Abstract
Background
Health literacy has yet to be described in a non-clinical, racially diverse, community-based cohort.
Methods
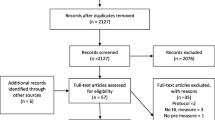
Four questions assessing health literacy were asked during annual phone encounters with Multi-Ethnic Study of Atherosclerosis (MESA) participants between 2016 and 2018 (n = 3629). We used prevalence ratios (PRs) with 95% confidence intervals (CIs) to characterize how demographic and acculturation factors related to limited health literacy. Models adjusted for age, sex, and race/ethnicity, and race/ethnicity-stratified models were also examined.
Results
Limited health literacy was prevalent in 15.4% of the sample. Participants who were older, female, lower-income, or less acculturated were at greater risk for having limited health literacy. Chinese, Hispanic, and Black participants were more likely than White participants to have limited health literacy. Patterns were similar when stratified by race/ethnicity.
Discussion
Within MESA limited health literacy was common, particularly among Chinese and Hispanic participants, with some of the variance explained by differences in acculturation.


Similar content being viewed by others
Change history
13 January 2021
A Correction to this paper has been published: https://doi.org/10.1007/s10903-020-01137-9
References
What is health literacy? | Health literacy | CDC [Internet]. 2018 [cited 2019 Sept 28]. Available from: https://www.cdc.gov/healthliteracy/learn/index.html
Magnani JW, Mujahid MS, Aronow HD, Cené CW, Vaughan DV, Edward H, et al. Health literacy and cardiovascular disease: fundamental relevance to primary and secondary prevention: a scientific statement from the American Heart Association. Circulation. 2018;138:e48–74.
The health literacy of America’s adults: results from the 2003 national assessment of adult literacy. 2003;76.
Volandes AE, Paasche-Orlow MK. Health literacy, health inequality and a just healthcare system. Am J Bioeth. 2007;7:5–10.
Health literacy – fact sheet: health literacy basics [Internet]. [cited 2019 Sept 25]. Available from: https://health.gov/communication/literacy/quickguide/factsbasic.htm
Farrell TW, Chandran R, Gramling R. Understanding the role of shame in the clinical assessment of health literacy. Fam Med. 2008;40:235–6.
Baker DW, Parker RM, Williams MV, Pitkin K, Parikh NS, Coates W, et al. The health care experience of patients with low literacy. Arch Fam Med. 1996;5:329–34.
Ornstein SM, Nietert PJ, Jenkins RG, Litvin CB. The prevalence of chronic diseases and multimorbidity in primary care practice: a PPRNet report. J Am Board Fam Med. 2013;26:518–24.
Association of health literacy with medication knowledge, adherence, and adverse drug events among elderly veterans. J Health Commun:17, No sup3 [Internet]. [cited 2019 Sept 25]. Available from: https://www.tandfonline.com/doi/full/10.1080/10810730.2012.712611
Kreps GL, Sparks L. Meeting the health literacy needs of immigrant populations. Patient Educ Couns. 2008;71:328–32.
Alba AD, Britigan DH, Lyden E, Johansson P. Assessing health literacy levels of Spanish-speaking Hispanic patients in Spanish at federally qualified health centers (FQHCs) in the Midwest. J Health Care Poor Underserved. 2016;27:1726–32.
López L, Grant RW, Marceau L, Piccolo R, McKinlay JB, Meigs JB. Association of acculturation and health literacy with prevalent Dysglycemia and diabetes control among Latinos in the Boston Area Community Health (BACH) survey. J Immigr Minor Health. 2016;18:1266–73.
Moser DK, Robinson S, Biddle MJ, Pelter MM, Nesbitt T, Southard J, et al. Health literacy predicts morbidity and mortality in rural patients with heart failure. J Card Fail. 2015;21:612–8.
Peterson PN, Shetterly SM, Clarke CL, Bekelman DB, Chan PS, Allen LA, et al. Health literacy and outcomes among patients with heart failure. JAMA. 2011;305:1695–701.
Stewart DW, Cano MÁ, Correa-Fernández V, Spears CA, Li Y, Waters AJ, et al. Lower health literacy predicts smoking relapse among racially/ethnically diverse smokers with low socioeconomic status. BMC Public Health. 2014;14:716.
Gazmararian JA, Williams MV, Peel J, Baker DW. Health literacy and knowledge of chronic disease. Patient Educ Couns. 2003;51:267–75.
Bild DE, Bluemke DA, Burke GL, Detrano R, Diez Roux AV, Folsom AR, et al. Multi-ethnic study of atherosclerosis: objectives and design. Am J Epidemiol. 2002;156:871–81.
Rodriguez F, Hicks LS, López L. Association of acculturation and country of origin with self-reported hypertension and diabetes in a heterogeneous Hispanic population. BMC Public Health. 2012;12:768.
Lutsey PL, Diez Roux AV, Jacobs DR, Burke GL, Harman J, Shea S, et al. Associations of acculturation and socioeconomic status with subclinical cardiovascular disease in the multi-ethnic study of atherosclerosis. Am J Public Health. 2008;98:1963–70.
Chew LD, Bradley KA, Boyko EJ. Brief questions to identify patients with inadequate health literacy. Fam Med. 2004;36:588–94.
Woloshin S, Schwartz LM, Welch HG. Patients and medical statistics: interest, confidence, and ability. J Gen Intern Med. 2005;20:996–1000.
Mackert M, Mabry-Flynn A, Donovan EE, Champlin S, Pounders K. Health literacy and perceptions of stigma. J Health Commun. 2019;24:856–64; Taylor & Francis
Perez A. Acculturation, health literacy, and illness perceptions of hypertension among hispanic adults. J Transcult Nurs. 2015;26:386–94.
Li C-C, Matthews AK, Dong X. The influence of health literacy and acculturation on cancer screening behaviors among older Chinese Americans. Gerontol Geriatr Med. 2018;4:233372141877819.
Shea JA, Beers BB, McDonald VJ, Quistberg DA, Ravenell KL, Asch DA. Assessing health literacy in African American and Caucasian adults: disparities in Rapid Estimate of Adult Literacy in Medicine (REALM) scores: 7
Low health literacy and health outcomes: an updated systematic review | Annals of internal medicine | American College of Physicians [Internet]. [cited 2019 Sept 25]. Available from: https://annals.org/aim/fullarticle/747040?casa_token=D6dFDoH3f-4AAAAA:tS_EuBhJqKxTP7arjuei6B_vzUH7tOKgNU5kn_UVX4VfElN0ejTIxZwq1FLw8tPqLPXp16p3Zw
Ciampa PJ, White RO, Perrin EM, Yin HS, Sanders LM, Gayle EA, et al. The association of acculturation and health literacy, numeracy and health-related skills in Spanish-speaking caregivers of young children. J Immigr Minor Health. 2013;15:492–8.
Low health literacy and cancer screening among Chinese Americans in California: a cross-sectional analysis | BMJ Open [Internet]. [cited 2019 Sept 25]. Available from: https://bmjopen.bmj.com/content/5/1/e006104?int_source=trendmd&int_medium=trendmd&int_campaign=trendmd
Chew LD, Griffin JM, Partin MR, Noorbaloochi S, Grill JP, Snyder A, et al. Validation of screening questions for limited health literacy in a large VA outpatient population. J Gen Intern Med. 2008;23:561–6.
Health literacy tool shed: a source for validated health literacy instruments. J Consum Health on the Internet: 21(1) [Internet]. [cited 2019 Sept 25]. Available from: https://www.tandfonline.com/doi/abs/10.1080/15398285.2017.1280344
Health literacy explains racial disparities in diabetes medication adherence. J Health Commun: 16, No sup3 [Internet]. [cited 2019 Sept 25]. Available from: https://www.tandfonline.com/doi/full/10.1080/10810730.2011.604388
James DCS, Harville C, Efunbumi O, Martin MY. Health literacy issues surrounding weight management among African American women: a mixed methods study. J Hum Nutr Diet. 2014;28:41–9.
Leung AYM, Bo A, Hsiao H-Y, Wang SS, Chi I. Health literacy issues in the care of Chinese American immigrants with diabetes: a qualitative study. BMJ Open. 2014;4:e005294.
Altin SV, Finke I, Kautz-Freimuth S, Stock S. The evolution of health literacy assessment tools: a systematic review. BMC Public Health. 2014;14:1207.
A new measurement of acculturation for hispanics: the Bidimensional Acculturation Scale for Hispanics (BAS) – Gerardo Marin, Raymond J. Gamba, 1996 [Internet]. [cited 2019 Sept 28]. Available from: https://journals.sagepub.com/doi/10.1177/07399863960183002
Livaudais-Toman J, Burke NJ, Napoles A, Kaplan CP. Health literate organizations: are clinical trial sites equipped to recruit minority and limited health literacy patients? J Health Dispar Res Pract. 2014;7:1–13.
Acknowledgments
Research reported in this publication was supported by the National Heart, Lung, and Blood Institute of the National Institutes of Health under Award Number T32 HL07779 (Ms. Anderson). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. MESA is a National Institutes of Health (NIH) contract. The NIH was involved in the overall MESA study design and data collection. However the NIH was not involved with the analysis, and interpretation of data; writing the report; and the decision to submit the report for publication. The authors gratefully acknowledge support from the Minnesota Population Center (P2C HD041023) funded through a grant from the Eunice Kennedy Shriver National Institute for Child Health and Human Development (NICHD). This research was supported by contracts HHSN268201500003I, N01-HC-95159, N01-HC-95160, N01-HC-95161, N01-HC-95162, N01-HC-95163, N01-HC-95164, N01-HC-95165, N01-HC-95166, N01-HC-95167, N01-HC-95168 and N01-HC-95169 from the National Heart, Lung, and Blood Institute, and by grants UL1-TR-000040, UL1-TR-001079, and UL1-TR-001420 from the National Center for Advancing Translational Sciences (NCATS). The authors thank the other investigators, the staff, and the participants of the MESA study for their valuable contributions.
A full list of participating MESA investigators and institutions can be found at http://www.mesa-nhlbi.org. No financial disclosures were reported by the authors of this paper.
Funding
No financial disclosures were reported by the authors of this paper. MESA is a National Institutes of Health (NIH) contract. The NIH was involved in the overall MESA study design and data collection. However the NIH was not involved with the analysis, and interpretation of data; writing the report; and the decision to submit the report for publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors have no conflicts of interest to state.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: The typo in author name Susan A. Everson-Rose has been corrected.
Rights and permissions
About this article
Cite this article
Anderson, M.D., Merkin, S.S., Everson-Rose, S.A. et al. Health Literacy Within a Diverse Community-Based Cohort: The Multi-Ethnic Study of Atherosclerosis. J Immigrant Minority Health 23, 659–667 (2021). https://doi.org/10.1007/s10903-020-01123-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10903-020-01123-1