Abstract
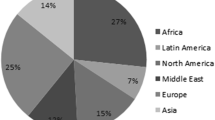
The aim was to explore and compare oral health and need for dental treatment in newly arrived refugees from the Middle East and Africa to Norway. Oral examination and structured interviews were performed with attending interpreters. Associations between origin and measures for oral health were studied with multiple linear regression. Half of the refugees (n = 132) reported oral impacts on daily performances (OIDP) and mean number of decayed teeth (DT) was 4.3 (SD 3.5). Refugees from the Middle East had more DT (1.38, p = 0.044), higher sum of decayed, missing and filled teeth (DMFT) (3.93, p = 0.001) and lower OIDP-score (− 3.72, p = 0.026) than refugees from Africa. Refugee oral health is generally poor, with more extensive challenges in refugees from the Middle East. However, few missing teeth, and manageable caries-gradient at the time of registration indicate that most refugees have the prerequisites for a good dentition, provided they get the necessary treatment.
Similar content being viewed by others
References
United Nations High Commissioner for Refugees (UNHCR). UNHCR chief issues key guidelines for dealing with Europe’s refugee crisis. 2015. http://www.unhcr.org/55e9793b6.html Accessed 8 Nov 2017.
Øzhayat EB, Østergaard P, Gotfredsen K. Oral health-related quality of life in socially endangered persons in Copenhagen, Denmark. Acta Odontol Scand. 2016;74:620–5.
Digital Solutions for Health Personnel (DIPS). Electronic Patient Journal. https://dips.com/no/pasientjournal. Accessed 28 Oct 2017.
Pottie K, Greenaway C, Feightner J, Welch V, Swinkels H, Rashid M, Narasiah L, Kirmayer LJ, Ueffing E, MacDonald NE, Hassan G, McNally M, Khan K, Buhrmann R, Dunn S, Dominic A, McCarthy AE, Gagnon AJ, Rousseau C, Tugwell P, Coauthors of the Canadian Collaboration for Immigrant and Refugee Health. Evidence-based clinical guidelines for immigrants and refugees. CMAJ. 2011;183:E824–97. https://doi.org/10.1503/cmaj.090313.
Ay M, González PA, Delgado RC. The perceived barriers of access to health care among a group of non-camp Syrian refugees in Jordan. Int J Health Serv. 2016;0:1–24.
Van Berlaer G, Carbonell FB, Manantsoa S, de Béthune X, Buyl R, Debacker M, Hubloue I. A refugee camp in the centre of Europe: clinical characteristics of asylum seekers arriving in Brussels. BMJ Open. 2016;6:e013963. https://doi.org/10.1136/bmjopen-2016-013963.
Ghiabi E, Matthews DC, Brillant MS. The oral health status of recent immigrants and refugees in Nova Scotia. Canada J Immigr Minor Health. 2014;16:95–101.
Willis MS, Bothun RM. Oral hygiene knowledge and practice among Dinka and Nuer from Sudan to the U.S. J Dent Hyg. 2011;85:306–15.
Davidson N, Skull S, Calache H, Murray SS, Chalmers J. Holes a plenty: oral health status a major issue for newly arrived refugees in Australia. Aust Dent J. 2006;51:306–11.
Mattila A, Ghaderi P, Tervonen L, Niskanen L, Pesonen P, Anttonen V, Laitala ML. Self-reported oral health and use of dental services among asylum seekers and immigrants in Finland—a pilot study. Eur J Public Health. 2016;26:1006–10.
Keboa MT, Hiles N, Macdonald ME. The oral health of refugees and asylum seekers: a scoping review. Globalization Health. 2016;12:59. https://doi.org/10.1186/s12992-016-0200-x.
Saltaji H. Oral health consequences of the crisis in Syria. Br Dent J. 2015;219:49.
Lightfoot E, Blevins J, Lum T, Dube A. Cultural health assets of Somali and Oromo refugees and immigrants in Minnesota: Findings from a community-based participatory research project. J Health Care Poor Underserved. 2016;27:252–60.
Geltman PL, Adams JH, Cochran J, Doros G, Rybin D, Henshaw M, Barnes LL, Paasche-Orlow M. The impact of functional health literacy and acculturation on the oral health status of Somali refugees living in Massachusetts. Am J Public Health. 2013;103:1516–23.
Adams JH, Young S, Laird LD, Geltman PL, Cochran JJ, Hassan A, Egal F, Paasche-Orlow MK, Barnes LL. The cultural basis for oral health practices among Somali refugees pre- and post-resettlement in Massachusetts. J Health Care Poor Underserved. 2013;24:1474–85.
Abid A, Maatouk F, Berrezouga L, Azodo C, Uti O, El-Shamy H, Oginni A. Prevalence and severity of oral diseases in the Africa and Middle East Region. Adv Dent Res. 2015;27:10–7.
The Norwegian Directorate of Immigration (UDI). RS 2011-044. Fordeling av asylsøkere fra transittmottak til ordinære mottak. (Distribution of asylum seekers from transit to ordinary reception centers). https://www.udiregelverk.no/no/rettskilder/udi-rundskriv/re-2011-044/. Accessed 8 March 2017.
The Norwegian Directorate of Immigration (UDI). Fact sheet 2015. https://www.udi.no/en/statistics-and-analysis/annual-reports/tall-og-fakta-2015/faktaskriv-2015/. Accessed 5 Dec 2017.
Salita Interpretation- and translation services. Tolke- og translatørtjeneste AS. https://www.salita.no.
Singh HK, Henshaw M, Cote SE, Grodin MA, Piwowarczyk LA. Oral health status of refugee torture survivors seeking care in the United States. Am J Public Health. 2008;98:2181–2.
Aduyanon S, Sheiham A. Oral Impacts on daily performance. In: Slade GD, ed. Measuring oral health and quality of life. Chapel Hill: Univ North Carolina; 1997. p. 151–60.
Åstrøm AN, Haugejorden O, Skaret E, Tronvik TA, Klock KS. Oral impacts on daily performances in Norwegian adults: Validity, reliability and prevalence estimates. Eur J Oral Sci. 2005;113:289–96.
Pani SC, Al-Sibai SA, Rao AS, Kazimoglu SN, Mosadomi HA. Parental perception of oral health-related quality of life in Syrian refugee children. J Int Soc Prev Community Dent. 2017;7:191–6.
Mishori R, Aleinikoff S, Davis D. Primary care for refugees: challenges and opportunities. Am Fam Physician. 2017;96:112–20.
World Health Organization (WHO). WHO’s oral health country/area profile programme (CAPP) database. 2013. http://www.mah.se/CAPP/Country-Oral-Health-Profiles. Accessed 14 March 2017.
Lagerweij MD, van Loveren C. Declining caries trends: are we satisfied? Curr Oral Health Rep. 2015;2:212–7.
Holst D, Schuller AA. Equality in adults’ oral health in Norway. Cohort and cross-sectional results over 33 years. Community Dent Oral Epidemiol. 2011;39:488–97.
Sheiham A, Williams DM. Reducing inequalities in oral health in the Africa and Middle East region. Adv Dent Res. 2015;27:4–9.
Fawell J, Bailey K, Chilton J, Dahi E, Fewtrell L, Magara Y. Fluoride in drinking-water. World Health Organization. London: IWA Publishing; 2006. pp. 97–117.
Acknowledgements
The authors would like to thank the Norwegian Directorate of Immigration, particularly the personnel at the reception centers Bjørnebekk, Bærum, Dikemark, Drammen, Hobøl, Moss, Skedsmo and Tønsberg. This research received no specific grant from any funding agency, but interpretation services were supported by the Norwegian Directory of Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Norwegian Ethics Committee and with the 1964 Helsinki declaration and its later amendments.
Rights and permissions
About this article
Cite this article
Høyvik, A.C., Lie, B., Grjibovski, A.M. et al. Oral Health Challenges in Refugees from the Middle East and Africa: A Comparative Study. J Immigrant Minority Health 21, 443–450 (2019). https://doi.org/10.1007/s10903-018-0781-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10903-018-0781-y