Abstract
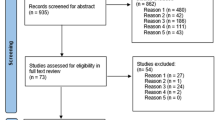
To examine two healthcare models, specifically “Primary Medical Care” (PMC) and “Primary Health Care” (PHC) in the context of immigrant populations’ health needs. We conducted a systematic scoping review of studies that examined primary care provided to immigrants. We categorized studies into two models, PMC and PHC. We used subjects of access barriers and preventive interventions to analyze the potential of PMC/PHC to address healthcare inequities. From 1385 articles, 39 relevant studies were identified. In the context of immigrant populations, the PMC model was found to be more oriented to implement strategies that improve quality of care of the acute and chronically ill, while PHC models focused more on health promotion and strategies to address cultural and access barriers to care, and preventive strategies to address social determinants of health. Primary Health Care models may be better equipped to address social determinants of health, and thus have more potential to reduce immigrant populations’ health inequities.

Similar content being viewed by others
References
Pottie K, Greenaway C, Feightner J, et al. Evidence-based clinical guidelines for immigrants and refugees. CMAJ. 2011;183(12):E824–925.
McDonald J, Kennedy S. Insights into the ‘healthy immigrant effect’: health status and health service use of immigrants to Canada. Soc Sci Med. 2004;59(8):1613–27.
Hyman I, Jackson B. The healthy immigrant effect: a temporary phenomenon? Health Policy Res Bull. 2010;17:17–21.
Fuller-Thomson E, Noack AM, George U. Health decline among recent immigrants to Canada: findings from a nationally-representative longitudinal survey. Can J Public Health. 2011;102(4):273–80.
Gee EM, Kobayashi KM, Prus SG. Examining the healthy immigrant effect in mid- to later life: findings from the Canadian Community Health Survey. Can J Aging. 2004;23(Suppl 1):S61–9.
Choi SH. Testing healthy immigrant effects among late life immigrants in the United States: using multiple indicators. J Aging Health. 2012;24(3):475–506.
Stanciole AE, Huber M. Access to health care for migrants, ethnic minorities, and asylum seekers in Europe. Vienna: European Centre for Social Welfare Policy and Research; 2009.
Joshi C, Russell G, Cheng I-H, et al. A narrative synthesis of the impact of primary health care delivery models for refugees in resettlement countries on access, quality and coordination. Int J Equity Health. 2013;12(1):88.
Whitehead M. The concepts and principles of equity and health. Copenhagen: World Health Organization Regional Office for Europe; 1990.
Tugwell P, Robinson V, Morris E. Mapping global health inequalities: challenges and opportunities. Santa Cruz: Center for Global, International and Regional Studies, UC Santa Cruz; 2007.
Lebrun LA, Dubay LC. Access to primary and preventive care among foreign-born adults in Canada and the United States. Health Serv Res. 2010;45(6 Pt 1):1693–719.
Derose KP, Bahney BW, Lurie N, Escarce JJ. Review: immigrants and health care access, quality, and cost. Med Care Res Rev. 2009;66(4):355–408.
Pottie K, Ng E, Spitzer D, Mohammed A, Glazier R. Language proficiency, gender and self-reported health: an analysis of the first two waves of the longitudinal survey of immigrants to Canada. Can J Public Health. 2008;99(6):505–10.
Tudor Hart J. The inverse care law. Lancet. 1971;297(7696):405–12.
Simich L. Health literacy and immigrant populations. Ottawa: Public Health Agency of Canada and Metropolis Canada; 2009.
Pottie K, Dahal G, Georgiades K, Premji K, Hassan G. Do first generation immigrant adolescents face higher rates of bullying, violence and suicidal behaviours than do third generation and native born? J Immigr Minor Health. 2015;17(5):1557–66. doi:10.1007/s10903-014-0108-6.
Clough J, Lee S, Chae DH. Barriers to health care among Asian immigrants in the United States: a traditional review. J Health Care Poor Underserved. 2013;24(1):384–403.
Chauvin P, Simonnot N. Access to health care for vulnerable groups in the European Union in 2012. Médecins du monde; 2012.
Harris MF. Access to preventive care by immigrant populations. BMC Med. 2012;10:55.
Muldoon LK, Hogg WE, Levitt M. Primary care (PC) and primary health care (PHC): what is the difference? Can J Public Health. 2006;97(5):409–11.
Egwu IN. Primary is not the same as primary health care, or is it? Fam Community Health. 1984;7(3):83–8.
Awofeso N. What is the difference between “primary care” and “primary healthcare”? Qual Prim Care. 2004;12:93–4.
Barnes D, Eribes C, Juarbe T, et al. Primary health care and primary care: a confusion of philosophies. Nurs Outlook. 1995;43(1):7–16.
WHO. Primary health care: now more than ever. The world health report 2008. Geneva: World Health Organization; 2008.
Meads G. Primary health care models: learning across continents. Prim Health Care Res Dev. 2006;7(04):281–3.
Lamarche PA, Beaulieu M-D, Pineault R, Contandriopoulos A-P, Denis J-L, Haggerty J. Choices for change: the path for restructuring primary healthcare services in Canada. Ottawa: Canadian Health Services Research Foundation; 2003.
Haggerty J, Burge F, Lévesque J-F, et al. Operational definitions of attributes of primary health care: consensus among Canadian experts. Ann Fam Med. 2007;5(4):336–44.
Samaan Z, Mbuagbaw L, Kosa D, et al. A systematic scoping review of adherence to reporting guidelines in health care literature. J Multidiscip Healthc. 2013;6:169–88.
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32.
iCAHE. Critical appraisal tools. Critical appraisal skills programme (CASP). http://w3.unisa.edu.au/cahe/Resources/CALibrary/default.asp.
NCCMT. Quality assessment tool for quantitative studies. 1998. http://www.nccmt.ca/registry/view/eng/14.html. Accessed 2 Aug 2013.
Tugwell P, Petticrew M, Kristjansson E, et al. Assessing equity in systematic reviews: realising the recommendations of the Commission on Social Determinants of Health. BMJ. 2010;341:873–7.
Ciliska D, Thomas H, Buffett C. An introduction to evidence-informed public health and a compendium of critical appraisal tools for public health practice. Hamilton: McMaster University; 2010.
Kmet LM, Lee RC, Cook LS. Standard quality assessment criteria for evaluating primary research papers from a variety of fields. Edmonton: Alberta Heritage Foundation for Medical Research; 2004.
Gale NK, Heath G, Cameron E, Rashid S, Redwood S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol. 2013;13(1):1–8.
Scheppers E, van Dongen E, Dekker J, Geertzen J, Dekker J. Potential barriers to the use of health services among ethnic minorities: a review. Fam Pract. 2006;23(3):325–48.
Pitkin Derose K, Bahney BW, Lurie N, Escarce JJ. Review: immigrants and health care access, quality, and cost. Med Care Res Rev. 2009;66(4):355–408.
Derose KP, Escarce JJ, Lurie N. Immigrants and health care: sources of vulnerability. Health Aff (Millwood). 2007;26(5):1258–68.
Access Alliance. Racialized groups and health status: a literature review exploring poverty, housing, race-based discrimination and access to health care as determinants of health for racialized groups. Access Alliance Multicultural Health and Community Services; 2005.
McKeary M, Newbold B. Barriers to Care: The challenges for canadian refugees and their health care providers. J Refugee Stud. 2010;23(4):523–45.
AFMC. Basic concepts in prevention, surveillance, and health promotion: the stages of prevention. In: Donovan D, McDowell I, Hunter D, editors. AFMC primer on population health: the association of faculties of medicine of canada public health educators’ network; 2010.
Solar O, Irwin A. A conceptual framework for action on the social determinants of health. Geneva: World Health Organization; 2010.
Telleen S, Rhee Kim YO, Chavez N, Barrett RE, Hall W, Gajendra S. Access to oral health services for urban low-income Latino children: social ecological influences. J Public Health Dent. 2012;72(1):8–18.
Singh-Franco D, Perez A, Wolowich WR. Improvement in surrogate endpoints by a multidisciplinary team in a mobile clinic serving a low-income, immigrant minority population in South Florida. J Health Care Poor Underserved. 2013;24(1):67–77.
Aragones A, Schwartz MD, Shah NR, Gany FM. A randomized controlled trial of a multilevel intervention to increase colorectal cancer screening among Latinos immigrants in a primary care facility. J Gen Intern Med. 2010;25(6):564–7.
Taylor VM, Yasui Y, Nguyen TT, et al. Pap smear receipt among Vietnamese immigrants: the importance of health care factors. Ethn Health. 2009;14(6):575–89.
Belue R, Degboe AN, Miranda PY, Francis LA. Do medical homes reduce disparities in receipt of preventive services between children living in immigrant and non-immigrant families? J Immigr Minor Health. 2012;14(4):617–25.
De Jonge A, Rijnders M, Agyemang C, et al. Limited midwifery care for undocumented women in the Netherlands. J Psychosom Obstet Gynecol. 2011;32(4):182–8.
Guruge S, Hunter J, Barker K, McNally MJ, Magalhaes L. Immigrant women’s experiences of receiving care in a mobile health clinic. J Adv Nurs. 2010;66(2):350–9.
Baarnhielm S, Ekblad S. Turkish migrant women encountering health care in Stockholm: a qualitative study of somatization and illness meaning. Cult Med Psychiatry. 2000;24(4):431–52.
Jensen NK, Norredam M, Priebe S, Krasnik A. How do general practitioners experience providing care to refugees with mental health problems? a qualitative study from Denmark. BMC Fam Pract. 2013;14:17.
Kim MJ, Cho HI, Cheon-Klessig YS, Gerace LM, Camilleri DD. Primary health care for Korean immigrants: sustaining a culturally sensitive model. Public Health Nursing (Boston Mass). 2002;19(3):191–200.
Kirmayer LJ, Narasiah L, Munoz M, et al. Common mental health problems in immigrants and refugees: general approach in primary care. CMAJ. 2011;183(12):E959–67.
Kaltman S, Pauk J, Alter CL. Meeting the mental health needs of low-income immigrants in primary care: a community adaptation of an evidence-based model. Am J Orthopsychiatry. 2011;81(4):543–51.
Kwong K, Chung H, Cheal K, Chou J, Chen T. Depression care management for Chinese Americans in primary care: a feasibility pilot study. Community Ment Health J. 2013;49(2):157–65.
Ahmed SM, Lemkau JP. Cultural issues in the primary care of South Asians. J Immigr Health. 2000;2(2):89–96.
Fowler N. Providing primary health care to immigrants and refugees: the North Hamilton experience. CMAJ. 1998;159(4):388–91.
Frank AL, Liebman AK, Ryder B, Weir M, Arcury TA. Health care access and health care workforce for immigrant workers in the agriculture, forestry, and fisheries sector in the southeastern US. Am J Ind Med. 2013;56(8):960–74.
Morrison SD, Haldeman L, Sudha S, Gruber KJ, Bailey R. Cultural adaptation resources for nutrition and health in new immigrants in central North Carolina. J Immigr Minor Health. 2007;9(3):205–12.
Blewett LA, Casey M, Call KT. Improving access to primary care for a growing Latino population: the role of safety net providers in the rural Midwest. J Rural Health. 2004;20(3):237–45.
Isaacs S, Valaitis R, Newbold KB, Black M, Sargeant J. Brokering for the primary healthcare needs of recent immigrant families in Atlantic, Canada. Prim Health Care Res Dev. 2013;14(1):63–79.
Chin JJ, Kang E, Kim JH, Martinez J, Eckholdt H. Serving Asians and Pacific Islanders with HIV/AIDS: challenges and lessons learned. J Health Care Poor Underserved. 2006;17(4):910–27.
Abreu M, Hynes P. The Latino Health Insurance Program: a pilot intervention for enrolling latino families in health insurance programs, East Boston, Massachusetts, 2006–2007. Prev Chronic Dis. 2009;6(4):A129.
Isralowitz RE. Vision change and quality of life among Ethiopian elderly immigrants in Israel. J Gerontol Soc Work. 2000;33(1):89–96.
De Jesus Diaz-Perez M, Farley T, Cabanis CM. A program to improve access to health care among Mexican immigrants in rural Colorado. J Rural Health. 2004;20(3):258–64.
Levin-Zamir D, Keret S, Yaakovson O, et al. Refuah shlema: a cross-cultural programme for promoting communication and health among ethiopian immigrants in the primary health care setting in Israel evidence and lessons learned from over a decade of implementation. Global Health Promot. 2011;18(1):51–4.
Ramos RL, Hernandez A, Ferreira-Pinto JB, Ortiz M, Somerville GG. Promovision: designing a capacity-building program to strengthen and expand the role of promotores in HIV prevention. Health Promot Pract. 2006;7(4):444–9.
Gould G, Viney K, Greenwood M, Kramer J, Corben P. A multidisciplinary primary healthcare clinic for newly arrived humanitarian entrants in regional NSW: model of service delivery and summary of preliminary findings. Aust N Z J Public Health. 2010;34(3):326–9.
Carrillo JE, Shekhani NS, Deland EL, et al. A regional health collaborative formed By NewYork-Presbyterian aims to improve the health of a largely Hispanic community. Health Aff (Millwood). 2011;30(10):1955–64.
Lofvander M, Dyhr L. Transcultural general practice in Scandinavia. Scand J Prim Health Care. 2002;20(1):6–9.
Ku L. Improving health insurance and access to care for children in immigrant families. Ambul Pediatr. 2007;7(6):412–20.
WHO. International migration, health and human rights. Geneva: WHO; 2003.
Tapp H, Smith HA, Dixon JT, Ludden T, Dulin M. Evaluating primary care delivery systems for an uninsured hispanic immigrant population. Fam Community Health. 2013;36(1):19–33.
Lyberg A, Viken B, Haruna M, Severinsson E. Diversity and challenges in the management of maternity care for migrant women. J Nurs Manag. 2012;20(2):287–95.
McElmurry BJ, Park CG, Buseh AG. The nurse-community health advocate team for urban immigrant primary health care. J Nurs Scholarsh. 2003;35(3):275–81.
Priebe S, Sandhu S, Dias S, et al. Good practice in health care for migrants: views and experiences of care professionals in 16 European countries. BMC Public Health. 2011;11:187.
Sim S-C, Peng C. Lessons learned from a program to sustain health coverage after September 11 in New York City’s Chinatown. New York: Asian American Federation of New York; 2004.
Marques TV. Refugees and migrants struggle to obtain health care in Europe. CMAJ. 2012;184(10):E531–2.
Muggah E, Dahrouge S, Hogg W. Access to primary health care for immigrants: results of a patient survey conducted in 137 primary care practices in Ontario, Canada. BMC Fam Pract. 2012;13(1):128–34.
Comino E, Davies G, Krastev Y, et al. A systematic review of interventions to enhance access to best practice primary health care for chronic disease management, prevention and episodic care. BMC Health Serv Res. 2012;12(1):415.
Baker R, Willars J, McNicol S, Dixon-Woods M, McKee L. Primary care quality and safety systems in the English National Health Service: a case study of a new type of primary care provider. J Health Serv Res Policy. 2014;19(1):34–41.
Pottie K, Hadi A, Chen J, Welch V, Hawthorne K. Realist review to understand the efficacy of culturally appropriate diabetes education programmes. Diabet Med. 2013;30(9):1017–25.
IOM. Migration initiatives 2013 in support of development. Geneva: International Organization for Migration; 2013.
WHO. Health of migrants: the way forward. Geneva: World Health Organization; 2010.
Cabieses B, Tunstall H, Pickett KE, Gideon J. Understanding differences in access and use of healthcare between international immigrants to Chile and the Chilean-born: a repeated cross-sectional population based study in Chile. Int J Equity Health. 2012;11(68):16.
Han G-S, Davies C. Ethnicity, Health and Medical Care: Towards a critical realist analysis of general practice in the Korean community in Sydney. Ethn Health. 2006;11:409–30.
Kantayya VS, Lidvall SJ. Community health centers: disparities in health care in the United States 2010. Dis Mon. 2010;56(12):681–97.
Nerad S, Janczur A. Primary health care with immigrant and refugee populations. Issues and challenges. Aust J Prim Health. 2000;6(4):222–9.
Shah CP, Moloughney BW. A strategic review of the community health centre program. Ontario: Ministry of Health and Long-Term Care; 2001.
Glazier RH, Zagorski BM, Rayner J. Comparison of primary care models in Ontario by demographics, case mix and emergency department use, 2008/09 to 2009/10. Toronto: Institute for Clinical Evaluative Sciences; 2012.
Shi L, Lee D-C, Liang H, et al. Community health centers and primary care access and quality for chronically-ill patients—a case-comparison study of urban Guangdong Province, China. Int J Equity Health. 2015;14(1):90.
Kawachi I, Kennedy BP, Lochner K, Prothrow-Stith D. Social capital, income inequality, and mortality. Am J Public Health. 1997;87(9):1491–8.
Gilbert J, van Kemenade S. Social capital and health: maximizing the benefits. In: Gilbert J, van Kemenade S, editors. Applied research and analysis directorate HPB, trans. Health policy research bulletin, vol 12. Ottawa: Health Canada; 2006.
Gilbert KL, Quinn SC, Goodman RM, Butler J, Wallace J. A meta-analysis of social capital and health: a case for needed research. J Health Psychol. 2013;18(11):1385–99.
Bouchard L, Roy JF, Van Kemenade S. Research traditions: an overview. Ottawa: Health Canada; 2006.
van Kemenade S, Roy JF, Bouchard L. Social networks and vulnerable populations: findings from the GSS. In: Gilbert J, van Kemenade S, editors. Health policy research bulletin. Vol social capital and health: maximizing the benefits. Ottawa: Health Canada; 2006. pp. 16–20.
WHO Europe. How health systems can address health inequities linked to migration and ethnicity. Copenhagen: WHO Regional Office for Europe; 2010.
WHO-CSDH. Closing the gap in a generation: health equity through action on the social determinants of health. Final report of the commission on social determinants of health. Geneva: World Health Organization; 2008.
Rasanathan K, Montesinos EV, Matheson D, Etienne C, Evans T. Primary health care and the social determinants of health: essential and complementary approaches for reducing inequities in health. J Epidemiol Community Health. 2011;65(8):656–60.
Ramírez NA, Ruiz JP, Romero RV, Labonté R. Comprehensive primary health care in South America: contexts, achievements and policy implications. Cadernos de Saúde Pública. 2011;27:1875–90.
Labonté R, Sanders D, Packer C, Schaay N. Is the Alma Ata vision of comprehensive primary health care viable? Findings from an international project. Global Health Action. 2014;7:16.
IOM. Glossary on migration. Geneva: International Organization for Migration; 2004.
WHO. A glossary of terms for community health care and services for older persons. Geneva: World Health Organization; 2004.
WHO-UNICEF. Declaration of Alma-Ata. International conference on primary health care, Sept 6–12, 1978, Alma-Ata, USSR.
Muldoon L, Dahrouge S, Hogg W, Geneau R, Russell G, Shortt M. Community orientation in primary care practices: results from the comparison of models of primary health care in Ontario study. Can Fam Physician. 2010;56:676–83.
Longlett SK, Kruse JE, Wesley RM. Community-oriented primary care: historical perspective. J Am Board Fam Pract. 2001;14(1):54–63.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declared no conflicts of interest with respect to the research, authorship, and/or publication of this article.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Batista, R., Pottie, K., Bouchard, L. et al. Primary Health Care Models Addressing Health Equity for Immigrants: A Systematic Scoping Review. J Immigrant Minority Health 20, 214–230 (2018). https://doi.org/10.1007/s10903-016-0531-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10903-016-0531-y