Abstract
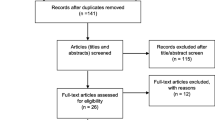
While Asian Indians (AIs) are the third fastest-growing Asian minority population in the United States, they fall short of the Healthy People cervical cancer screening target goals, with rates averaging 70% compared to 83% among non-Hispanic Whites. The purpose of this systematic review is to examine factors influencing cervical cancer screening behaviors among AIs in the US. Medline, CINAHL, PubMed, PsychINFO, and ProQuest databases were searched for qualitative and quantitative studies conducted between 1990 and 2017 that focused on cervical cancer screening behaviors among AIs in the US. The seven selected quantitative cross-sectional descriptive studies show that acculturation, length of stay in the US, age, education level, employment, cultural beliefs, and language influence cervical cancer screening behaviors among AIs in the US. Results from this systematic review inform development of culturally sensitive interventions to raise awareness and engagement in cervical cancer screening among AIs.

Similar content being viewed by others
References
American Cancer Society. (n.d.). American Cancer Society: Cancer facts & figures 2017. https://www.cancer.org/research/cancer-facts-statistics/all-cancer-facts-figures/cancer-facts-figures-2017.html
SEER fast stats: Age-adjusted rates by data type, cervix uteri, all ages, all races, female, 1992–2014. (2017). National Cancer Institute. https://seer.cancer.gov/faststats/selections.php?run=runit&output=2&statistic=1&cancer=57&year=201702&race=1&sex=3&age=1&series=data&data=1;13;2
Healthy people 2010: Understanding and improving health (2nd Ed.) (2000).U. S. Department of Health and Human Services. National Institute of Health. http://www.health.gov/healthypeople/PrevAgenda/ goals.htm
Healthy People 2020. (2010). U. S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion https://www.healthypeople.gov/2020/About-Healthy-People
U.S. Preventive Services Task Force. (2017). Draft recommendation statement: Cervical cancer screening. https://www.uspreventiveservicestaskforce.org/Page/Document/draft-recommendation-statement/cervical-cancer-screening2
The American Congress of Obstetrics and Gynecologists. (n.d.). Cervical Cancer Screening Guidelines. ACOG Online. https://www.acog.org
CDC. Human papillomavirus-associated cancers—United States, 2004–2008. MMWR Morb Mortal Wkly Rep. 2012;61:258–61.
World Cancer Research Fund. (2018). Cervical Cancer Statistics. https://www.wcrf.org/dietandcancer/cancer-trends/cervical-cancer-statistics
Hoeffel, E. M., Rastogi, S., Kim, M. O., & Shahid, H. (2011). The Asian population: 2010. U.S. Department of Commerce, Economics and Statistics Administration, U.S. Census Bureau. https://www.census.gov/prod/cen2010/briefs/c2010br-11.pdf
Ryan, C. L., & Bauman, K. (2016). Educational Attainment in the United States: 2015. U.S. Department of Commerce Economics and Statistics Administration. U.S. Census Bureau. U.S. Census Bureau Online. www.census.gov/content/dam/Census/library/publications/2016/demo/p20-578.pdf
Allard, M. D. (n.d.) U.S. Bureau of Labor Statistics. 2011. Asians in the U.S. Labor Force. www.bls.gov/opub/mlr/2011/11/art1full.pdf
White A, Thompson TD, White MC, Sabatino SA, de Moor J, Doria-Rose PV, Geiger AM, Richardson LC. Cancer screening test use—United States 2015. MMWR Morb Mortal Wkly Rep. 2017;66(8):201–6. https://doi.org/10.15585/mmwr.mm6608a1.
American Cancer Society. (2016). American Cancer Society: Cancer facts & figures 2016. https://www.cancer.org/research/cancer-facts-statistics/all-cancer-facts-figures/cancer-facts-figures-2016.html
Nghiem VT, Davies KR, Chan W, Mulla ZD, Cantor SB. Disparities in cervical cancer survival among Asian-American women. Ann Epidemiol. 2016;26(1):28–35. https://doi.org/10.1016/j.annepidem.2015.10.004.
Islam NS, Trinh-Shevrin C, Rey MJ. Toward a contextual understanding of Asian American health. In: Asian American communities and health: context, research, policy, and action. Hoboken: Wiley; 2009. p. 3–22.
Budhwani H, De P. Human papillomavirus vaccine initiation in Asian Indians and Asian subpopulations: a case for examining disaggregated data in public health research. J Public Health. 2017;153:111–7. https://doi.org/10.1016/j.puhe.2017.07.036.
Chaudhary N, Vyas A, Parrish EB. Community based organizations addressing South Asian American health. J Community Health. 2010;35(4):384–91.
Fink A. Conducting research literature reviews: from the internet to paper. 2nd ed. Thousand Oaks: Sage Publications; 2005. p. 136–44.
Mehrotra N, Gaur S, Petrova A. Health care practices of the foreign born Asian Indians in the United States. A community based survey. J Community Health. 2012;37(2):328–34.
Misra R, Menon U, Vadaparampil S, BeLue R. Age- and sex-specific cancer prevention and screening practices among Asian Indian immigrants in the United States. J Investig Med. 2011;59(5):787–92.
Misra R, Vadaparampil S. Personal cancer prevention and screening practices among Asian Indian physicians in the United States. Cancer Detect Prev. 2004;28(4):269–76.
Ross JS, Nuñez-Smith M, Forsyth BA, Rosenbaum JR. Racial and ethnic differences in personal cervical cancer screening amongst post-graduate physicians: Results from a cross-sectional survey. BMC Public Health. 2008;8:378. https://doi.org/10.1186/1471-2458-8-378.
Williams JJ, Santoso JT, Ling FW, Przepiorka D. Regular article: Pap smear noncompliance among female obstetrics-gynecology residents. Gynecol Oncol. 2003;90:597–600. https://doi.org/10.1016/S0090-8258(03)00406-2.
Shoemaker ML, White MC. Breast and cervical cancer screening among Asian subgroups in the USA: estimates from the National Health Interview Survey, 2008, 2010, and 2013. Cancer Causes Control CCC. 2016;27(6):825–9. https://doi.org/10.1007/s10552-016-0750-5.
Thompson CA, Gomez SL, Chan A, Chan JK, McClellan SR, Chung S, Olson C, Nimbal V, Palaniappan LP. Patient and provider characteristics associated with colorectal, breast, and cervical cancer screening among Asian Americans. Cancer Epidemiol Biomark Prev. 2014;23(11):2208–17.
Leyden WA, Manos MM, Geiger AM, Weinmann S, Mouchawar J, Bischoff K. Cervical cancer in women with comprehensive health care access: attributable factors in the screening process. J Natl Cancer Inst. 2005;97(9):675–80.
Forman D, Martel CD, Lacey CJ, Soerjomataram I, Lortet-Tieulent J, Bruni L. Global burden of human papillomavirus and related diseases. Vaccine. 2012;30:F12–23.
Vaccarella S, Lortet-Tieulent J, Plummer M, Franceschi S, Bray F. Worldwide trends in cervical cancer incidence: impact of screening against changes in disease risk factors. European Journal for Cancer. 2013;49:3262–73.
Wang SS, Carreon JD, Gomez SL, Devesa SS. Cervical cancer incidence among 6 Asian ethnic groups in the United States, 1996 through 2004. Cancer. 2010;116:949–56.
Melnikow, J., Henderson, J. T., Burda, B. U., et al. (2017). Screening for cervical cancer with high-risk human papillomavirus testing: A systematic evidence review for the U.S. Preventive Services Task Force. Evidence Synthesis No. 158. Agency for Healthcare Research and Quality. https://www.ahrq.gov
Datta SD, Koutsky LA, Ratelle S, Unger ER, Shlay J, McClain T, et al. Human papillomavirus infection and cervical cytology in women screened for cervical cancer in the United States, 2003–2005. Ann Intern Med. 2008;148(7):493–500.
Ferlay, J., Soerjomataram, I., Ervik, M., Dikshit, R., Eser, S., Mathers, C., Rebelo, M., Parkin, D. M., Forman, D., & Bray, F. (2013). GLOBOCAN 2012 v1.0, Cancer Incidence and Mortality Worldwide: IARC CancerBase No. 11. International Agency for Research on Cancer. http://globocan.iarc.fr
Scarinci IC, Garcia FR, Kobetz E, Partridge EE, Brandt HM, Bell MC, et al. Cervical cancer prevention: new tools and old barriers. Cancer. 2010;116(11):2531–42. https://doi.org/10.1002/cncr.25065.
Marlow LV, Waller J, Evans REC, Wardle J. Predictors of interest in HPV vaccination: a study of British adolescents. Vaccine. 2009;27:2483–8.
Bernard VB, Royalty J, Saraiya M, Rockwell T, Helsel W. The effectiveness of targeting never or rarely screened women in a national cervical cancer screening program for underserved women. Cancer Causes Control CCC. 2015;26(5):713–9. https://doi.org/10.1007/s10552-015-0542-3.
Marlow LV, Wardle J, Waller J. Understanding cervical screening non-attendance among ethnic minority women in England. Br J Cancer. 2015;113(5):833–9. https://doi.org/10.1038/bjc.2015.248.
Waller J, Jackowska M, Marlow LV, Wardle J. Exploring age differences in reasons for nonattendance for cervical screening: a qualitative study. BJOG Int J Obstet Gynaecol. 2011;119:26–32. https://doi.org/10.1111/j.1471-0528.2011.03030.x.
Waller J, Bartoszek M, Marlow LV, Wardle J. Barriers to cervical cancer screening attendance in England: a population-based survey. J Med Screen. 2009;16(4):199–204.
McCaffery K, Forrest S, Waller J, Desai M, Szarewski A, Wardle J. Attitudes towards HPV testing: a quantitative study of beliefs among Indian, Pakistani, African-Caribbean and White British women in the UK. Br J Cancer. 2003;88:42–6. https://doi.org/10.1038/sj.bjc.6600686.
Colby, S. L., & Ortman, J. M. (2009). Projections of the size and composition of the U.S. population: 2014 to 2060, Current Population Reports, 25–1143. U.S. Census Bureau. www.census.gov/content/dam/Census/library/publications/2015/.../p25-1143.pdf?
Roy S, Shankar A. HPV vaccination of girl child in India: intervention for primary prevention of cervical cancer. Asian Pac J Cancer Prev APJCP. 2018;19(9):2357–8. https://doi.org/10.22034/APJCP.2018.19.9.2357.
Kar SB, Campbell K. Invisible Americans: an exploration of Indo-American quality of life. Amerasia J. 1995;21(3):25–52.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Jillapalli, R., Radhakrishnan, K. Cervical Cancer Screening Behaviors Among Asian Indians in the United States: A Systematic Review. J Immigrant Minority Health 24, 779–789 (2022). https://doi.org/10.1007/s10903-021-01237-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10903-021-01237-0