Abstract
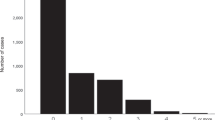
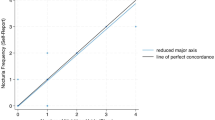
Although widely viewed as a urological condition, nocturia has been increasingly recognized to accompany various non-urological conditions such as hypertension and blood pressure (BP) elevation on office determination. Home BP monitoring (HBPM) has been shown superior to office-based readings and provides an opportunity to assess potential relationships between nocturia and novel indices derived from multiple BP recordings including BP load, BP variability, and arterial stiffness, which have prognostic significance. We retrospectively studied 103 home BP logs and nocturia frequencies provided by 61 stable cardiology patients ≥ 21 years without medication change. Nocturnal voids ranged from 0 to 5 voids per night, median: 1.5. Nocturia frequency was significantly correlated with home and office systolic BPs and with BP load, but not with diastolic BPs, BP variability or arterial stiffness. On Poisson regression analysis, the estimated prevalence ratio (PR) for home and office systolic BPs were 1.025 (CI: 1.01, 1.04; p < .001) and 1.01 (CI:1.00, 1.02; p = .019), indicating 2.5% and 1% increases in the risk of nocturia per mmHg increases in BP respectively. In conclusion, higher mean home and office systolic BPs are associated with self-reported nocturia frequency with stronger associations seen for home BP measurement. Nocturia frequency appears unrelated to mean home and office diastolic BPs. Nocturia may be related to BP load, (percentage of elevated BP values), but not to BP variability or arterial stiffness. Future prospective studies using HBPM are needed to confirm these findings and to contribute to the understanding of the elevated BP-nocturia link.
Similar content being viewed by others
Availability of data and material (data transparency)
Not applicable.
References
Weiss, J. P., Monaghan, T. F., Epstein, M. R., & Lazar, J. M. (2019). Future considerations in nocturia and nocturnal polyuria. Urology, 133S, 34–42.
Everaert, K., Herve, F., Bosch, R., et al. (2019). International Continence Society consensus on the diagnosis and treatment of nocturia. Neurourology And Urodynamics, 38(2), 478–498.
Bliwise, D. L., Wagg, A., & Sand, P. K. (2019). Nocturia: A highly prevalent disorder with multifaceted consequences. Urology, 33, 3–13.
Vaughan, C. P., Brown, C. J., Goode, P. S., Burgio, K. L., Allman, R. M., & Johnson, T. M. 2 (2010). The association of nocturia with incident falls in an elderly community-dwelling cohort. International Journal Of Clinical Practice, 64(5), 577–583. https://doi.org/10.1111/j.1742-1241.2009.02326.x PMID: 20456212; PMCID: PMC3222329.
Declerck, V., De Backer, T., Pauwaert, K., et al. (2022). De novo nocturia: A red flag for coronary heart disease patients. Progres En Urologie, 32(11), 756–762. https://doi.org/10.1016/j.purol.2022.05.005 Epub 2022 Jun 27. PMID: 35773176.
Gulur, D. M., Mevcha, A. M., & Drake, M. J. (2011). Nocturia as a manifestation of systemic disease. Bju International, 107(5), 702–713.
Feldstein, C. A. (2013). Nocturia in arterial hypertension: a prevalent, underreported, and sometimes underestimated association. J Am Soc Hypertens, 7(1), 75–84.
Rahman, S. N., Cao, D. J., Monaghan, T. F., et al. (2021). Phenotyping the association between nocturia and hypertension: A systematic review and meta-analysis. Journal Of Urology, 205(6), 1577–1583. https://doi.org/10.1097/JU.0000000000001433 Epub 2020 Oct 20. PMID: 33081593.
Victor, R. G., Li, N., Blyler, C. A., et al. (2019). Nocturia as an unrecognized symptom of uncontrolled hypertension in Black men aged 35 to 49 Years. J Am Heart Assoc, 8(5), e010794.
Saito, S., Asayama, K., Ohkubo, T., et al. (2004). The second progress report on the Hypertension Objective treatment based on Measurement by Electrical Devices of Blood Pressure (HOMED-BP) study. Blood Press Monit, 9(5), 243–247.
Muntner, P., Carey, R. M., Jamerson, K., Wright, J. T. Jr., & Whelton, P. K. (2019). Rationale for ambulatory and home blood pressure monitoring thresholds in the 2017 American College of Cardiology/American Heart Association Guideline. Hypertension, 73(1), 33–38.
Booth, J. N. 3rd, Hubbard, D., Sakhuja, S., et al. (2019). Proportion of US adults recommended out-of-clinic blood pressure monitoring according to the 2017 hypertension clinical practice guidelines. Hypertension, 74(2), 399–406.
Shimbo, D., Artinian, N. T., Basile, J. N., et al. (2020). American Heart Association and the American Medical Association. self-measured blood pressure monitoring at home: A joint policy statement from the American Heart Association and American Medical Association. Circulation. ;142(4):e42-e63. https://doi.org/10.1161/CIR.0000000000000803 Epub 2020 Jun 22. Erratum in: Circulation. 2020;142(4):e64. PMID: 32567342.
Imai, Y., Ohkubo, T., Sakuma, M., et al. (1996). Predictive power of screening blood pressure, ambulatory blood pressure and blood pressure measured at home for overall and cardiovascular mortality: a prospective observation in a cohort from Ohasama, northern Japan. Blood Press Monit, 1(3), 251–254.
Vaur, L., Dubroca, I. I., Dutrey-Dupagne, C., et al. (1998). Superiority of home blood pressure measurements over office measurements for testing antihypertensive drugs. Blood Press Monit, 3(2), 107–114.
Bliziotis, I. A., Destounis, A., & Stergiou, G. S. (2012). Home versus ambulatory and office blood pressure in predicting target organ damage in hypertension: a systematic review and meta-analysis. Journal Of Hypertension, 30, 1289–1299. https://doi.org/10.1097/HJH.0b013e3283531eaf.
Shimbo, D., Pickering, T. G., Spruill, T. M., Abraham, D., Schwartz, J. E., & Gerin, W. (2007). Relative utility of home, ambulatory, and office blood pressures in the prediction of end-organ damage. American Journal Of Hypertension, 20(5), 476–482.
Umemura, S., Arima, H., Arima, S., et al. The Japanese Society of Hypertension guidelines for the management of hypertension (JSH 2019).Hypertens Res; 42(9):1235–1481.
Stergiou, G. S., Ntineri, A., Kollias, A., Ohkubo, T., Imai, Y., & Parati, G. (2014). Blood pressure variability assessed by home measurements: a systematic review. Hypertension Research, 37(6), 565–572. https://doi.org/10.1038/hr.2014.2 Epub 2014 Feb 20. PMID: 24553366.
Steven, S. L., Wood, S., Koshiaris, C., et al. (2016). Blood pressure variability and cardiovascular disease: systematic review and meta-analysis. Bmj, 354, i4098.
Parati, G., Stergiou, G. S., Dolan, E., & Bilo, G. (2018). Blood pressure variability: clinical relevance and application. J Clin Hypertens (Greenwich). ;20(7):1133–1137. https://doi.org/10.1111/jch.13304. PMID: 30003704.
Qureshi, G., Salciccioli, L., Clark, L. T., et al. (2008). Home blood pressure monitoring in an ethnically diverse inner-city cardiology practice. Ethnicity And Disease, 18(1), 37–41.
Qureshi, G., Lazar, J. M., Javaid, H., Weber, M., & Salciccioli, L. (2007t). Self-measured (blood pressure) arterial stiffness index: A promising new measure of arterial stiffness. J Am Soc Hypertens, 1(5), 347–352. https://doi.org/10.1016/j.jash.2007.05.005.PMID. : 20409865.
Reboldi, G., Angeli, F., & Verdecchia, P. (2014). Interpretation of ambulatory blood pressure profile for risk stratification keep it simple hypertension. ;63:913–914.
Fatani, N., Dixon, D., Van Tassell, B., et al. (2021). Systolic blood pressure time in target range and cardiovascular outcomes in patients with hypertension. Journal Of The American College Of Cardiology, 77(10), 1290–1299. https://doi.org/10.1016/j.jacc.2021.01.01423.
Stergiou, G. S., Palatini, P., Parati, G., et al. (2021). 2021 European Society of Hypertension practice guidelines for office and out-of-office blood pressure measurement. J Hypertens. ;39(7):1293–1302. https://doi.org/10.1097/HJH.0000000000002843. PMID: 33710173.
Adji, A., O’Rourke, M. F., & Namasivayam, M. (2011). Arterial stiffness, its assessment, prognostic value, and implications for treatment. American Journal Of Hypertension, 24(1), 5–17. https://doi.org/10.1038/ajh.2010.192 Epub 2010 Sep 9. PMID: 20940710.
Li, Y., Wang, J. G., Dolan, E., et al. (2006). Ambulatory arterial stiffness index derived from 24-hour ambulatory blood pressure monitoring. Hypertens, 47(3), 359–364.
Kikuya, M., Ohkubo, T., Satoh, M., et al. (2012). Prognostic significance of home arterial stiffness index derived from self-measurement of blood pressure: the Ohasama Study. American Journal Of Hypertension, 25(1), 67–73. https://doi.org/10.1038/ajh.2011.167 Epub 2011 Sep 29. PMID: 21956526.
Anwar, Y. A., Tendler, B. E., McCabe, E. J., Mansoor, G. A., & White, W. B. (1997). Evaluation of the Datascope Accutorr Plus according to the recommendations of the Association for the Advancement of Medical Instrumentation. Blood Press Monit, 2(2), 105–110.
Siniorakis, E., Kotsanis, A., Kanderakis, S., Exarchos, S., & Kapiris, I. (2008). Nocturia in males with heart failure: prostatic edema and circadian neurohormonal rhythm. International Journal Of Cardiology, 24(123), 3:361–363.
Mekki, P., Monaghan, T. F., Lee, L., et al. (2021). Nocturia and electrocardiographic abnormalities among patients at an inner-city cardiology clinic. Neurourology And Urodynamics, 40(1), 509–514. https://doi.org/10.1002/nau.24590 Epub 2020 Dec 21. PMID: 33348456.
Lombardo, R., Tubaro, A., & Burkhard, F. (2020). Nocturia: the complex role of the heart, kidneys, and bladder. Eur Urol Focus. ;6(3):534–536. https://doi.org/10.1016/j.euf.2019.07.007. Epub 2019 Aug 5. PMID: 31395515.
Ohishi, M., Kubozono, T., Higuchi, K., & Akasaki, Y. (2021). Hypertension, cardiovascular disease, and nocturia: a systematic review of the pathophysiological mechanisms. Hypertens Res. ;44(7):733–739. https://doi.org/10.1038/s41440-021-00634-0. Epub 2021 Mar 3. PMID: 33654248.
Stergiou, G. S., Baibas, N. M., Gantzarou, A. P., et al. (2002). Reproducibility of home, ambulatory, and clinic blood pressure: implications for the design of trials for the assessment of antihypertensive drug efficacy. Am J Hypertens. ;15(2 Pt 1):101–104. https://doi.org/10.1016/s0895-7061(01)02324-x. PMID: 11863243.
Sugaya, K., Nakada, S., Simoji, T., Odaguchi, N., Nakamoto, M., & Nakazato, S. (2009). Relationship between blood pressure and nocturia in hypertensive patients. LUTS, 1, 16–35.
Graugaard-Jensen, C., Rittig, S., & Djurhuus, J. C. (2006). Nocturia and circadian blood pressure profile in healthy elderly male volunteers. J Urol. ;176(3):1034–1039. https://doi.org/10.1016/j.juro.2006.04.046. PMID: 16890685.
Matsumoto, T., Tabara, Y., Murase, K., et al. (2018). Nocturia and increase in nocturnal blood pressure: the Nagahama study. J Hypertens. ;36(11):2185–2192. https://doi.org/10.1097/HJH.0000000000001802. PMID: 29846331.
Matzkin, H., Greenstein, A., Prager-Geller, T., Sofer, M., & Braf, Z. (1996). Do reported micturition symptoms on the American Urological Association Questionnaire correlate with 24-hour home uroflowmetry recordings? Journal Of Urology, 155(1), 197–199. PMID: 7490832.
Reynard, J. M., Cannon, A., Yang, Q., & Abrams, P. (1998). A novel therapy for nocturnal polyuria: a double-blind randomized trial of furosemide against placebo. British Journal Of Urology, 81, 215–218.
Mock, L. L., Parmelee, P. A., Kutner, N., et al. (2008). Content validation of symptom-specific nocturia quality-of-life instrument developed in men: issues expressed by women, as well as men. Urology, 72(4), 736–742.
Abraham, L., Hareendran, A., Mills, I. W., et al. (2004). Development and validation of a quality-of-life measure for men with nocturia. Urology, 63(3), 481–486.
Haapanen, N., Miilunpalo, S., Pasanen, M., Oja, P., & Vuori, I. (1997). Agreement between questionnaire data and medical records of chronic diseases in middle-aged and elderly Finnish men and women. Am J Epidemiol. ;145(8):762–769. https://doi.org/10.1093/aje/145.8.762. PMID: 9126003.
Hodgkinson, J. A., Stevens, R., Grant, S., et al. (2019). Schedules for self-monitoring blood pressure: a systematic review. American Journal Of Hypertension, 32(4), 350–364. https://doi.org/10.1093/ajh/hpy185 PMID: 30668627; PMCID: PMC6420684.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
CRediT Taxonomy: Conceptualization: Jason Lazar; Methodology: Alexandra Posner, Kamal Akbar, Gulzhan Tologonova, Thomas Monaghan, Sarah Goldman, Rasheda Browne, Jason Lazar; Formal Analysis and Investigation: Christopher Murray, Elizabeth Helzner, Rose Calixte.
Writing – Original Draft Preparation: Jason Lazar, Christopher Murray, Louis Salciccioli, Thomas Monaghan; Writing – Review and Editing: Thomas F. Monaghan, Jeffrey P. Weiss, Karel Everaert, Tine DeBacker, Elizabeth Helzner, Rose Calixte, Louis Salciccioli; Funding Acquisition: N/A; Resources: N/A; Supervision: N/A.
Corresponding author
Ethics declarations
Ethics approval (include appropriate approvals or waivers)
The present analysis employed retrospectively collected data that required institutional board approval but did not require patient consent.
Conflicts of interest/Competing interests (include appropriate disclosures)
Jason M. Lazar has no direct or indirect commercial incentive associated with publishing this article and certifies that all conflicts of interest relevant to the subject matter discussed in the manuscript are the following: Dr. Everaert has served as Promoter for the Ghent University Frederik Paulsen Chair and Medtronic OptiLUTS Chair, is a minority shareholder (without salary) in P2solutions, and has received institutional grants and honoraria from Astellas, Ferring, and Medtronic, outside the submitted work. The additional authors have nothing to disclose.
Consent to participate (include appropriate consent statements)
Not applicable.
Consent for publication (consent statement regarding publishing an individual’s data or image)
Not applicable.
Code availability (software application or custom code)
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lazar, J.M., Posner, A., Akbar, K. et al. Home Blood Pressure Monitoring And Nocturia In Adults. J Community Health 48, 238–244 (2023). https://doi.org/10.1007/s10900-022-01171-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10900-022-01171-8