Abstract
The purpose of this study was to use qualitative interviews to ascertain the perspective of pediatric primary care providers on the implementation of Integrated Behavioral Health (IBH) as provided by psychologists within an expanded HealthySteps™ model, and with a particular focus on prevention of behavioral health symptoms in the first five years. A semi-structured interview guide was used to assess medical providers’ perceptions of behavioral health integration into their primary care clinics. A conventional qualitative content analysis approach was utilized to identify patterns of meaning across qualitative interviews. Four themes were identified: (1) practice prior to IBH and initial concerns about integration, (2) psychologist’s role and perceived added value, (3) what integration looks like in practice, and (4) perceived families’ response to and experiences with IBH. Despite initial concerns about potential disruptions to clinic flow, providers indicated that adoption of IBH was seamless. The distinct roles of the psychologist were clear, and both treatment and prevention services provided by IBH were valued. Multidisciplinary collaboration and real-time response to family needs was seen as especially important and primary care providers reported that families were accepting of and highly valued IBH.
Similar content being viewed by others
Introduction
Emotional and behavioral health problems in children and adolescents have dramatically increased. In 2016, based on parent-report, 16.5% children under 18 years had a mental health disorder (Whitney & Peterson, 2019). This rate has increased during the Covid-19 pandemic, creating a significant public health problem that warrants a comprehensive and immediate response (Rider et al., 2021). Most children with emotional and behavioral health concerns are first identified in pediatric primary care (PPC). Approximately half of all pediatric primary care visits involve behavioral, emotional, or psychosocial concerns (Martini et al., 2012). As a result, pediatric primary care is an ideal setting to provide behavioral health intervention and treatment. However, primary care providers face challenges to effectively respond to these concerns (Brady et al., 2020). Lack of resources, inadequate training, time constraints, and a limited number of tested models impede development and deployment of comprehensive behavioral health approaches in pediatric primary care (Power et al., 2008). The scope of the problem requires innovative thinking and new approaches to leverage the pediatric primary care setting to address the alarming increase in emotional and behavioral health problems in children (Schor & Bergman, 2021).
PPC has several distinct features that make it an ideal setting to provide behavioral health services. PPC is almost universal, with 84% of children aged 0 to 17 receiving a well-child visit at least once in the past year (Larson et al., 2016). Pediatricians are highly trusted by families, providing opportunities to address stigma and embarrassment about mental health issues (Imfeld et al., 2021). The existing emphasis on prevention and healthy development in PPC can readily incorporate emotional and behavioral health issues. Medical homes are designed to comprehensively address all issues of health, including emotional and behavioral health. Furthermore, the recent recognition of the importance of PPC in addressing health inequities in racial and ethnic minorities and economically marginalized children has also highlighted the need for mental health support (Hodgkinson et al., 2017).
In response to these needs, several models have been developed that explicitly add behavioral health services to PPC. These include facilitated referral approaches and mental health consultation, (Sarvet et al., 2010) co-located mental health providers, (Platt et al., 2018) and fully integrated programs in which behavioral health providers are members of the pediatric team (Talmi et al., 2016). Of these models, integrated behavioral health (IBH) programs have been called out as especially promising (Yogman et al., 2018). Yet, to date such approaches have primarily focused on providing treatment for identified mental health symptoms and have given limited attention to prevention and promoting healthy emotional and behavioral health prior to symptoms developing or being identified.
The HealthySteps™ model incorporates and emphasizes IBH in PPC (Valado et al., 2019). HealthySteps™ is a practice-based approach to promotion of healthy child development and prevention of emotional and behavioral health problems in children aged 0 to 3. It involves all members of the pediatric clinic focusing on addressing health concerns related to poverty, adversity, and social risks. A key feature of the model is the integration of a behavioral health specialist in the pediatric team. The specialist works directly with families identified as being high-risk during well-child visits to provide education about development and parenting, and short-term interventions related to behavioral health and child development. At the practice level, all members of the pediatric team are aware of and sensitive to the deleterious impacts of poverty and adversity on family functioning and child development. Further, all children within the practice are screened for delayed development and behavioral health problems. A randomized clinical trial of the model established its efficacy by demonstrating increased well-child visit adherence, immunizations, receipt of anticipatory guidance, and decreased use of corporal punishment (Minkovitz et al., 2003, 2007).
The recency of broader adoption of IBH approaches, including the HealthySteps™ model, has highlighted questions about how the programs work in practice and how to best facilitate adoption. While previous qualitative studies have highlighted physician and patient perspectives about the value of integrated behavioral health services, there is discrepancy in models of care and target population (cite Miller-Matero et al. 2016; Miller-Matero et al., 2019; Fong et al., 2019). Additionally, there is a paucity of information about how practices experience the incorporation of integrated behavioral health, especially with a focus on prevention in pediatric primary care. This is important as proponents of IBH often emphasize the need for pediatric practices to be adequately prepared for adoption, including identifying barriers, modifying procedures, and anticipating how the pediatric team will best utilize behavioral health resources (Mautone et al., 2021). Pediatric practices often have concerns about how the addition of a behavioral health provider will impact clinic flow, work seamlessly with the pediatric team, be perceived by families, and balance demands to address both prevention and treatment (cite Fong et al., 2019), and this is important to stud.
The purpose of this study was to use qualitative interviews to ascertain the perspective of PPC providers on the implementation of IBH as provided by psychologists within the HealthySteps™ model, and with a particular focus on prevention of behavioral health symptoms in the first five years. Medical providers within the practices were queried about concerns prior to implementation, how the pediatric team incorporates behavioral health, their perception of family responses, and benefits and challenges of IBH with a prevention focus (see Appendix A for Interview Script). Findings have implications for understanding how (1) IBH approaches can work, (2) they impact practices and families, and (3) to prepare practices for adopting these models.
Method
Sample and Setting
We used purposive sampling to recruit providers across 3 different clinics and with different levels of experience. The sample consisted of 11 pediatric providers (10 pediatricians, 1 pediatric nurse-practitioner) recruited from three pediatric primary care clinics affiliated with an urban academic medical center. Table 1 shows the demographic characteristics of the sample. The setting consisted of three pediatric primary care centers, 2 urban and one suburban, which together are the medical home for over 36,000 active patients and see over 62,000 visits/year. The payer mix is uniform across the centers: 85% Medicaid, 3% private insurance, and 12% self-pay or uninsured. These sites train over 200 residents and medical students per year, and are staffed by over 40 attending physicians.
Integrated Behavioral Health Model
In our adaptation of the HealthySteps™ model, an HealthySteps™ specialist provided integrated behavioral health as a prevention or treatment service. IBH prevention encounters targeted all families of children 0–5 years (not just those with an elevated score on a behavioral health screen) and consisted of a 15-min visit with the family as part of the well-child visit (Ammerman et al., 2021; Herbst et al., 2020). In some cases, the visit was extended to 30 min or longer at the discretion of the psychologist based on family need. Delivered by a doctoral-level pediatric psychologist, intervention focused on four areas: (1) assessment of emotional and tried to found book review sample under 10441behavioral health of the child and caregiver, (2) education on important supports for child emotional and behavioral health, (3) modeling and guidance on nurturing and responsive parenting, and (4) addressing parental concerns about and promoting child development (Herbst et al., 2020). The encounters used trauma-informed and relationship building methods, such as motivational interviewing. The psychologists worked closely with pediatricians and the clinical team to ensure coordinated care delivery. This consisted of real-time sharing of information during well-child visits as well as discussions outside of the visit. In addition, psychologists provided short-term treatment to children of all ages in the clinics as needed, participated in crisis management as needed, and provided short-term behavioral treatment when warranted.
Procedures
Retrospective qualitative interviews were conducted with each provider and a clinical research coordinator lasting approximately 30 min. A semi-structured interview guide was used to assess medical providers’ perceptions of behavioral health integration into their primary care clinic. Queries reflected both benefits and challenges of integration. At the end of each interview, the researcher confirmed all relevant information had been included to ensure the quality and accuracy of the data. All interviews were recorded, transcribed, verified for accuracy, and entered into the qualitative analysis software, Dedoose (www.dedoose.com).
Data Analysis
The principal investigator, a psychology postdoctoral fellow, and two research assistants served as coders and analyzed the interview data using an inductive approach via conventional qualitative content analysis as outlined by Hsieh and Shannon (Hsieh & Shannon, 2005). This methodological approach mirrors traditional thematic analysis as it focuses on identification of repeated patterns of meaning across a data set and differs from summative content analysis which focuses primarily on counts and quantification of data (Braun & Clarke, 2006).
Coders had advanced training related to behavioral health as well as prior experience conducting qualitative research. Coders independently reviewed 100% of the interviews to obtain an overall framework of providers’ experiences with IBH. The coders subsequently coded the key concepts in this subset of transcripts that aligned with the interview questions (Hsieh & Shannon, 2005). Once data were independently coded from the subset, the coders discussed preliminary findings, as the use of multiple analysts to contribute to the development of codes enhances the findings’ credibility (Braun & Clarke, 2006). Codes were added or revised to reflect emerging patterns in the data. After the development of consensus among all coders around these initial codes, transcripts were independently coded (double coding). Coding led to the formation of categories and subsequently principal themes. Differences between coders were resolved through discussion of the underlying meanings of categories, revisiting the data, and reflecting on underlying elements to reach consensus. Saturation was reached when no new codes emerged. Coding checks (i.e., ongoing comparisons of independent coding, discussions to rectify differences) with alternate coders resulted in eventual consistency of greater than 90%, deeming further review was not necessary (Braun & Clarke, 2006).
To promote credibility, the authors reflected on potential sources of bias. One of the authors completed an independent audit of 20% of transcripts to verify the trustworthiness and credibility of the coding. Strategies of using two independent coders and credibility checks with participants were employed to address and minimize potential bias and positionality while optimizing accurate representation of participants’ perceptions (Braun & Clarke, 2006). One of the authors, a PPC physician, reviewed the categories following data analysis to assess alignment with personal experience with IBH in primary care (i.e., member checking).
Results
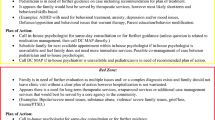
Four major themes were identified and are shown in Fig. 1. Descriptions of the themes and representative quotes from the interviews are presented below.
Practice Prior to IBH and Initial Concerns About IBH
Lack of Competency/Comfort Addressing Behavioral Health
One theme identified was around the how the primary care practices addressed behavioral health prior to implementation of IBH and the concerns they had about integration. Pediatric medical providers reported how they addressed emotional and behavioral health prior to IBH as insufficient and often unsuccessful. Some clinicians reported feeling inadequately prepared to handle more challenging behavioral problems: “I was not very comfortable with certain areas. I could talk about tantrums and sleep, and [in] other areas I needed more help.” Another clinician underscored limitations in training and preparedness that restricted their competence to address to mental health concerns: “We’re not trained necessarily in motivational interviewing, we’re not trained in interventions related to … anxiety or depression.” Others noted that, even if they felt comfortable providing emotional and behavioral health guidance, competing demands limited the amount of time they could spend with patients and families: “even if I knew the interventions to do, I might not have adequate time to do them."
Outside Referrals for Behavioral Health Concerns
Prior to integration, all providers reported a strong reliance on outside referrals for mental health support, despite recognizing this approach’s limitations. Identifying an appropriate referral site was often difficult, and the limited time providers spent with patients precluded the thorough assessment needed to appropriately match the site with the patient’s needs. “Previously, there was probably more kneejerk referrals, or we were busy. It’s a very busy clinic, so trying to get things moving, and perhaps some ineffective referrals that never got followed up on.” Frustration with the lack of follow through with many referral sites was a common issue for patients and families: “We refer to these outside agencies, and then [they] come back, and it’s like oh, we didn’t go, or we didn’t get a phone call. And you’re like oh, we’re back at square one.” Another clinician reported significant barriers to coordinate care. “When we refer to a community agency, when we refer to a school counselor, very rarely do we get any information back about how those sessions go, so most times, it’s from the family. I don’t know what type of therapy they’re getting, I don’t know if they’re seeing any improvements over a couple of months, I don’t know if the diagnoses that I’m considering are aligning with what the psychologist is seeing—he’s spending much more time with the patient.”
Initial Concerns About IBH
Prior to IBH implementation, providers noted two concerns, retrospectively, about the implementation. The first involved worry that including psychologists on the team, specifically that adding another provider would interfere with clinic flow. But following integration, the providers reported that psychologists became essential to day-to-day work: “So, now, went from, “How we gonna have them integrated in clinic and how they gonna impact flow and role?” to, “Oh my gosh, they’re not in clinic today, ‘cause they have meeting, and how we gonna do it?” “And, I can’t tell you how many times either myself, or residents, my peers would say, “How did we do that before the psychologists were in our clinic?” Second, several clinicians wondered how families would react to seeing a psychologist, and if stigma related to mental health problems might lead them to be wary and unaccepting of the services: “I think that we were nervous originally of what are people going to say when they see we have a psychologist. Should we not call them psychologists?” Another stated: “I also had some mixed feeling about parents and are they gonna be open to—and how we gonna introduce the psychologist, and what does it mean” As described below, after integration providers found that families appreciated IBH.
Psychologist’s Role and Added Value
The second theme PCPs articulated during interviews was the psychologists’ unique role and value added to both patients/families and the broader primary care, that became evident once psychologists were integrated into these settings. Regarding their specific role in patient care, the medical providers noted psychologists’ unique contributions in providing prevention, treatment, and overall clinical triage. Providers emphasized psychologists’ ability to help residents and medical team develop additional competencies in managing common behavioral presenting concerns through resident education, and hands-on learning opportunities. This theme captured how the role of the psychologist in a larger medical team is highly respected, valued, and appreciated. More specifically, within this theme the psychologists’ roles were perceived to add value in three distinct areas outlined. (Table 2)
Prevention and Treatment
PCPs recognized the distinction in services offered by the psychologists within the integrated pediatric primary care setting in both prevention and consultation/short-term behavioral health treatment. “They see patients either to provide prevention or intervention in real-time, or they can schedule appointment and follow-up, or patient can come back to see them in PPC, that is in the medical home.” Resoundingly, medical providers expressed the value of preventive behavioral health services for families, how it aligns with the pediatric medical model of care and fulfills the needs of a busy practice. “I think prevention is important. Prevention is something that, in pediatrics, we’re really focused on, and I think there’s decent evidence that behavioral health anticipatory guidance related to prevention helping improve parent/child interactions, improving school performance, and can decrease the risk of developing behavioral health disorders.”
Medical providers also emphasized the value for families being able to talk to an expert on child development and behavior at each visit to teach and reinforce positive parenting strategies that affect behavior and prevent future behavior challenges through anticipatory guidance. “I think the thing I value most is that it gives that opportunity for families to talk with someone who has expertise related to normal child development, normal parent/child interactions, because I feel like we don’t do that. We didn’t get to do that before. It was all crisis management. So, the opportunity to normalize the discussion around behavior and to—even when kids are having good behavior, to talk about it so it stays good, and start to anticipate and hopefully prevent the development of disorders or crises in the future—that’s what I value the most.” In a busy practice, medical providers stated that they need to be responsive to acute concerns and are often not able to fully address prevention topics. “I think it helps normalize that we’re gonna talk about behavior at all these visits, so I think that prevention piece is something, especially when we’re busy providers seeing 14 patients [per session], we’re running from room to room. That opportunity for prevention is not always available if there are other concerns during a visit. So, there tends to be concerns during the visit, so you wanna address those concerns appropriately, but you might miss the opportunity to provide prevention, so I think that having the opportunity to do some preventative work related to behavioral health—I think it’s important, and I think that hopefully, long-term, we’ll see payoffs related to that.” Providers noted the value in providing foundational behavioral knowledge and strategies to parents to build their confidence and capacity in managing age-typical behavioral concerns to prevent future behavioral crises. “I think that there is huge value. As the shifting from crisis management to how we can start from the get-go and get these families tools, and educate them about common behavioral problem, and how they can manage, and have more confident parents in tune with their children’s behavior can then, hopefully, eventually, eliminate the crisis or we don’t get to that point.”
PPCs viewed the ability for short-term intervention to occur within the clinic as an opportunity to help families address immediate behavioral health needs, navigate the system, and determine the appropriate level of treatment (e.g., longer psychological intervention, specialty referrals). These services also served to bridge services until the family could be seen in the community or in a specialty clinic. “But now, just the opportunity to do short-term interventions in clinic, and then bridge individuals through the psychologists to a [mental health agency] … that works best for the family, because they’re interacting more with the family, they’re having that opportunity, they’re getting the sense of is this something that a school counselor at this school would be able to handle, or is this something that really needs someone with a lot of expertise in trauma, or something else? So, I think that has been super helpful.”
PCPs commented on the frequency of behavioral health-related concerns that families want to address as part of routine well-child check visits and the role of psychologists in helping to provide evidence-based care through proper assessment and diagnosis. “Commonly there’ll be behavior—behavior concerns are the chief complaint when a child comes in. Or it’s a child well known to us for behavior issues, but we haven’t really figured out a true diagnosis, what really is going on. So, for those intervention follow ups or new visits for behavior, we really utilize behavioral health to kind of help us diagnose, really, and get—make sure we’re not just slapping an ADHD diagnosis on a kid and really being evidence-based. Same with like teenagers with depression.” Providers also saw benefit in brief consultations with psychologists for patients and families, even when it was evident that the family would require longer-term treatment beyond the scope services able to be provided in pediatric primary care through the integrated psychologist. “Even recognizing whatever the problem is, is gonna need more long-term follow-up than we’re gonna provide through the integrated psychologist, I still think it helps. It just makes for a warmer hand off and starts to give parents some tools that they can still go home with that day.”
Clinical Triage
The PCPs also identified psychologists as adding value to the clinical triaging of patients. In a busy clinic, psychologists are able to work with providers to assess and determine which consults can be handled in the moment and which patients and families are better served through follow-up visits with the psychologist. “Sometimes with consultation it’s—ʿThis is not urgent. Let’s schedule something in three days if it works for the family and sometimes the consultation happens on the spot, but we can have that informed conversation with an expert who understands the context in which our patients live, and that three days coming back actually may not work. And, even though it may not be a mental health emergency, that three days coming back will not work, and then the next time it truly will be an emergency.” Providers noted that psychologists are helpful in obtaining additional information to appropriately triage and determine the best follow-up care plan for patients in families. “They’ve been great and definitely taken the lead to some degree, and some of these kids, seeing them for … psychology only visits, helped us figure out some details on what’s going on in school or daycare settings, helped us kind of triage okay, parents can’t often be expected to make one or two referrals, but sometimes even more than one, so kinda triaging which step we’re gonna take, setting up a follow-up plan, and I think just having that backup of multiple people [in clinic] knowing about the kid, being available for follow up is really helpful.”
Psychologists are also helpful in determining the most appropriate referrals for families based on each family’s unique needs. “I think they’ve helped make sure that the referrals are appropriate because you can go to them and say I’m worried about this or about this, and I plan to refer here, and they can say well, maybe that’s not the best case. I’ve had kids I’ve wanted to get neuropsychological testing, but they’ve been able to say well, actually, you should refer them to this department rather than this department, and things like that. So, I think they kinda help streamline that and just make sure that I’m referring to the appropriate place rather than referring, then it gets denied, and the family ends up going nowhere, and it’s just this waste of time. But actually, they kinda help make sure that things are appropriate.”
Providers remarked about psychologists’ unique value in helping with higher acuity cases. “I think that has just been an incredible resource for those crisis situations, where kids come in because they’re having panic attacks, they’ve been out of school for a week. A referral where they’re gonna be seen in a month or two is just not gonna cut it, so the ability to provide interventions real-time is incredible, and I think families really appreciate it. I think providers really appreciate it because it can—it was really challenging before we had psychologists to approach some of those conditions, and I think that people were unsatisfied on both sides. Providers didn’t feel like they had adequate time, knowledge, or expertise to provide the interventions necessary, and parents maybe felt like they weren’t leaving with the skills to really address it, and so, now that we have individuals who are able to provide that real-time skill training, it’s great.” They also noted psychologist’s advanced clinical ability to help youth who express suicidal ideation and need appropriate safety planning and follow-up. "I have had several adolescents who came in with pretty high-risk cases, where there’s suicidal ideation, or significant depression or anxiety, and when I had discussed the case with a psychologist, we were able to either prevent emergency room referral or handle it in real time.”
Teaching and Training
PCPs also noted the value of psychologists’ role in teaching medical providers and residents. “I think they’ve really broadened our knowledge about kinda some—both some techniques and background, I think, about whether it’s trauma, looking for patterns, just ways that we interact with families, improving our motivational interviewing and other skills. I mean, just having their knowledge base and hearing—available to us, then we can apply those to other patients, so there’s been a really broad variety of benefits to my practice.” Providers stated that having psychologists sit in the shared workstation with other staff and providers allows for natural learning opportunities, as they provide unique perspectives on patients and families. “When you have psychologists sitting with you in the room, who are listening in and offering guidance, it just makes you recognize, oh, I hadn't really thought about this before. So I think you try to view things, and you start to view things in a different light because you have these wonderful psychologists sitting in the room with you, to kind of engage with and collaborate, and I also think—we’ve also learned a ton that's made us a lot more comfortable dealing with these issues.” Additionally, psychologists engage in medical resident teaching opportunities and use in the moment interactions with residents to help them cultivate their skillsets further. “That was one of our biggest wins, I feel like, with psychology, it's been the resident education. They're a very proactive group, the residents are in general. They really want to learn, and when they come, to PPC, they're like sponges. They want to soak up all the stuff, so they are always going to psychologists, and the psychologists do a great job because it's changed a little bit to ‘I want to go and see every kid too, ‘what do you think we should tell them?’ ‘What are things that we could do?’ So, I think it's really empowered the residents to try and do a little bit more intervention on their own, as opposed to always just defaulting to the psychologists because, you know, most places don't have a psychologist sitting 3 feet away. I think it's been a real win from resident education perspective as well.” Providers also highlighted that the entire team had learned a lot from the psychologists. “They are fantastic educators. So, we have all learned a ton from them.”
What Integration Looks Like in Practice
Psychologists are Seamlessly Integrated into Clinic Flow
The third larger theme identified in the interviews was around what the integration of behavioral health into the practices actually looked like. PCPs noted that psychologists were seamlessly integrated into clinic flow and are available in real-time. “I think its improved efficiency, in the sense that it—it kind of—our roles well, and we overlap in some ways, but it’s improved the efficiency, it’s improved the consistency of advice and care that the families are getting. And I think it’s allowed a much more streamlined approach to actual problems that come up for families to have an expert available.” Despite initial concerns that an additional team member might impact flow of clinic, providers remarked that psychologists were mindful of flow and non-disruptive to it. “I would say the psychologists are very thoughtful about flow. I feel like they have not really impacted clinic flow, from my standpoint. It’s very impressive. They are like ninjas getting in there and getting out.”
Collaboration
They noted that psychologists are “very approachable” and responsive to in the moment consultations, which further promotes behavioral health access and medical provider skill development. “And they’re right in the workroom, so they’re easy to—accessible, and to talk to, so that kind of helps with treatment as well, that it's this multidisciplinary approach all in one office, I think is really great for families too.” Providers noted that a natural collaborative environment had developed over time. “The other thing that I think has been really fantastic is just the sense of collaboration. Like it is not like this. I'm here. The psychologists are over there. My people go and talk with them. Maybe they’ll come and talk with us. There's just this kind of very natural kind of evolution that has taken place within the clinic. We all sit together, we all work together, we all chat about—not only just about patients. We chat about whatever. And so you feel like you’ve kind of created like a whole new group of friends.”
Working Through Challenges and Barriers to IBH
With any new change, a system can be expected to encounter challenges and barriers. For instance, providers described some initial challenges between navigating social workers’ and psychologists’ roles as they were “trying to figure out whose domain is whose domain.” However, providers also noted that role confusion has been resolved through collaborative efforts and discussion. “I think there’s been a lot of discussion, a lot of collaborative teamwork between psychology and our social workers to kind of come to it. I feel like I have a pretty good understanding of who does what, and a lot of stuff they do together and work together, something that's ultimately turned into a positive for us.” Another challenge noted by medical providers was limited space in the workroom. “Really, probably just physical space. Sometimes we don’t have enough seats.” A couple of medical providers wondered how the addition of psychologists might impact residents’ critical thinking skills over time as they became more reliant on psychologists. I worry a little bit, doing both together incapacitates the provider, more of that turfing that I was talking about of, like, “This eight-year-old, they’re [complicated]. I don’t know what to do." We have to deal with that here, and I like that. I don’t want them taking away critical thinking skills from pediatricians. I feel like “You should be enhancing skills, not taking away.” I don’t know that that's happening, but I just—That’s one of the things that I think gets really blurry.” When asked about ways that integration efforts could be improved, medical providers responded resoundingly requesting more psychologists. “I dream of the days where we will have psychologists 8:00 [am] to 8:00 [pm] and on Saturdays.” Providers differed in how they would allocate additional psychologist efforts some requesting enough psychologists to “see every well-child checkup visit from birth and during the most critical years before entering kindergarten,” while others noted they would “prioritize teenagers,” and further requested “robust availability for problem-based visits, trauma care.” Other providers noted that following and providing care to families at greater risk for emotional and behavioral difficulties is beneficial. “Sometimes the intervention visits at times may be more important than prioritizing certain well-child prevention visits. I think it would be good to identify high-risk families, specifically, and follow them definitely like throughout, but then that may be a way to utilize the resources a little better.”
Families’ Response to IBH and Experiences with IBH
Families are Open to Seeing a Psychologist
The fourth large theme identified in this study reflected that PCPs experience that families were overwhelmingly open to the idea of seeing a psychologist. One stated “honestly, none of them [families] ever say no.” It was noted that psychologists are seen as part of the team, and the close connection between emotional and behavioral health and other aspects of pediatric health care reduced stigma associated with mental health topics: “They're already here. They don’t honestly see it as a mental health provider; I think they just think they're a different one of us. So, I think that, for the families, is huge. It's the ability for our at-risk, socially limited families to get to a brand new place to start a brand new intake process. It feels overwhelming for me, and I'm not living their lives. So, I think that's by far the biggest benefit."
Families Appreciate Access to IBH in Primary Care
Given frustrations associated with outside referrals and barriers to accessing mental health support in the community, the ability to provide preventive services right away in the pediatric clinic was seen as an important benefit of IBH, especially for racial and ethnic minorities and families that face considerable barriers to accessing behavioral health services. One provider recounted an example of being able to quickly respond to a family’s behavioral health needs: “’We’re very fortunate to have psychologists here, and I know that’s something that we were talking about and let me check to see if one of them is available if you have time to stay. How would that work?’ And, again, usually it’s, ‘Oh my gosh, we can see someone today? It’s fabulous! We’ve been on a waiting list for a long time.’ So, I think it’s really changed.”
Families Find Value in Meeting with Psychologist
The integration of preventive behavioral health services also brought structure and organization to concerns that would otherwise have been inadequately addressed. Several providers described the value of having a plan for supporting families going forward. One provider stated that “if you follow up with that patient in the future, you know what’s been addressed, and you can kinda continue to build on those things. So, I think that’s been the most impactful, is being able to have a clear plan with families in real-time during the visit.” Another provider, describing a child with emerging externalizing behavior problems, stated “what I get from the families is that they know what the plan is, they know what to do, and they like it, which is, I think, good. Because before they’re like, well we’re just waiting until they turn 5, so you can start medicine, and now there's a plan of what they’re doing and they're working on it.”
Also important was the teaching of specific skills in the IBH encounter: “So our psychologist was in the room with him for like 20 min, and the family was so impressed and engaged with all these different strategies to kind of alleviate the tic, and even in the 20 min she was in the room, came up with some strategies that were already working while she was in there. And that’s the stuff. This kid has been missing school, had been out of school for I don’t know how long because of this tic, and 20 min in a room with one of our psychologists, and I don’t want to say it's all resolved, but I mean definitely on a road to kind of making significant improvements.” Teaching-specific skills and providing strategies to use at home was identified as an additional benefit: “I’m seeing parents leaving with tools that they can use to either handle sleep problem, or feeding, or tantrum, or whatsoever. They’re applying it and coming back with feedback that it did work or it didn’t.”
Discussion
This qualitative study queried medical providers in pediatric primary care about their experiences with integrated behavioral health (IBH) provided by psychologists. IBH has expanded nationally in the past decade, fueled by increases in mental health disorders in children. Concerns about access to mental health care, particularly in racial and ethnic minorities and children living in poverty, have further spotlighted pediatric primary care as a promising setting to reach, engage, educate, and treat emotional and behavioral health issues in children (Mautone et al., 2021). Yet the accelerated adoption of IBH models has occurred in the absence of a full understanding of how to best design and implement these programs. Our study sought to address this gap by collecting and synthesizing the perspectives of pediatric primary care medical providers about their view on the challenges and benefits of IBH in their clinics. Results indicated that, while some providers had concerns about the operational feasibility of IBH, the experience with the approach was universally positive and the anticipated barriers did not occur.
The success of integrating behavioral health into the pediatric practice was quick and relatively seamless. Providers reported that early fears of disruptions to clinic flow, feasibility of smooth integration, and acceptability were unfounded. This is at least partly attributable to training and preparation in advance. HealthySteps™ training prepared the practices to incorporate behavioral health clinicians, and discussions about logistics and needed procedural accommodations were held prior to introduction of IBH. Guidance on adopting IBH in pediatric practices emphasizes preparation and readiness (McLeigh et al., 2022). Our qualitative findings provide support for the importance of this step in adopting an IBH model.
Pediatric providers identified a number of benefits of IBH. They noted that offering the service universally highlighted the valuing of emotional and behavioral health. Seeing a mental health provider from the very first well-child visit normalized the topic of behavioral concerns, decreasing stigma associated with seeing a mental health professional. The importance of integration with the clinical team was a predominate theme of the qualitative interviews. Working together closely and in real-time permitted rapid attending to family needs, optimized efficiency, and led to better overall care. Prior to integrations, pediatric providers reported a heavy reliance on outside referrals for mental health concerns, a strategy that was often unsuccessful. Availability of the psychologist in the clinic, on the other hand, led to quick responding to needs and regular communication about progress.
An additional benefit of IBH was the opportunity for training of pediatricians, residents, and other members of the medical team in mental health issues. Given the recent emphasis on enhancing the competence of pediatric providers in addressing mental health problems, this feature of IBH can contribute to practice transformation (Schor & Bergman, 2021). Psychologists provided training both informally and formally. They modelled strategies for building parenting skills and responding to emotional and behavioral health concerns. Team huddles and meetings provided opportunities for discussion of approaches and strategies. More structured didactic training was provided on important issues in emotional and behavioral health.
This study had several strengths. We sought to identify specific benefits and challenges with IBH. Queries addressed multiple aspects of IBH, including operational logistics, impact on families and providers, and training. The study was conducted in an academic medical center. Given that over 5 million children receive pediatric care in such clinics, findings are generalizable to similar settings (Krugman et al., 2007). There are also limitations to the study. The number of participants was small and comprised mostly of pediatricians. Other medical providers and families were not included. Quantitative elements of behavioral health integration were not collected.
Implications for Behavior Health
Our findings have several implications for clinical practice and future research. Acceptance of integrated behavioral health for clinical providers and families is broad. Practice preparation is an essential component of adopting integrated behavioral health, but there is clear guidance on procedures and strategies needed to accomplish this (Riley et al., 2022). Balancing the competing needs for prevention and acute treatment is a significant challenge. Careful oversight and continual monitoring are required to maintain focus and achieve targeted objectives. There is a strong need for full coverage of patient populations, made difficult by inconsistent funding for prevention across states and availability of qualified mental health providers (Merikangas et al., 2011). Finally, there is a need for a more definitive evidence base documenting the short and long-term impacts of integrated behavioral health and prevention efforts in pediatric primary care (Brown et al., 2018).
Data Availability
Consistent with the open science movement, we will share with other investigators (1) individual participant data after deidentification and (2) study management documents (protocol, statistical analysis plan, consent form, analytic code, data dictionary). These will be made available three months after publication of the primary article and ending five years after publication. Those requesting data will be required to submit a proposal to the PI. This will be reviewed by the investigative team for methodological soundness and scientific merit before data are shared. This plan is consistent with guidelines developed by the International Committee of Medical Journal Editors (Taichman et al., 2017).
Code Availability
Not applicable.
References
Ammerman, R., Herbst, R., & Stark, L. (2021). Integrated Behavioral Health Prevention in Pediatric Primary Care. Cincinnati Children’s Hospital Medical Center, Cincinnati, Ohio, 1–16.
Brady, K. J., Durham, M. P., Francoeur, A., Henneberg, C., Adhia, A., Morley, D., Tamene, M., Singerman, A., Morris, A., & Fortuna, L. R. (2020). Barriers and facilitators to integrating behavioral health services and pediatric primary care. Clinical Practice in Pediatric Psychology.
Braun, V., & Clarke, V. (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3(2), 77–101.
Brown, C. M., Raglin Bignall, W. J., & Ammerman, R. T. (2018). Preventive behavioral health programs in primary care: A systematic review. Pediatrics. https://doi.org/10.1542/peds.2017-0611
Herbst, R. B., McClure, J. M., Ammerman, R. T., Stark, L. J., Kahn, R. S., Mansour, M. E., & Burkhardt, M. C. (2020). Four innovations: A robust integrated behavioral health program in pediatric primary care. Families, Systems, & Health, 38(4), 450.
Hodgkinson, S., Godoy, L., Beers, L. S., & Lewin, A. (2017). Improving mental health access for low-income children and families in the primary care setting. Pediatrics. https://doi.org/10.1542/peds.2015-1175
Hsieh, H.-F., & Shannon, S. E. (2005). Three approaches to qualitative content analysis. Qualitative Health Research, 15(9), 1277–1288.
Imfeld, S. M., Darang, D. M., Neudecker, M., & McVoy, M. K. (2021). Primary care pediatrician perceptions towards mental health within the primary care setting. Pediatric Research, 90(5), 950–956.
Krugman, S. D., Racine, A., Dabrow, S., Sanguino, S., Meyer, W., Seid, M., & Serwint, J. R. (2007). Measuring primary care of children in pediatric resident continuity practices: A Continuity Research Network study. Pediatrics, 120(2), e262–e271.
Larson, K., Cull, W. L., Racine, A. D., & Olson, L. M. (2016). Trends in access to health care services for US children: 2000–2014. Pediatrics. https://doi.org/10.1542/peds.2016-2176
Martini, R., Hilt, R., Marx, L., Chenven, M., Naylor, M., Sarvet, B., & Ptakowski, K. K. (2012). Best Principles for Integration of Child Psychiatry into the Pediatric Health Home. 1–13
Mautone, J. A., Wolk, C. B., Cidav, Z., Davis, M. F., & Young, J. F. (2021). Strategic implementation planning for integrated behavioral health services in pediatric primary care. Implementation Research and Practice, 2, 2633489520987558.
McLeigh, J. D., Malthaner, L., Winebrenner, C., & Stone, K. E. (2022). Paediatric integrated care in the primary care setting: A scoping review of populations served, models used and outcomes measured. Child: Care, Health and Development. https://doi.org/10.1111/cch.13000
Merikangas, K. R., He, J.-P., Burstein, M., Swendsen, J., Avenevoli, S., Case, B., Georgiades, K., Heaton, L., Swanson, S., & Olfson, M. (2011). Service utilization for lifetime mental disorders in US adolescents: Results of the National Comorbidity Survey-Adolescent Supplement (NCS-A). Journal of the American Academy of Child & Adolescent Psychiatry, 50(1), 32–45.
Minkovitz, C. S., Hughart, N., Strobino, D., Scharfstein, D., Grason, H., Hou, W., Miller, T., Bishai, D., Augustyn, M., & McLearn, K. T. (2003). A practice-based intervention to enhance quality of care in the first 3 years of life: The healthy steps for young children program. JAMA, 290(23), 3081–3091.
Minkovitz, C. S., Strobino, D., Mistry, K. B., Scharfstein, D. O., Grason, H., Hou, W., Ialongo, N., & Guyer, B. (2007). Healthy steps for young children: sustained results at 5.5 years. Pediatrics, 120(3), e658–e668.
Platt, R. E., Spencer, A. E., Burkey, M. D., Vidal, C., Polk, S., Bettencourt, A. F., Jain, S., Stratton, J., & Wissow, L. S. (2018). What’s known about implementing co-located paediatric integrated care: A scoping review. International Review of Psychiatry, 30(6), 242–271.
Power, T. J., Mautone, J. A., Manz, P. H., Frye, L., & Blum, N. J. (2008). Managing attention-deficit/hyperactivity disorder in primary care: A systematic analysis of roles and challenges. Pediatrics, 121(1), e65–e72.
Rider, E. A., Ansari, E., Varrin, P. H., & Sparrow, J. (2021). Mental health and wellbeing of children and adolescents during the covid-19 pandemic. BMJ. https://doi.org/10.1136/bmj.n1730
Riley, A. R., Walker, B. L., Ramanujam, K., Gaultney, W. M., & Cohen, D. J. (2022). A mixed-method investigation of parent perspectives on early childhood behavioral services in primary care. The Journal of Behavioral Health Services & Research, 49(2), 134–148.
Sarvet, B., Gold, J., Bostic, J. Q., Masek, B. J., Prince, J. B., Jeffers-Terry, M., Moore, C. F., Molbert, B., & Straus, J. H. (2010). Improving access to mental health care for children: The Massachusetts Child Psychiatry Access Project. Pediatrics, 126(6), 1191–1200.
Schor, E. L., & Bergman, D. (2021). Pediatric preventive care: Population health and individualized care. Pediatrics. https://doi.org/10.1542/peds.2020-049877
Talmi, A., Muther, E. F., Margolis, K., Buchholz, M., Asherin, R., & Bunik, M. (2016). The scope of behavioral health integration in a pediatric primary care setting. Journal of Pediatric Psychology, 41(10), 1120–1132.
Valado, T., Tracey, J., Goldfinger, J., & Briggs, R. (2019). HealthySteps. The Future of Children, 29(1), 99–122.
Whitney, D. G., & Peterson, M. D. (2019). US national and state-level prevalence of mental health disorders and disparities of mental health care use in children. JAMA Pediatrics, 173(4), 389–391.
Yogman, M. W., Betjemann, S., Sagaser, A., & Brecher, L. (2018). Integrated behavioral health care in pediatric primary care: A quality improvement project. Clinical Pediatrics, 57(4), 461–470.
Acknowledgements
The authors thank Laura Raney for assistance to the project.
Funding
The Behavioral Health Integration in Pediatric Primary Care Project was funded by the Ohio Department of Medicaid (Grant No. G-2021-05-0069) and administered by the Ohio Colleges of Medicine Government Resource Center. The views expressed in this publication are solely those of the authors and do not represent the views of the state of Ohio or federal Medicaid programs.
Author information
Authors and Affiliations
Contributions
RTA conceptualized and designed the study, designed the data collection instruments, coordinated and supervised data collection, drafted the initial manuscript, and reviewed and revised the manuscript. TMR conducted qualitative analysis, drafted the initial manuscript, reviewed, and revised the manuscript. RBH and ZMS, and AB, AM, and EB, conducted qualitative analysis, reviewed, and revised the manuscript. CZ designed the data collection instruments and coordinated data management, reviewed, and revised the manuscript. LJS and JMM helped with conceptualization of the study and reviewed and revised the manuscript. All authors reviewed and revised the manuscript and approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
Authors Tiffany M. Rybak, Rachel B. Herbst, Lori J. Stark, Zeina M. Samaan, Cynthia Zion, Alyssa Bryant, Jessica M. McClure, Aileen Maki, Elizabeth Bishop, Aimee Mack, T. Ammerman have no conflicts of interest relevant to this article to disclose.
Ethics Approval
This paper has Institution Review Board approval.
Consent to Participate
Not applicable—waiver of consent.
Consent for Publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
IBH Pediatric Provider Qualitative Interview
Thank you for volunteering to participate in our IBH Qualitative Interview for Pediatric Providers. Your honest feedback is important to us as we improve our systems of care in primary care. We want to understand your experiences so we can get better. Our questions aren’t about any individual practitioner and your answers will in no way be used to evaluate any individual practitioner’s performance. Your answers will be de-identified and reported in aggregate prior to being reviewed by the research team.
Introduction/ Warm-up
Tell me about your background working in primary care.
Tell me a bit about your experience here in (PPC/HPC/FPC).
Awareness & Cultural Impact of IBH services
How would you describe the service that the psychologists provide in the practice?
What value does the psychologist bring to the clinical team?
Has the practice changed since the integration of psychologists into the practice? How would you describe that change?
Experiences interacting with IBH
Tell me about how you collaborate with the psychologists.
Tell me about how having the psychologist has impacted patient care.
Tell me about how having the psychologist has impacted your day-to-day clinical practice.
How has IBH impacted your approach to addressing mental health concerns in your patients?
Tell me about any change in your knowledge or confidence in addressing patients’ mental health concerns?
How has IBH impacted your comfort managing those concerns?
Thoughts about intervention versus prevention
Psychologists’ services are categorized into prevention or intervention visits for reporting purposes. Prevention visits focus on anticipatory guidance and typically occur alongside well child checks whereas when psychologists are addressing a family concern we label these intervention visits. We would like to get your thoughts and opinions about each of these types of services.
Since the psychologist has been in clinic, have you changed how you address typical behavioral concerns with parents (sleep, feeding, fussiness, etc.)?
Have you learned new tips or tricks to better [address or talk about] these concerns with your patients?
(re: content vs message delivery)
Since the psychologist has been in clinic, have you changed how you address emerging mental health or developmental challenges with parents?
Since the psychologist has been in clinic, have you changed how you address high-risk cases or immediate crises?
Whole-practice integration
We know there can be challenges to incorporating new services into the clinic workflow. Tell me about any barriers to clinical care you have noticed since the integration of psychology into the practice?
Tell me about how the psychologists have facilitated good clinical practice since their integration into the clinic.
Since the integration of psychology have you noticed any changes in the way administrative staff operate or interact with patients? Nurses? Medical assistants? Residents? Tell me about those changes.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Rybak, T.M., Herbst, R.B., Stark, L.J. et al. Provider Perspectives on an Integrated Behavioral Health Prevention Approach in Pediatric Primary Care. J Clin Psychol Med Settings 30, 741–752 (2023). https://doi.org/10.1007/s10880-023-09947-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10880-023-09947-3