Abstract
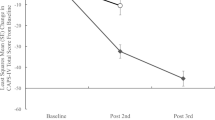
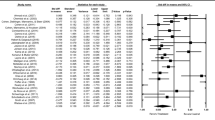
This study explored the relationship between injury severity and depressive symptoms for treatment-seeking individuals with traumatic brain injury (TBI). The Mayo Classification System was used to classify TBI severity in 72 participants who completed the Patient Health Questionnaire at admission and at dismissal from rehabilitation. Patients with mild TBI reported more depressive symptoms than those with moderate or severe TBI at admission and at dismissal. Although injury severity groups differed by gender composition, gender had no effect on severity of depressive symptoms. All participants reported fewer depressive symptoms at dismissal from rehabilitation, including lower endorsement of dysphoria by discharge. Participants with mild TBI, however, continued to report depressive symptoms of a mild severity at dismissal, with residual problems with anhedonia. These findings underscore the benefit of interdisciplinary post-acute rehabilitation services for persons with TBI of any severity, including those with mild injury.
Similar content being viewed by others
Abbreviations
- CBT:
-
Cognitive behavioral therapy
- MCS:
-
Mayo Classification System
- PHQ-9:
-
Patient Health Questionnaire
- PTSD:
-
Posttraumatic stress disorder
- TBI:
-
Traumatic brain injury
References
Alexander, M. P. (1992). Neuropsychiatric correlates of persistent postconcussive syndrome. The Journal of Head Trauma Rehabilitation, 7, 60–69.
Alway, Y., Gould, K. R., Johnston, L., McKenzie, D., & Ponsford, J. (2016). A prospective examination of Axis I psychiatric disorders in the first 5 years following moderate to severe traumatic brain injury. Psychological Medicine, 46, 1331–1341. https://doi.org/10.1017/S0033291715002986.
Batten, S. V., & Pollack, S. J. (2008). Integrative outpatient treatment for returning service members. Journal of Clinical Psychology, 64, 928–939. https://doi.org/10.1002/jclp.20513.
Belanger, H. G., Kretzmer, T., Vanderploeg, R. D., & French, L. M. (2010). Symptom complaints following combat-related traumatic brain injury: Relationship to traumatic brain injury severity and posttraumatic stress disorder. Journal of the International Neuropsychological Society, 16, 194–199. https://doi.org/10.1017/S1355617709990841.
Belanger, H. G., Vanderploeg, R. D., & Kretzmer, T. (2009). Symptom complaints following combat-related TBI: Relationship to TBI severity and PTSD. Clinical Neuropsychologist, 23, 570. https://doi.org/10.1080/13854040902867551.
Bombardier, C. H., Fann, J. R., Ludman, E. J., Vannoy, S. D., Dyer, J. R., Barber, J. K., & Temkin, N. R. (2017). The relations of cognitive, behavioral, and physical activity variables to depression severity in traumatic brain injury: Reanalysis of data from a randomized controlled trial. Journal of Head Trauma Rehabilitation, 32, 343–353. https://doi.org/10.1097/HTR.0000000000000288.
Bombardier, C. H., Fann, J. R., Temkin, N. R., Esselman, P. C., Barber, J., & Dikmen, S. S. (2010). Rates of major depressive disorder and clinical outcomes following traumatic brain injury. JAMA, 303, 1938–1945. https://doi.org/10.1001/jama.2010.599.
Bombardier, C. H., Hoekstra, T., Dikmen, S., & Fann, J. R. (2016). Depression trajectories during the first year after traumatic brain injury. Journal of Neurotrauma, 33, 2115–2124. https://doi.org/10.1089/neu.2015.4349.
Brooks, B. L., Silverberg, N., Maxwell, B., Mannix, R., Zafonte, R., Berkner, P. D., & Iverson, G. L. (2018). Investigating effects of sex differences and prior concussions on symptom reporting and cognition among adolescent soccer players. American Journal of Sports Medicine, 46, 961–968. https://doi.org/10.1177/0363546517749588.
Cicerone, K. D., Dahlberg, C., Malec, J. F., Langenbahn, D. M., Felicetti, T., Kneipp, S., … Catanese, J. (2005). Evidence-based cognitive rehabilitation: Updated review of the literature from 1998 through 2002. Archives of Physical Medicine and Rehabilitation, 86, 1681–1692. https://doi.org/10.1016/j.apmr.2005.03.024.
Cicerone, K. D., Langenbahn, D. M., Braden, C., Malec, J. F., Kalmar, K., Fraas, M., … Ashman, T. (2011). Evidence-based cognitive rehabilitation: Updated review of the literature from 2003 through 2008. Archives of Physical Medicine and Rehabilitation, 92, 519–530. https://doi.org/10.1016/j.apmr.2010.11.015.
Clark, D. C., Fawcett, J., Salazar-Grueso, E., & Fawcett, E. (1984). Seven-month clinical outcome of anhedonic and normally hedonic depressed inpatients. American Journal of Psychiatry, 141, 1216–1220. https://doi.org/10.1176/ajp.141.10.1216.
Cooper, D. B., Bowles, A. O., Kennedy, J. E., Curtiss, G., French, L. M., Tate, D. F., & Vanderploeg, R. D. (2017). Cognitive rehabilitation for military service members with mild traumatic brain injury: A randomized clinical trial. Journal of Head Trauma Rehabilitation, 32, E1–E15. https://doi.org/10.1097/HTR.0000000000000254.
Covassin, T., & Bay, E. (2012). Are there gender differences in cognitive function, chronic stress, and neurobehavioral symptoms after mild-to-moderate traumatic brain injury? Journal of Neuroscience Nursing, 44, 124–133. https://doi.org/10.1097/JNN.0b013e318252737d.
Deary, V., Chalder, T., & Sharpe, M. (2007). The cognitive behavioural model of medically unexplained symptoms: A theoretical and empirical review. Clinical Psychology Review, 27, 781–797. https://doi.org/10.1016/j.cpr.2007.07.002.
Dikmen, S. S., Bombardier, C. H., Machamer, J. E., Fann, J. R., & Temkin, N. R. (2004). Natural history of depression in traumatic brain injury. Archives of Physical Medicine and Rehabilitation, 85, 1457–1464.
Dimaggio, G., & Shahar, G. (2017). Behavioral activation as a common mechanism of change across different orientations and disorders. Psychotherapy (Chic), 54, 221–224. https://doi.org/10.1037/pst0000117.
Donders, J., & Pendery, A. (2017). Clinical utility of the Patient Health Questionnaire-9 in the assessment of major depression after broad-spectrum traumatic brain injury. Archives of Physical Medicine and Rehabilitation, 98, 2514–2519. https://doi.org/10.1016/j.apmr.2017.05.019.
Ernst, J., Faller, H., Koch, U., Brahler, E., Harter, M., Schulz, H., … Mehnert, A. (2018). Doctor’s recommendations for psychosocial care: Frequency and predictors of recommendations and referrals. PloS One, 13, e0205160. https://doi.org/10.1371/journal.pone.0205160.
Evans, C. C., Sherer, M., Nick, T. G., Nakase-Richardson, R., & Yablon, S. A. (2005). Early impaired self-awareness, depression, and subjective well-being following traumatic brain injury. Journal of Head Trauma Rehabilitation, 20, 488–500.
Fann, J. R., Bombardier, C. H., Dikmen, S., Esselman, P., Warms, C. A., Pelzer, E., … Temkin, N. (2005). Validity of the Patient Health Questionnaire-9 in assessing depression following traumatic brain injury. Journal of Head Trauma Rehabilitation, 20, 501–511.
Farrell-Carnahan, L., Barnett, S., Lamberty, G., Hammond, F. M., Kretzmer, T. S., Franke, L. M., … Nakase-Richardson, R. (2015). Insomnia symptoms and behavioural health symptoms in veterans 1 year after traumatic brain injury. Brain Injury, 29, 1400–1408.
Ferguson, R. J., & Mittenberg, W. (1996). Cognitive-behavioral treatment of postconcussion syndrome: A therapist’s manual. In V. B. Van Hasselt & M. Hersen (Eds.), Sourcebook of psychological treatment manuals for adult disorders (pp. 615–655). New York: Plenum Press.
Fleming, J. M., Strong, J., & Ashton, R. (1998). Cluster analysis of self-awareness levels in adults with traumatic brain injury and relationshipto outcome. Journal of Head Trauma Rehabilitation, 13, 39–51.
Fuentes, M. M., Bjornson, K., Christensen, A., Harmon, R., & Apkon, S. D. (2016). Disparities in functional outcomes during inpatient rehabilitation between American Indian/Alaska native and white children. Journal of Health Care for the Poor and Underserved, 27, 1080–1096. https://doi.org/10.1353/hpu.2016.0143.
Fuentes, M. M., Moore, M., Qiu, Q., Quistberg, A., Frank, M., & Vavilala, M. S. (2018). Differences in injury characteristics and outcomes for American Indian/Alaska native people hospitalized with traumatic injuries: An analysis of the national trauma data bank. J Racial Ethn Health Disparities. https://doi.org/10.1007/s40615-018-0529-3.
Fuentes, M. M., Thompson, L., Quistberg, D. A., Haaland, W. L., Rhodes, K., Kartin, D., … Rivara, F. P. (2017). Auditing access to outpatient rehabilitation services for children with traumatic brain injury and public insurance in Washington State. Archives of Physical Medicine and Rehabilitation, 98, 1763–1770 e1767. https://doi.org/10.1016/j.apmr.2016.12.013.
Gauvin-Lepage, J., Friedman, D., Grilli, L., & Gagnon, I. (2018). Effect of sex on recovery from persistent postconcussion symptoms in children and adolescents participating in an active rehabilitation intervention. Journal of Head Trauma Rehabilitation. https://doi.org/10.1097/HTR.0000000000000402.
Glintborg, C., & Hansen, T. G. (2016). Bio-psycho-social effects of a coordinated neurorehabilitation programme: A naturalistic mixed methods study. NeuroRehabilitation, 38, 99–113. https://doi.org/10.3233/NRE-161301.
Gomez-Hernandez, R., Max, J. E., Kosier, T., Paradiso, S., & Robinson, R. G. (1997). Social impairment and depression after traumatic brain injury. Archives of Physical Medicine and Rehabilitation, 78, 1321–1326.
Gunstad, J., & Suhr, J. A. (2001). “Expectation as etiology” versus “the good old days”: Postconcussion syndrome symptom reporting in athletes, headache sufferers, and depressed individuals. Journal of the International Neuropsychological Society, 7, 323–333.
Gunstad, J., & Suhr, J. A. (2002). Perception of illness: Nonspecificity of postconcussion syndrome symptom expectation. Journal of the International Neuropsychological Society, 8, 37–47.
Hart, T., Brenner, L., Clark, A. N., Bogner, J. A., Novack, T. A., Chervoneva, I., … Arango-Lasprilla, J. C. (2011). Major and minor depression after traumatic brain injury. Archives of Physical Medicine and Rehabilitation, 92, 1211–1219. https://doi.org/10.1016/j.apmr.2011.03.005.
Hart, T., Hoffman, J. M., Pretz, C., Kennedy, R., Clark, A. N., & Brenner, L. A. (2012). A longitudinal study of major and minor depression following traumatic brain injury. Archives of Physical Medicine and Rehabilitation, 93, 1343–1349. https://doi.org/10.1016/j.apmr.2012.03.036.
Hoem Nordhaug, L., Vik, A., Hagen, K., Stovner, L. J., Pedersen, T., Gravdahl, G. B., & Linde, M. (2016). Headaches in patients with previous head injuries: A population-based historical cohort study (HUNT). Cephalalgia, 36, 1009–1019. https://doi.org/10.1177/0333102415618948.
Hoge, C. W., McGurk, D., Thomas, J. L., Cox, A. L., Engel, C. C., & Castro, C. A. (2008). Mild traumatic brain injury in U.S. Soldiers returning from Iraq. New England Journal of Medicine, 358, 453–463. https://doi.org/10.1056/NEJMoa072972.
Iverson, G. L. (2005). Outcome from mild traumatic brain injury. Current Opinion in Psychiatry, 18, 301–317. https://doi.org/10.1097/01.yco.0000165601.29047.ae.
Iverson, G. L. (2006). Complicated vs uncomplicated mild traumatic brain injury: Acute neuropsychological outcome. Brain Injury, 20, 1335–1344.
Iverson, G. L., Zasler, N. D., & Lange, R. T. (2007). Post-concussive disorder. In N. D. Zasler, D. I. Katz & R. D. Zafonte (Eds.), Brain injury medicine: Principles and practice (pp. 373–405). New York: Demos Medical Publishing.
Janak, J. C., Cooper, D. B., Bowles, A. O., Alamgir, A. H., Cooper, S. P., Gabriel, K. P., … Orman, J. A. (2017). Completion of multidisciplinary treatment for persistent postconcussive symptoms is associated with reduced symptom burden. Journal of Head Trauma Rehabilitation, 32, 1–15. https://doi.org/10.1097/HTR.0000000000000202.
Jorge, R. E., Robinson, R. G., Arndt, S. V., Forrester, A. W., Geisler, F., & Starkstein, S. E. (1993). Comparison between acute- and delayed-onset depression following traumatic brain injury. Journal of Neuropsychiatry and Clinical Neurosciences, 5, 43–49. https://doi.org/10.1176/jnp.5.1.43.
Jorge, R. E., & Starkstein, S. E. (2005). Pathophysiologic aspects of major depression following traumatic brain injury. Journal of Head Trauma Rehabilitation, 20, 475–487.
Kroenke, K., Spitzer, R. L., & Williams, J. B. (2001). The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine, 16, 606–613.
Lange, R. T., Brickell, T., French, L. M., Ivins, B., Bhagwat, A., Pancholi, S., & Iverson, G. L. (2013). Risk factors for postconcussion symptom reporting after traumatic brain injury in U.S. military service members. Journal of Neurotrauma, 30, 237–246. https://doi.org/10.1089/neu.2012.2685.
Lewis, F. D., & Horn, G. J. (2017). Depression following traumatic brain injury: Impact on post-hospital residential rehabilitation outcomes. NeuroRehabilitation, 40, 401–410. https://doi.org/10.3233/NRE-161427.
Liossi, C., & Wood, R. L. (2009). Gender as a moderator of cognitive and affective outcome after traumatic brain injury. Journal of Neuropsychiatry and Clinical Neurosciences, 21, 43–51. https://doi.org/10.1176/appi.neuropsych.21.1.43.
Losoi, H., Silverberg, N. D., Waljas, M., Turunen, S., Rosti-Otajarvi, E., Helminen, M., … Iverson, G. L. (2016). Recovery from mild traumatic brain injury in previously healthy adults. Journal of Neurotrauma, 33, 766–776. https://doi.org/10.1089/neu.2015.4070.
Lucas, S., Hoffman, J. M., Bell, K. R., & Dikmen, S. (2014). A prospective study of prevalence and characterization of headache following mild traumatic brain injury. Cephalalgia, 34, 93–102. https://doi.org/10.1177/0333102413499645.
Malec, J. F., & Basford, J. S. (1996). Postacute brain injury rehabilitation. Archives of Physical Medicine and Rehabilitaion, 77, 198–207.
Malec, J. F., Brown, A. W., Leibson, C. L., Flaada, J. T., Mandrekar, J. N., Diehl, N. N., & Perkins, P. K. (2007). The Mayo classification system for traumatic brain injury severity. Journal of Neurotrauma, 24, 1417–1424. https://doi.org/10.1089/neu.2006.0245.
Malec, J. F., Brown, A. W., Moessner, A. M., Stump, T. E., & Monahan, P. (2010). A preliminary model for posttraumatic brain injury depression. Archives of Physical Medicine and Rehabilitation, 91, 1087–1097. https://doi.org/10.1016/j.apmr.2010.04.002.
Malec, J. F., Smigielski, J. S., DePompolo, R. W., & Thompson, J. M. (1993). Outcome evaluation and prediction in a comprehensive-integrated post-acute outpatient brain injury rehabilitation programme. Brain Injury, 7, 15–29.
Malec, J. F., Testa, J. A., Rush, B. K., Brown, A. W., & Moessner, A. M. (2007). Self-assessment of impairment, impaired self-awareness, and depression after traumatic brain injury. Journal of Head Trauma Rehabilitation, 22, 156–166. https://doi.org/10.1097/01.HTR.0000271116.12028.af.
Management of Concussion/mTBI Working Group. (2009). VA/DoD clinical practice guideline for management of concussion/mild traumatic brain injury. Journal of Rehabilitation Research and Development, 46, CP1–C68.
McCrea, M. (2008). Mild traumatic brain injury and postconcussion syndrome: The new evidence base for diagnosis and treatment. New York: Oxford University Press.
McCrea, M., Iverson, G. L., McAllister, T. W., Hammeke, T. A., Powell, M. R., Barr, W. B., & Kelly, J. P. (2009). An integrated review of recovery after mild traumatic brain injury (MTBI): Implications for clinical management. Clinical Neuropsychologist, 23, 1368–1390. https://doi.org/10.1080/13854040903074652.
McCrory, P., Meeuwisse, W. H., Aubry, M., Cantu, R. C., Dvorak, J., Echemendia, R. J., … Turner, M. (2013). Consensus statement on concussion in sport: The 4th International Conference on Concussion in Sport, Zurich, November 2012. Journal of Athletic Training, 48, 554–575. https://doi.org/10.4085/1062-6050-48.4.05.
Meagher, A. D., Beadles, C. A., Doorey, J., & Charles, A. G. (2015). Racial and ethnic disparities in discharge to rehabilitation following traumatic brain injury. Journal of Neurosurgery, 122, 595–601. https://doi.org/10.3171/2014.10.JNS14187.
Mittenberg, W., Canyock, E. M., Condit, D., & Patton, C. (2001). Treatment of post-concussion syndrome following mild head injury. Journal of Clinical and Experimental Neuropsychology, 23, 829–836. https://doi.org/10.1076/jcen.23.6.829.1022.
Mittenberg, W., DiGiulio, D. V., Perrin, S., & Bass, A. E. (1992). Symptoms following mild head injury: Expectation as aetiology. Journal of Neurology, Neurosurgery and Psychiatry, 55, 200–204.
Mittenberg, W., Tremont, G., Zielinski, R. E., Fichera, S., & Rayls, K. R. (1996). Cognitive-behavioral prevention of postconcussion syndrome. Archives of Clinical Neuropsychology, 11, 139–145.
Nampiaparampil, D. E. (2008). Prevalence of chronic pain after traumatic brain injury: A systematic review. JAMA, 300, 711–719. https://doi.org/10.1001/jama.300.6.711.
Nieto Fernandez, E., & Barraca Mairal, J. (2017). Behavioral activation versus cognitive restructuring to reduce automatic negative thoughts in anxiety generating situations. Psicothema, 29, 172–177. https://doi.org/10.7334/psicothema2016.325.
Obermeyer, Z., Samra, J. K., & Mullainathan, S. (2017). Individual differences in normal body temperature: Longitudinal big data analysis of patient records. BMJ, 359, j5468. https://doi.org/10.1136/bmj.j5468.
Ozen, L. J., & Fernandes, M. A. (2011). Effects of “diagnosis threat” on cognitive and affective functioning long after mild head injury. Journal of the International Neuropsychological Society, 17, 219–229. https://doi.org/10.1017/S135561771000144X.
Perrin, P. B., Krch, D., Sutter, M., Snipes, D. J., Arango-Lasprilla, J. C., Kolakowsky-Hayner, S. A., … Lequerica, A. (2014). Racial/ethnic disparities in mental health over the first 2 years after traumatic brain injury: A model systems study. Archives of Physical Medicine and Rehabilitation, 95, 2288–2295. https://doi.org/10.1016/j.apmr.2014.07.409.
Preiss-Farzanegan, S. J., Chapman, B., Wong, T. M., Wu, J., & Bazarian, J. J. (2009). The relationship between gender and postconcussion symptoms after sport-related mild traumatic brain injury. PM R, 1, 245–253. https://doi.org/10.1016/j.pmrj.2009.01.011.
Rapoport, M., McCauley, S., Levin, H., Song, J., & Feinstein, A. (2002). The role of injury severity in neurobehavioral outcome 3 months after traumatic brain injury. Neuropsychiatry, Neuropsychology, and Behavioral Neurology, 15, 123–132.
Rapoport, M. J., McCullagh, S., Streiner, D., & Feinstein, A. (2003a). Age and major depression after mild traumatic brain injury. American Journal of Geriatric Psychiatry, 11, 365–369.
Rapoport, M. J., McCullagh, S., Streiner, D., & Feinstein, A. (2003b). The clinical significance of major depression following mild traumatic brain injury. Psychosomatics, 44, 31–37. https://doi.org/10.1176/appi.psy.44.1.31.
Sacks, S. B. (2004). Rational emotive behavior therapy: Disputing irrational philosophies. Journal of Psychosocial Nursing and Mental Health Services, 42, 22–31.
Scheenen, M. E., Spikman, J. M., de Koning, M. E., van der Horn, H. J., Roks, G., Hageman, G., & van der Naalt, J. (2017). Patients “At Risk” of suffering from persistent complaints after mild traumatic brain injury: The role of coping, mood disorders, and post-traumatic stress. Journal of Neurotrauma, 34, 31–37. https://doi.org/10.1089/neu.2015.4381.
Schrader, G. D. (1997). Does anhedonia correlate with depression severity in chronic depression? Comprehensive Psychiatry, 38, 260–263.
Seidler, Z. E., Rice, S. M., Ogrodniczuk, J. S., Oliffe, J. L., & Dhillon, H. M. (2018). Engaging men in psychological treatment: A scoping review. American Journal of Men’s Health, 12, 1882–1900. https://doi.org/10.1177/1557988318792157.
Silverberg, N. D., Berkner, P. D., Atkins, J. E., Zafonte, R., & Iverson, G. L. (2016). Relationship between short sleep duration and preseason concussion testing. Clinical Journal of Sport Medicine, 26, 226–231. https://doi.org/10.1097/JSM.0000000000000241.
Silverberg, N. D., Hallam, B. J., Rose, A., Underwood, H., Whitfield, K., Thornton, A. E., & Whittal, M. L. (2013). Cognitive-behavioral prevention of postconcussion syndrome in at-risk patients: A pilot randomized controlled trial. Journal of Head Trauma Rehabilitation, 28, 313–322. https://doi.org/10.1097/HTR.0b013e3182915cb5.
Silverberg, N. D., & Iverson, G. L. (2013). Is rest after concussion “the best medicine?”: Recommendations for activity resumption following concussion in athletes, civilians, and military service members. Journal of Head Trauma Rehabilitation, 28, 250–259. https://doi.org/10.1097/HTR.0b013e31825ad658.
Singh, R., Mason, S., Lecky, F., & Dawson, J. (2018). Prevalence of depression after TBI in a prospective cohort: The SHEFBIT study. Brain Injury, 32, 84–90. https://doi.org/10.1080/02699052.2017.1376756.
Snell, D. L., Surgenor, L. J., Hay-Smith, E. J., Williman, J., & Siegert, R. J. (2015). The contribution of psychological factors to recovery after mild traumatic brain injury: Is cluster analysis a useful approach? Brain Injury, 29, 291–299. https://doi.org/10.3109/02699052.2014.976594.
Solomon, S. (2009). Post-traumatic headache: Commentary: An overview. Headache, 49, 1112–1115. https://doi.org/10.1111/j.1526-4610.2009.01462.x.
Speicher, S. M., Walter, K. H., & Chard, K. M. (2014). Interdisciplinary residential treatment of posttraumatic stress disorder and traumatic brain injury: Effects on symptom severity and occupational performance and satisfaction. American Journal of Occupational Therapy, 68, 412–421. https://doi.org/10.5014/ajot.2014.011304.
Suhr, J. A., & Gunstad, J. (2002a). “Diagnosis Threat”: The effect of negative expectations on cognitive performance in head injury. Journal of Clinical and Experimental Neuropsychology, 24, 448–457. https://doi.org/10.1076/jcen.24.4.448.1039.
Suhr, J. A., & Gunstad, J. (2002b). Postconcussive symptom report: The relative influence of head injury and depression. Journal of Clinical and Experimental Neuropsychology, 24, 981–993. https://doi.org/10.1076/jcen.24.8.981.8372.
Taylor, B. C., Campbell, H., Nugent, E., Bidelspach, S., Kehle-Forbes, D. E., Scholten, S. M., Sayer, J., N. A (2017). Three year trends in veterans health administration utilization and costs after traumatic brain injury screening among veterans with mild traumatic brain injury. Journal of Neurotrauma, 34, 2567–2574. https://doi.org/10.1089/neu.2016.4910.
Trontel, H. G., Hall, S., Ashendorf, L., & O’Connor, M. K. (2013). Impact of diagnosis threat on academic self-efficacy in mild traumatic brain injury. Journal of Clinical and Experimental Neuropsychology, 35, 960–970. https://doi.org/10.1080/13803395.2013.844770.
van Dongen, C. H., Goossens, P. H., van Zee, I. E., Verpoort, K. N., Vlieland, T. P. V., & van Velzen, J. M. (2018). Short-term and long-term outcomes of a vocational rehabilitation program for patients with acquired brain injury in the Netherlands. Journal of Occupational Rehabilitation, 28, 523–530. https://doi.org/10.1007/s10926-017-9738-6.
Vetter, P. H., Pritzbuer, J. V., Jungmann, K., Moises, H. W., Koller, O., & Kropp, P. (2000). Motivation to seek psychotherapy in patients with recurrent depressive disorder. Psychotherapy Research, 10, 159–168. https://doi.org/10.1080/713663672.
Waldron-Perrine, B., Hennrick, H., Spencer, R. J., Pangilinan, P. H., & Bieliauskas, L. A. (2014). Postconcussive symptom report in polytrauma: Influence of mild traumatic brain injury and psychiatric distress. Military Medicine, 179, 856–864. https://doi.org/10.7205/MILMED-D-13-00282.
Wardlaw, C., Hicks, A. J., Sherer, M., & Ponsford, J. L. (2018). Psychological resilience is associated with participation outcomes following mild to severe traumatic brain injury. Frontiers in Neurology, 9, 563. https://doi.org/10.3389/fneur.2018.00563.
Funding
This study received no funding for creation of the database, analysis of the data, or any other aspect of the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Matthew R. Powell, Allen W. Brown, Danielle Klunk, Jennifer R. Geske, Kamini Krishnan, Cassie Green, Thomas F. Bergquist declare that they have no conflict of interest.
Human and Animal Rights
The Mayo Clinic Institutional Review Board approved this study, which was considered to pose minimal risk to patients. The data, which consisted of patient responses to questionnaires, were collected from patient medical records and coded in a manner to ensure confidentiality; no specimens were collected.
Informed Consent
For this type of study, formal consent is not required (the requirement was waived after institutional review board review).
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Powell, M.R., Brown, A.W., Klunk, D. et al. Injury Severity and Depressive Symptoms in a Post-acute Brain Injury Rehabilitation Sample. J Clin Psychol Med Settings 26, 470–482 (2019). https://doi.org/10.1007/s10880-019-09602-w
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10880-019-09602-w