018-1064-0. PMID: 29890984; PMCID: PMC5996508.
Sharma E, Howard N, Duclos D. Navigating new lives: A scoping review and thematic synthesis of forced migrant women’s perinatal experiences. J Migr Health. 2020 Dec 2;1–2:100014. doi: https://doi.org/10.1016/j.jmh.2020.100014. PMID: 34405168; PMCID: PMC8352206.
Fair F, Raben L, Watson H, Vivilaki V, van den Muijsenbergh M, Soltani H. ORAMMA team. Migrant women’s experiences of pregnancy, childbirth and maternity care in European countries: A systematic review. PLoS One. 2020 Feb 11;15(2):e0228378. doi: https://doi.org/10.1371/journal.pone.0228378. PMID: 32045416; PMCID: PMC7012401.
Bahamondes L, Laporte M, Margatho D, de Amorim HSF, Brasil C, Charles CM, Becerra A, Hidalgo MM. Maternal health among Venezuelan women migrants at the border of Brazil. BMC Public Health. 2020 Nov 23;20(1):1771. doi: https://doi.org/10.1186/s12889-020-09912-x. PMID: 33228642; PMCID: PMC7682772.
Doocy S, Page KR, de la Hoz F, Spiegel P, Beyrer C. Venezuelan migration and the border health crisis in Colombia and Brazil. J Migr Hum Security. 2019;7:79–91.
Garnica-Rosas L, Granich-Armenta A, Guerra Y, Guerra G, Sánchez-Dominguez M, Lamadrid-Figueroa H. Perinatal Outcomes Among Venezuelan Immigrants in Colombia: A Cross-Sectional Study. J Immigr Minor Health. 2021 Oct;23(5):976–85. doi:https://doi.org/10.1007/s10903-021-01248-x. Epub 2021 Aug 7. PMID: 34363575; PMCID: PMC8346779.
Guarnizo-Herreño CC, Wehby GL. Health of Infants Born to Venezuelan Refugees in Colombia. J Immigr Minor Health. 2021 Apr;23(2):222–31. doi:https://doi.org/10.1007/s10903-020-01114-2. Epub 2021 Feb 7. PMID: 33550477.
Instituto Nacional de Estadistica y Censos (INEC). Registros Estadísticos de Nacidos Vivos y Defunciones Fetales. Accessed at: https://www.ecuadorencifras.gob.ec/nacidos-vivos-y-defunciones-fetales/.
United Nations High Commissioner for Refugees (UNHCR). What is a Refugee? 2021. Accessed at: https://www.unhcr.org/en-us/what-is-a-refugee.html.
Instituto Nacional de Estadistica y Censos (INEC). Registro Estadístico de Entradas y Salidas. Accessed at: https://www.ecuadorencifras.gob.ec/entradas-y-salidas-internacionales/.
United Nations High Commissioner for Refugees (UNHCR). Global Focus. Ecuador, 2021. Accessed at: https://reporting.unhcr.org/ecuador.
World Health Organization. WHO recommendations on antenatal care for a positive pregnancy experience. Geneva Switzerland, World Health Organization, 2016. https://www.who.int/publications/i/item/9789241549912.
Gallo Marin B, Amaya A, Medina Perez G, Levine AC, Moretti K, Garbern SC. A Scoping Review of Non-Communicable Diseases and Maternal and Child Health Needs of Venezuelan Migrants in South America. J Glob Health Rep. 2021;5:e2021045. doi:https://doi.org/10.29392/001c.23621.
Fellmeth G, Fazel M, Plugge E. Migration and perinatal mental health in women from low- and middle-income countries: a systematic review and meta-analysis. BJOG. 2017 Apr;124(5):742–52. doi:https://doi.org/10.1111/1471-0528.14184. Epub 2016 Jun 20. PMID: 27320110.
Republic of Ecuador. LEY ORGÁNICA DE MOVILIDAD HUMANA. Registro Oficial No. 938 – Suplemento. Feb. 2017. Accessed at: https://www.acnur.org/fileadmin/Documentos/BDL/2017/10973.pdf.
Miller S, Panayotatos D. A Fragile Welcome. Ecuador’s Response to the Influx of Venezuelan Refugees and Migrants. Refugees International Field Report; June 2019. Accessed at. https://www.refugeesinternational.org/reports/2019/6/17/a-fragile-welcome.
United Nations High Commissioner for Refugees (UNHCR). RMRP 2020 for Refugees and Migrants from Venezuela. Jan.-Dec. 2020.
Chaves-González D, Amaral J, Mora MJ. Socioeconomic Integration of Venezuelan Migrants and Refugees. The Cases of Brazil, Chile, Colombia, Ecuador, and Peru. Washington, DC and Panama City: Migration Policy Institute and International Organization for Migration; 2021.
Castro A. UNDP LAC C19 PDS No. 19 Challenges posed by the COVID-19 pandemic in the health of women, children, and adolescents in Latin America and the Caribbean. UNDP Latin America and the Caribbean #COVID19 | POLICY DOCUMENTS SERIES. Accessed at. Challenges posed by. the COVID-19 pandemic in the health of women, children, and adolescents in Latin America and the Caribbean (unicef.org).
United Nations. Plan de Respuesta Humanitaria COVID-19 Ecuador. Equipo Humanitario de Pais, April 2020. Accessed at: 20200430-EHP-ECUADOR-COVID-19.pdf (reliefweb.int).
World Health Organization. WHO Statement on Caesarean Section Rates, 2015. http://apps.who.int/iris/bitstream/handle/10665/161442/WHO_RHR_15.02_eng.pdf;jsessionid=235FDF8C0D63C0FEE812ACD26E47EDF6?sequence=1.
Vogel JP, Chawanpaiboon S, Moller AB, Watananirun K, Bonet M, Lumbiganon P. The global epidemiology of preterm birth. Best Pract Res Clin Obstet Gynaecol. 2018 Oct;52:3–12. doi:https://doi.org/10.1016/j.bpobgyn.2018.04.003. Epub 2018 Apr 26. PMID: 29779863.
Blencowe H, Cousens S, Chou D, et al. Born too soon: the global epidemiology of 15 million preterm births. Reprod Health. 2013;10(Suppl 1):2. doi:https://doi.org/10.1186/1742-4755-10-S1-S2. Suppl 1 ) .
Blencowe H, Krasevec J, de Onis M, Black RE, An X, Stevens GA, Borghi E, Hayashi C, Estevez D, Cegolon L, Shiekh S, Ponce Hardy V, Lawn JE, Cousens S. National, regional, and worldwide estimates of low birthweight in 2015, with trends from 2000: a systematic analysis. Lancet Glob Health. 2019 Jul;7(7):e849-e860. doi: 10.1016/S2214-109 × (18)30565-5. Epub 2019 May 15. PMID: 31103470; PMCID: PMC6560046.
Embleton ND, Katz J, Ziegler EE, editors: Low-Birthweight Baby: Born Too Soon or Too Small. Nestlé Nutr Inst Workshop Ser. Nestec Ltd. Vevey/S. Karger AG Basel, © 2015, vol 81, pp 1–7. https://doi.org/10.1159/000365790.
UNHCR and Insituto de la Ciudad 2014. Urban Profiles of the Colombian Population in Quito. Refugees, asylum seekers and other migrants. Main results and recommendations. file:///C:/Users/18123/AppData/Local/Temp/Profiling-report-Ecuador-PerfilesUrbanosQuito-2014-EN.pdf.
No se puede ser refugiado toda la vida”… Refugiados urbanos: el caso de la población colombiana en Quito y Guayaquil / coordinado por Carlos Ortega y Oscar Ospina. Quito:FLACSO, Sede Ecuador, 2012.
Bilsborrow RE, Mena CF, Arguello E. Colombian Refugees in Ecuador: Sampling Schemes, Migratory Patterns and Consequences for Migrants. Int J Global Environ Issues. 2011;11(3/4):271–98.
Traylor CS, Johnson JD, Kimmel MC, Manuck TA. Effects of psychological stress on adverse pregnancy outcomes and nonpharmacologic approaches for reduction: an expert review. Am J Obstet Gynecol MFM. 2020 Nov;2(4):100229. doi:https://doi.org/10.1016/j.ajogmf.2020.100229. Epub 2020 Sep 24. PMID: 32995736; PMCID: PMC7513755.
Vohr BR, Poggi Davis E, Wanke CA, Krebs NF. Neurodevelopment: The Impact of Nutrition and Inflammation During Preconception and Pregnancy in Low-Resource Settings. Pediatrics. 2017 Apr;139(Suppl 1):S38-S49. doi: https://doi.org/10.1542/peds.2016-2828F. PMID: 28562247.
Mousa A, Naqash A, Lim S. Macronutrient and Micronutrient Intake during Pregnancy: An Overview of Recent Evidence. Nutrients. 2019;11(2):443. doi:https://doi.org/10.3390/nu11020443. Published 2019 Feb 20.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Weigel, M.M., Armijos, R.X. Maternal Care and Pregnancy Outcomes of Venezuelan and Colombian Refugees. J Immigrant Minority Health 25, 86–95 (2023). https://doi.org/10.1007/s10903-022-01370-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10903-022-01370-4