Abstract
Background
Self-Rated Health (SRH) is a valid proxy for individuals’ overall well-being and mortality risk. This study examined contributions of diabetes distress (stress from diabetes self-management) and depressive symptoms to SRH among Chinese Americans with type 2 diabetes (T2DM).
Methods
For this cross-sectional study, a survey measuring diabetes distress, depressive symptoms, physical health, and demographics was administered to a convenience sample of 151 foreign-born community-dwelling Chinese Americans with T2DM.
Results
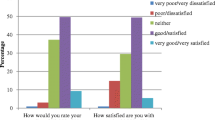
Fifty-five percent of participants rated their health as good or very good. With demographic and physical health variables controlled, hierarchical logistic regression showed that people who reported more diabetes distress (OR = 2.88, p < 0.05) or depressive symptoms (OR = 3.54, p < 0.05) were more likely to have poor SRH. Acculturation (OR = 0.88, p < 0.001) was protective for SRH.
Conclusions
Diabetes distress and depressive symptoms are significantly associated with poor SRH and should be managed in Chinese Americans with T2DM.
Similar content being viewed by others
References
Carpenter R, DiChiacchio T, Barker K. Interventions for self-management of type 2 diabetes: an integrative review. Int J Nurs Sci. 2019;6:70–91. https://doi.org/10.1016/ijns2018.12.002.
Centers for Diabetes Control and Prevention. National Diabetes Statistics Report 2020. https://www.cdc.gov/diabetes/pdfs/data/statistics/national-diabetes-statistics-report.pdf Accessed 8 July 2020.
Kolb H, Martin J. Environmental/lifestyle factors in the pathogenesis and prevention of type 2 diabetes. BMC Med. 2017;15:131–41. https://doi.org/10.1186/s12916-017-0901-x.
United States Bureau of the Census. Asian American and Pacific Islander Heritage Month: May 2020. https://www.census.gov/newsroom/facts-for-features/2020/aian.html Accessed 8 July 2020.
Egede LE, Dismuke CE. Serious psychological distress and diabetes: a review of the literature. Curr Psychiatry Rep. 2012;14(1):15–22.
de Groot M, Anderson R, Freedland KE, Clouse RE, Lustman PJ. Association of depression and diabetes complications: a metaanalysis. Psychosom Med. 2001;63(4):619–30.
Snoek FJ, Bremmer MA, Hermanns N. Constructs of depression and distress in diabetes: time for an appraisal. Lancet Diabetes Endocrinol. 2015;3(6):450–60.
Polonsky WH, Fisher L, Earles J, Dudl RJ, Lees J, Mullan J, Jackson RA. Assessing psychosocial distress in diabetes: development of the diabetes distress scale. Diabetes Care. 2002;8(3):626–31.
Gebel. Diabetes Distress. https://www.diabetes.org/living-with-diabetes/complications/mental-health/diabetes-distress.html?referrer%2520=%2520https://www.google.com/. Accessed 28 March 2019.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders (DSM-5®). Washington, DC: American Psychiatric Pub; 2013.
Ali S, Stone MA, Peters JL, Davies MJ, Khunti K. The prevalence of co-morbid depression in adults with Type 2 diabetes: a systematic review and meta-analysis. Diabet Med. 2006;23(11):1165–73.
Egede LE, Ellis C. Diabetes and depression: global perspectives. Diabetes Res Clin Pract. 2010;87(3):302–12.
Yeung A, Yu SC, Fung F, Vorono S, Fava M. Recognizing and engaging depressed Chinese Americans in treatment in a primary care setting. Int J Geriatr Psychiatry. 2006;21(9):819–23.
Hwang WC, Myers HF, Takeuchi DT. Psychosocial predictors of first-onset depression in Chinese Americans. Soc Psychiatry Psychiatr Epidemiol. 2000;35(3):133–45.
Mak WW, Zane NW. The phenomenon of somatization among community Chinese Americans. Soc Psychiatry Psychiatr Epidemiol. 2004;39(12):967–74.
DeSalvo KB, Bloser N, Reynolds K, He J, Muntner P. Mortality prediction with a single general self-rated health question. J Gen Intern Med. 2006;21(3):267–75.
Assari S, Kumar A. Social determinants of physical self-rated health among Asian Americans. Comp. Six Ethnic Groups Soc. 2018;8(2):1–9.
Jang Y, Huang YC, Yoon H, Lin S. Correlates of self-rated health and self-rated mental health in older Chinese Americans. Soc Work Public Health. 2016;31(4):309–15.
Badawi G, Gariepy G, Pagé V, Schmitz N. Indicators of self-rated health in the Canadian population with diabetes. Diabet Med. 2012;29(8):1021–8.
Dankner R, Olmer L, Kaplan G, Chetrit A. The joint association of self-rated health and diabetes status on 14-year mortality in elderly men and women. Qual Life Res. 2016;25(11):2889–966.
Bulut E, Gayman MD. Acculturation and self-rated mental health among Latino and Asian immigrants in the United States: A latent class analysis. J Immigr Minor Health. 2016;18:836–49.
Jang Y, Kim G, Chiriboga D, King-Kallimanis B. A bidimensional model of acculturation for Korean American older adults. J Aging Stud. 2007;21(3):267–75.
Federal Interagency Forum on Aging-Related Statistics. Older Americans: Key indicators of well-being. https://agingstats.gov/docs/LatestReport/Older-Americans-2016-Key-Indicators-of-WellBeing.pdf. Accessed 22 May 2019.
Fisher L, Hessler DM, Polonsky WH, Mullan J. When is diabetes distress clinically meaningful? Establishing cut points for the diabetes distress scale. Diabetes Care. 2012;35(2):259–64.
Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1(3):385–401.
Zhang Y, Ting RZ, Lam MH, Lam SP, Yeung RO, Nan H, Ozaki R, Luk AO, Kong AP, Wing YK, Sartorius N. Measuring depression with CES-D in Chinese patients with type 2 diabetes: the validity and its comparison to PHQ-9. BMC Psychiatry. 2015;15:1–10.
Corpo IBM. IBM SPSS Statistics for Windows Version- 25.0. Armonk, New York: IBM Corpo; 2017.
Xu Y, Pan W, Liu H. The role of acculturation in diabetes self-management among Chinese Americans with type 2 diabetes. Diabetes Res Clin Pract. 2011;93(3):363–70.
Chang E, Chan KS, Han HR. Effect of acculturation on variations in having a usual source of care among Asian Americans and non-Hispanic whites in California. Am J Public Health. 2015;105(2):398–407.
Chun KM, Chesla CA, Kwan CM. “So We Adapt Step by Step”: acculturation experiences affecting diabetes management and perceived health for Chinese American immigrants. Soc Sci Med. 2011;72(2):256–64.
Deng F, Zhang A, Chan CB. Acculturation, dietary acceptability, and diabetes management among Chinese in North America. Front Endocrinol. (Lausanne). 2013;4:1–7.
Renn BN, Feliciano L, Segal DL. The bidirectional relationship of depression and diabetes: a systematic review. Clin Psychol Rev. 2011;31(8):1239–46.
Lin SY. Beliefs about causes, symptoms, and stigma associated with severe mental illness among ‘highly acculturated’ Chinese-American patients. Int J Soc Psychiatry. 2013;59(8):745–51.
Yang LH, Chen FP, Sia KJ, Lam J, Lam K, Ngo H, Lee S, Kleinman A, Good B. “What matters most:” A cultural mechanism moderating structural vulnerability and moral experience of mental illness stigma. Soc Sci Med. 2014;103:84–93.
Tseng J, Halperin L, Ritholz MD, Hsu WC. Perceptions and management of psychosocial factors affecting type 2 diabetes mellitus in Chinese Americans. J Diabetes Complic. 2013;27(4):383–90.
Chesla CA, Chun KM, Kwan CM. Cultural and family challenges to managing type 2 diabetes in immigrant Chinese Americans. Diabetes Care. 2009;32(10):1812–6.
Xu Y, Pan W, Liu H. Self-management practice of Chinese American with type 2 diabetes. Nurs Health Sci. 2010;12(2):228–34.
Ong WM, Chua SS, Ng CJ. Barriers and facilitators to self-monitoring of blood glucose in people with type 2 diabetes using insulin: a qualitative study. Patient Prefer Adherence. 2014;8:237–46.
Sun F, Gao X, Gao S, Li Q, Hodge DR. Depressive symptoms among older Chinese Americans: examining the role of acculturation and family dynamics. J Gerontol B Psychol Sci Soc Sci. 2016;73(5):870–9.
Acknowledgements
The authors thank all the participants and community organizations that supported and helped with this study.
Funding
The work was supported by the Sigma Theta Tau Epsilon Theta Chapter and the Hogg Foundation for Mental Health (Grant number: FFW-008–17-07).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical Approval
The research design was reviewed and approved by a university institutional review board. Oral consent was obtained from each participant prior to data collection.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Huang, YC., Zuñiga, J., Hua, Y. et al. Emotional Distress and Self-Rated Health Among Middle-Aged and Older Chinese Americans with Type 2 Diabetes. J Immigrant Minority Health 23, 487–493 (2021). https://doi.org/10.1007/s10903-020-01062-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10903-020-01062-x