Abstract
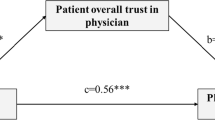
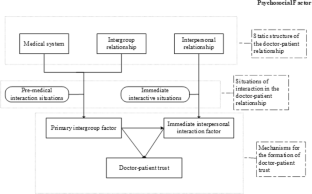
Based on an integrated model of doctor–patient psychological mechanisms, the formation mechanism of doctor-–patient trust was systematically demonstrated from the healthcare professional (HCP)’s perspective integrating intergroup relations (expectations), interpersonal relations (communication), and psychosocial (stereotypes). The results of a survey of 3000 doctors and nurses from 14 provinces in eastern, central, and western China support the rationality of an integrated model of doctor–patient psychological mechanisms. The establishment of doctor–patient trust is influenced by the direct role of primary intergroup factors, the indirect role of immediate interpersonal interactions, and the moderating role of social psychology. Specifically, (1) doctor–patient trust is directly predicted by HCP’s expectation and indirectly influenced by communication; (2) stereotypes regulate the relationship between HCP’s expectation, communication, and doctor–patient trust: the activation of positive stereotypes enhances the positive relationship among the three; Negative stereotypes only positively contribute to mediated pathway-communication behaviors and have a weaker facilitation effect compared to positive stereotypes.




Similar content being viewed by others
Data Availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Agliata, A. K., & Renk, K. (2009). College students’ affective distress: The role of expectation discrepancies and communication. Journal of Child and Family Studies, 18(4), 396.
Atkinson, J. W. (1957). Motivational determinants of risk-taking behavior. Psychological Review, 64(6p1), 359.
Bandura, A. (1986). Social foundations of thought and action. Englewood Cliffs, NJ, 1986(23–28)
Barber, B. (1983). The logic and limits of trust. New Brunswick, NJ: Rutgers University Press.
Baviskar, K. (2015). Doctor-patient relation a study of communication. Asian Journal of Research in Social Sciences and Humanities, 5(9), 1–8.
Birkhäuer, J., Gaab, J., & Calnan, M. (2017). Is having a trusting doctor-patient relationship better for patients’ health? European Journal for Person Centered Healthcare, 5(1), 145–147.
Bostan, S., Acuner, T., & Yilmaz, G. (2007). Patient (customer) expectations in hospitals. Health Policy, 82(1), 62–70.
Cegala, D. J., Coleman, M. T., & Turner, J. W. (1998). The development and partial assessment of the medical communication competence scale. Health Communication, 10(3), 261–288.
Chai, M. Q., & Wang., J., (2016). An exploration of formation mechanism of doctor-patient trust crisis: From the perspective of intergroup relationship. Journal of Nanjing Normal University (Social Science Edition), 02
Chang, P.-C., Wu, T., & Du, J. (2020). Psychological contract violation and patient’s antisocial behaviour. International Journal of Conflict Management, 31(4), 647–664. https://doi.org/10.1108/ijcma-07-2019-0119
Chrisler, J. C., Barney, A., & Palatino, B. (2016). Ageism can be hazardous to women’s health: Ageism, sexism, and stereotypes of older women in the healthcare system. Journal of Social Issues, 72(1), 86–104.
Cook, K. S., Kramer, R. M., Thom, D. H., Stepanikova, I., Mollborn, S. B., & Cooper, R. M. (2004). Trust and distrust in patient-physician relationships: Perceived determinants of high-and low-trust relationships in managed-care settings. Russell Sage Foundation.
Crisp, R. J., & Turner, R. N. (2009). Can imagined interactions produce positive perceptions?: Reducing prejudice through simulated social contact. American Psychologist, 64(4), 231–240.
Cuddy, A. J., Fiske, S. T., & Glick, P. (2007). The BIAS map: Behaviors from intergroup affect and stereotypes. Journal of Personality and Social Psychology, 92(4), 631–648.
Dhingra, C., Anand, R., & Prasad, S. (2014). Reflection over doctor patient relationship: A promise of trust. Journal of Oral Health & Community Dentistry, 8(2)
Dong, X. (2020). New interpretation of trust from the holistic perspective. Journal of China University of Mining & Technology(Social Sciences), (1009–105X), 1–10.
Dong, Z., & Chen, C. (2016). A preliminary study of validity and reliability of the Chinese version of the Physician Trust in Patient Scale. Chinese Mental Health Journal, 30(7), 481–485.
Douglass, T., & Calnan, M. (2016). Trust matters for doctors? Towards an agenda for research. Social Theory & Health, 14(4), 393–413.
Du, L., Xu, J., Chen, X., Zhu, X., Zhang, Y., Wu, R., Ji, H., & Zhou, L. (2020). Rebuild doctor–patient trust in medical service delivery in China. Scientific Reports, 10(1), 1–11. https://doi.org/10.1038/s41598-020-78921-y
Gabay, G. (2019). Patient self-worth and communication barriers to trust of Israeli patients in acute-care physicians at public general hospitals. Qualitative Health Research, 29(13), 1954–1966.
Glasman, L. R., & Albarracín, D. (2006). Forming attitudes that predict future behavior: A meta-analysis of the attitude-behavior relation. Psychological Bulletin, 132(5), 778.
Greene, J., & Ramos, C. (2021). A mixed methods examination of health care provider behaviors that build patients’ trust. Patient Education and Counseling, 104(5), 1222–1228.
Grob, R., Darien, G., & Meyers, D. (2019). Why physicians should trust in patients. JAMA, 321(14), 1347.
Guo, A., & Wang, P. (2020). The current state of doctors’ communication skills in Mainland China from the perspective of doctors’ self-evaluation and patients’ evaluation: A cross-sectional study. Patient Education and Counseling, 104, 1–7.
Hao, J., Yang, J., Peng, Y., & Ma, X. (2016). Factor analysis of patients’ trust of township health centers in suburbs, Beijing. Medicine and Society, 29(4), 17–19.
Hauer, K. E., Fernandez, A., Teherani, A., Boscardin, C. K., & Saba, G. W. (2011). Assessment of medical students’ shared decision-making in standardized patient encounters. Journal of General Internal Medicine, 26(4), 367–372.
Hayes, A. F. (2012). PROCESS: A versatile computational tool for observed variable mediation, moderation, and conditional process modeling. University of Kansas.
Higgins, E. T., Idson, L. C., Freitas, A. L., Spiegel, S., & Molden, D. C. (2003). Transfer of value from fit. Journal of Personality and Social Psychology, 84(6), 1140.
Hillen, M., De Haes, H., Stalpers, L., Klinkenbijl, J., Eddes, E., Butow, P., van der Vloodt, J., van Laarhoven, H. W., & Smets, E. (2014). How can communication by oncologists enhance patients’ trust? An experimental study. Annals of Oncology, 25(4), 896–901.
Koirala, N. (2019). Trust and communication in a doctor patient relationship. Birat Journal of Health Sciences, 4(3), 770–770.
Kuzla, A. (2017). A review of acceptant responses to stereotype threat: Performance expectations and self-handicapping strategies. DTCF Dergisi, 57(2), 1223–1248.
Li, Y., & Wang, P. (2018). The social psychological mechanism of the construction of doctor-patient trust. Chinese Social Psychological Review, 14, 4–15.
Liu, J., Yu, C., Li, C., & Han, J. (2020). Cooperation or conflict in doctor-patient relationship? An analysis from the perspective of evolutionary game. IEEE Access, 8, 42898–42908.
Luhmann, N. (2018). Trust and power. Wiley.
Makoul, G. (2001). The SEGUE framework for teaching and assessing communication skills. Patient Education and Counseling, 45(1), 23–34.
Marx, D. M., & Stapel, D. A. (2006). Understanding stereotype lift: On the role of the social self. Social Cognition, 24(6), 776–792.
Nie, J. B., Cheng, Y., Zou, X., Gong, N., Tucker, J. D., Wong, B., & Kleinman, A. (2018). The vicious circle of patient–physician mistrust in China: Health professionals’ perspectives, institutional conflict of interest, and building trust through medical professionalism. Developing World Bioethics, 18(1), 26–36.
Oettingen, G., & Mayer, D. (2002). The motivating function of thinking about the future: Expectations versus fantasies. Journal of Personality and Social Psychology, 83(5), 1198.
Perna, G., Varriale, L., & Ferrara, M. (2019). The role of communication in stereotypes, prejudices and professional identity: The case of nurses. Organizing for digital innovation (pp. 79–95). Springer International Publishing.
Petrocchi, S., Iannello, P., Lecciso, F., Levante, A., Antonietti, A., & Schulz, P. (2019a). Interpersonal trust in doctor-patient relation: Evidence from dyadic analysis and association with quality of dyadic communication. Social Science & Medicine, 235, 112391.
Petrocchi, S., Iannello, P., Lecciso, F., Levante, A., Antonietti, A., & Schulz, P. J. (2019b). Interpersonal trust in doctor-patient relation: Evidence from dyadic analysis and association with quality of dyadic communication. Social Science & Medicine. https://doi.org/10.1016/j.socscimed.2019.112391
Prizer, L. P., Gay, J. L., Perkins, M. M., Wilson, M. G., Emerson, K. G., Glass, A. P., & Miyasaki, J. M. (2017). Using social exchange theory to understand non-terminal palliative care referral practices for Parkinson’s disease patients. Palliative Medicine, 31(9), 861–867.
Qu, X. P., & Ye, X. C. (2014). Development and evaluation research of measurement tools for stereotypes of doctor role perception. Chinese Hospital Management, 34(2), 48–50.
Riva, S., & Pravettoni, G. (2014). How to define trust in medical consultation? A new perspective with the game theory approach. Global Journal for Research Analysis, 3(8), 76–79.
Rosenthal, R. (2003). Covert communication in laboratories, classrooms, and the truly real world. Current Directions in Psychological Science, 12(5), 151–154.
Ruan, X., & Xiao, X. (2017). Correlation analysis on trusted patient assessment and occupational well-being of pediatricians in Wuhan City. Occup and Health, 33(12), 1661–1664.
Ruscher, J. B. (1998). Prejudice and stereotyping in everyday communication. Advances in Experimental Social Psychology, 30, 241–307.
Scheid, T. L., & Smith, G. H. (2017). Is physician-patient concordance associated with greater trust for women of low socioeconomic status? Women & Health, 57(6), 631–649.
Schneider, D. J. (2005). The psychology of stereotyping. Guilford Press.
Shah, R., & Ogden, J. (2006). ‘What’s in a face?’The role of doctor ethnicity, age and gender in the formation of patients’ judgements: An experimental study. Patient Education and Counseling, 60(2), 136–141.
Sherlock, R. (1986). Reasonable men and sick human beings. The American Journal of Medicine, 80(1), 2–4.
Shih, M., Ambady, N., Richeson, J. A., Fujita, K., & Gray, H. M. (2002). Stereotype performance boosts: The impact of self-relevance and the manner of stereotype activation. Journal of Personality and Social Psychology, 83(3), 638.
Skirbekk, H., Middelthon, A.-L., Hjortdahl, P., & Finset, A. (2011). Mandates of trust in the doctor–patient relationship. Qualitative Health Research, 21(9), 1182–1190.
Street, R. L., Jr. (2002). Gender differences in health care provider–patient communication: Are they due to style, stereotypes, or accommodation? Patient Education and Counseling, 48(3), 201–206.
Sun, L., & Wang, P. (2019a). Theoretical system of the harmonious doctor-patient relationship evaluation. Journal of Shanghai Normal University(Philosophy & Social Sciences Edition), 48(05), 88–98.
Sun, L., & Wang, P. (2019b). Theory construction on the psychological mechanism of the harmonious doctor-patient relationship and its promoting technology. Advances in Psychological Science, 27(6), 951–964.
Thom, D. H., & Campbell, B. (1997). foTlG INALRESEARCH patient-physician trust: An exploratory study. The Journal of Family Practice, 44(2), 169.
Thom, D. H., Wong, S. T., Guzman, D., Wu, A., Penko, J., Miaskowski, C., & Kushel, M. (2011). Physician trust in the patient: Development and validation of a new measure. The Annals of Family Medicine, 9(2), 148–154.
Thorne, S. E., & Robinson, C. A. (1988). Reciprocal trust in health care relationships. Journal of Advanced Nursing, 13(6), 782–789.
Tyler, R., & Pugh, L. C. (2009). Application of the theory of unpleasant symptoms in bariatric surgery. Bariatric Nursing and Surgical Patient Care, 4(4), 271–276.
Wang, P. (1999). A review of social cognitive research on stereotypes. Journal of Psychological Science, 22(4), 342–345.
Wang, X. J., & Wang, C. (2016). Doctor-patient trust in contemporary China: Characteristics, current situation and research prospects. Journal of Nanjing Normal University (Social Science Edition), 2, 102–109.
Wang, P., Yin, Z., Luo, X., Ye, X., & Bai, Y. (2018). The impact of doctor-patient communication frequency on the stereotype of the doctor. Studies of Psychology and Behavior, 16(1), 119.
Ward, P. (2018). Trust and communication in a doctor-patient relationship: A literature review. Arch Med, 3(3), 36.
Xu, L. L., Sun, L. N., Li, J. Q., Zhao, H. H., & He, W. (2021). Metastereotypes impairing doctor–patient relations: The roles of intergroup anxiety and patient trust. PsyCh Journal, 10(2), 275–282.
Yao, Q., Ma, H. W., & Yue, G. A. (2010). Success expectations and performance: Regulatory focus as a moderator. Acta Psychologica Sinica, 42(06), 704.
Yoshihisa, K., & Victoria, W.-L.Y. (2010). Serial reproduction: An experimental simulation of cultural dynamics. Acta Psychologica Sinica, 42(01), 56–71.
Zhang, B., Yuan, F., & Xu, L. (2014). Reducing the effects of stereotype threat: intervention strategies and future directions. Journal of Psychological Science, 37(1), 197–204.
Zhang, N., & Zhao, J. (2014). Research on credibility crisis in doctor-patient relationship based on expectation disconfirmation theory. Chinese Medical Ethics, 27(3), 391–393.
Acknowledgements
We thank the staff of our partner hospitals for their help in collecting data.
Funding
This research was supported by Major bidding projects for National Social Sciences Fund of China (17ZDA327).
Author information
Authors and Affiliations
Contributions
YW and QW contributed equally to this article. YW and QW: design of the work; analysis, interpretation of data for the work, drafting the work and revising it critically for important intellectual content. YW: proofreading manuscript. PW: validation, investigation, resources, writing—review and editing, supervision, project administration, funding acquisition, and final approval of the version to be published.
Corresponding author
Ethics declarations
Conflict of interest
Yao Wang, Qing Wu, Yanjiao Wang, and Pei Wang declare that they have no conflict of interest.
Ethical Approval
This study was approved by the local ethics committee of Shanghai Normal University and was conducted in accordance with the Declaration of Helsinki (2013).
Consent to Participate
All participants were informed before the investigation began. All methods were carried out in accordance with relevant guidelines and regulations.
Human and Animal Rights
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was approved by the ethics committee of Shanghai Normal University.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wang, Y., Wu, Q., Wang, Y. et al. The Formation Mechanism of Trust in Patient from Healthcare Professional’s Perspective: A Conditional Process Model. J Clin Psychol Med Settings 29, 760–772 (2022). https://doi.org/10.1007/s10880-021-09834-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10880-021-09834-9