Abstract
Purpose
The compensatory reserve metric (CRM) is a novel tool to predict cardiovascular decompensation during hemorrhage. The CRM is traditionally computed using waveforms obtained from photoplethysmographic volume-clamp (PPGVC), yet invasive arterial pressures may be uniquely available. We aimed to examine the level of agreement of CRM values computed from invasive arterial-derived waveforms and values computed from PPGVC-derived waveforms.
Methods
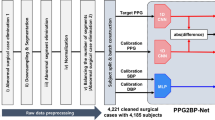
Sixty-nine participants underwent graded lower body negative pressure to simulate hemorrhage. Waveform measurements from a brachial arterial catheter and PPGVC finger-cuff were collected. A PPGVC brachial waveform was reconstructed from the PPGVC finger waveform. Thereafter, CRM values were computed using a deep one-dimensional convolutional neural network for each of the following source waveforms; (1) invasive arterial, (2) PPGVC brachial, and (3) PPGVC finger. Bland-Altman analyses were used to determine the level of agreement between invasive arterial CRM values and PPGVC CRM values, with results presented as the Mean Bias [95% Limits of Agreement].
Results
The mean bias between invasive arterial- and PPGVC brachial CRM values at rest, an applied pressure of -45mmHg, and at tolerance was 6% [-17%, 29%], 1% [-28%, 30%], and 0% [-25%, 25%], respectively. Additionally, the mean bias between invasive arterial- and PPGVC finger CRM values at rest, applied pressure of -45mmHg, and tolerance was 2% [-22%, 26%], 8% [-19%, 35%], and 5% [-15%, 25%], respectively.
Conclusion
There is generally good agreement between CRM values obtained from invasive arterial waveforms and values obtained from PPGVC waveforms. Invasive arterial waveforms may serve as an alternative for computation of the CRM.





Similar content being viewed by others
Data availability
All data pertaining to the study will be made available upon reasonable request to the corresponding author.
References
Sevransky J. Clinical assessment of hemodynamically unstable patients. Curr Opin Crit Care. 2009;15:234–8.
Bajwa EK, Malhotra A, Thompson BT. Methods of monitoring shock. Semin Respir Crit Care Med. 2004;25:629–44.
Ward KR, Tiba MH, Ryan KL, Torres Filho IP, Rickards CA, Witten T, et al. Oxygen transport characterization of a human model of progressive hemorrhage. Resuscitation. 2010;81:987–93.
Convertino VA, Koons NJ. The compensatory reserve: potential for accurate individualized goal-directed whole blood resuscitation. Transfusion. 2020;60:S150–7.
Convertino VA, Sawka MN. Wearable technology for compensatory reserve to sense hypovolemia. J Appl Physiol (1985). 2018;124:442–51.
Convertino VA, Grudic G, Mulligan J, Moulton S. Estimation of individual-specific progression to impending cardiovascular instability using arterial waveforms. J Appl Physiol (1985). 2013;115:1196–202.
Koons NJ, Nguyen B, Suresh MR, Hinojosa-Laborde C, Convertino VA. Tracking DO2 with Compensatory Reserve during whole blood resuscitation in baboons. Shock. 2020;53:327–34.
Benov A, Yaslowitz O, Hakim T, Amir-Keret R, Nadler R, Brand A, et al. The effect of blood transfusion on compensatory reserve: a prospective clinical trial. J Trauma Acute Care Surg. 2017;83:S71.
Janak JC, Howard JT, Goei KA, Weber R, Muniz GW, Hinojosa-Laborde C, et al. Predictors of the onset of hemodynamic decompensation during Progressive Central Hypovolemia: comparison of the Peripheral Perfusion Index, pulse pressure variability, and Compensatory Reserve Index. Shock. 2015;44:548.
Ciaraglia A, Osta E, Wang H, Cigarroa F, Thomas E, Fritze D, et al. Evidence for beneficial use of the compensatory reserve measurement in guiding intraoperative resuscitation: a prospective study of orthotopic liver transplant recipients. Shock. 2024;61:61.
Benov A, Brand A, Rozenblat T, Antebi B, Ben-Ari A, Amir-Keret R, et al. Evaluation of sepsis using compensatory reserve measurement: a prospective clinical trial. J Trauma Acute Care Surg. 2020;89:S153–60.
Convertino VA, Wirt MD, Glenn JF, Lein BC. The Compensatory Reserve for early and accurate prediction of hemodynamic compromise: a review of the underlying physiology. Shock. 2016;45:580–90.
Convertino VA, Schauer SG, Weitzel EK, Cardin S, Stackle ME, Talley MJ, et al. Wearable Sensors Incorporating Compensatory Reserve Measurement for Advancing Physiological Monitoring in critically injured trauma patients. Sensors. 2020;20:6413.
Bos WJ, van Goudoever J, van Montfrans GA, van den Meiracker AH, Wesseling KH. Reconstruction of brachial artery pressure from noninvasive finger pressure measurements. Circulation. 1996;94:1870–5.
Martina JR, Westerhof BE, van Goudoever J, de Beaumont EMFH, Truijen J, Kim Y-S, et al. Noninvasive continuous arterial blood pressure monitoring with Nexfin®. Anesthesiology. 2012;116:1092–103.
Bartels K, Thiele RH. Advances in photoplethysmography: beyond arterial oxygen saturation. Can J Anesth/J Can Anesth. 2015;62:1313–28.
Techentin RW, Felton CL, Schlotman TE, Gilbert BK, Joyner MJ, Curry TB et al. 1D Convolutional Neural Networks for Estimation of Compensatory Reserve from Blood Pressure Waveforms. 2019 41st Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC). 2019. pp. 2169–73.
Stewart CL, Mulligan J, Grudic GZ, Talley ME, Jurkovich GJ, Moulton SL. The Compensatory Reserve Index following Injury: results of a prospective clinical trial. Shock. 2016;46:61–7.
Trieu HT, Khanh LP, Ming DKY, Quang CH, Phan TQ, Van VCN, et al. The compensatory reserve index predicts recurrent shock in patients with severe dengue. BMC Med. 2022;20:109.
Convertino VA, Cardin S. Advanced medical monitoring for the battlefield: a review on clinical applicability of compensatory reserve measurements for early and accurate hemorrhage detection. J Trauma Acute Care Surg. 2022;93:S147.
Giavarina D. Understanding bland Altman analysis. Biochemia Med. 2015;25:141–51.
Bunce C, Correlation. Agreement, and bland–Altman Analysis: statistical analysis of Method Comparison studies. Am J Ophthalmol. 2009;148:4–6.
Wampler MR, Johnson MC, Alarhayem AQ, Convertino VA, Chung KK, Stewart R, et al. Establishing threshold variables for the dashboard view of the Compensatory Reserve Measurement. J Am Coll Surg. 2018;227:S263.
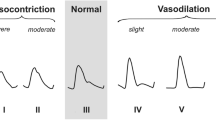
Ciaraglia AV, Convertino VA, Johnson MC, DeRosa M, Nicholson SE, Eastridge BJ. Compensatory reserve and pulse character: enhanced potential to predict urgency for transfusion and other life-saving interventions after traumatic injury. Transfusion. 2022;62:S130–8.
Rickards CA, Ryan KL, Cooke WH, Convertino VA. Tolerance to central hypovolemia: the influence of oscillations in arterial pressure and cerebral blood velocity. J Appl Physiol (1985). 2011;111:1048–58.
Castaneda D, Esparza A, Ghamari M, Soltanpur C, Nazeran H. A review on wearable photoplethysmography sensors and their potential future applications in health care. Int J Biosens Bioelectron. 2018;4:195–202.
Fine J, Branan KL, Rodriguez AJ, Boonya-ananta T, Ajmal, Ramella-Roman JC, et al. Sources of inaccuracy in Photoplethysmography for continuous Cardiovascular monitoring. Biosens (Basel). 2021;11:126.
Scheer B, Perel A, Pfeiffer UJ. Clinical review: complications and risk factors of peripheral arterial catheters used for haemodynamic monitoring in anaesthesia and intensive care medicine. Crit Care. 2002;6:199–204.
Parati G, Casadei R, Groppelli A, Di Rienzo M, Mancia G. Comparison of finger and intra-arterial blood pressure monitoring at rest and during laboratory testing. Hypertension. 1989;13:647–55.
Sasser SM, Hunt RC, Faul M, Sugerman D, Pearson WS, Dulski T et al. Guidelines for Field Triage of Injured Patients: Recommendations of the National Expert Panel on Field Triage, 2011. Morbidity and Mortality Weekly Report: Recommendations and Reports. 2012;61:1–20.
Tobias JD. Strategies for minimizing blood loss in orthopedic surgery. Semin Hematol. 2004;41:145–56.
Romagnoli S, Ricci Z, Quattrone D, Tofani L, Tujjar O, Villa G, et al. Accuracy of invasive arterial pressure monitoring in cardiovascular patients: an observational study. Crit Care. 2014;18:644.
Convertino VA, Schiller AM. Measuring the compensatory reserve to identify shock. J Trauma Acute Care Surg. 2017;82:S57–65.
Ciaraglia A, Convertino VA, Wang H, Cigarroa F, Thomas E, Fritze D, et al. Intraoperative Use of Compensatory Reserve Measurement in Orthotopic Liver Transplant: Improved Sensitivity for the prediction of hypovolemic events. Mil Med. 2023;188:322–7.
Stewart CL, Nawn CD, Mulligan J, Grudic G, Moulton SL, Convertino VA. Compensatory Reserve for early and accurate prediction of hemodynamic compromise: Case studies for clinical utility in Acute Care and Physical Performance. J Spec Oper Med. 2016;16:6–13.
Frezza EE, Mezghebe H. Indications and complications of arterial catheter use in surgical or medical intensive care units: analysis of 4932 patients. Am Surg. 1998;64:127–31.
Pinsky MR. Hemodynamic monitoring in the intensive care unit. Clin Chest Med. 2003;24:549–60.
Perner A, Cecconi M, Cronhjort M, Darmon M, Jakob SM, Pettilä V, et al. Expert statement for the management of hypovolemia in sepsis. Intensive Care Med. 2018;44:791–8.
Ragaller MJ, Theilen H, Koch T. Volume replacement in critically ill patients with acute renal failure. J Am Soc Nephrol. 2001;12(Suppl 17):S33–39.
Rackow EC, Falk JL, Fein IA, Siegel JS, Packman MI, Haupt MT, et al. Fluid resuscitation in circulatory shock: a comparison of the cardiorespiratory effects of albumin, hetastarch, and saline solutions in patients with hypovolemic and septic shock. Crit Care Med. 1983;11:839.
Acknowledgements
The authors sincerely thank all participants within the study. We acknowledge the contributions of the Mayo Clinic Clinical Research and Trials Unit (CRTU), the Special Purpose Processor Development Group (SPPDG), as well as the assistance of the members of the Human Integrative Physiology Lab, Shelly K. Roberts, Nancy J. Meyer, Pam A. Engrav, Olaf H. Morkeberg, Ellen K. Gorman, Jonathon W. Senefeld, and Cecile El-Borgi.
Funding
The presented work was funded in part by the Congressionally Directed Medical Research Program (Award No. DM180240).
Author information
Authors and Affiliations
Contributions
All authors take responsibility for the integrity, accuracy, and interpretation of the information and data presented in this report. T.B.C., V.A.C., M.J.J., C.R.H., and D.R.H conceived the presented study. K.L.W., W.W.P, R.J.P., R.W.T, C.P.J, R.J.R, K.J.B., D.R.H., C.R.H., and C.C.W. assisted with data collection. K.L.W. and W.W.P. performed data processing, data analyses, and drafted the original manuscript. All authors revised the manuscript and approved the final version of the article.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest. The opinions or assertions contained herein are the private views of the authors and are not to be construed as official or as reflecting the views of the Department of the Army, Department of the Navy, or the Department of Defense.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Webb, K.L., Pruter, W.W., Poole, R.J. et al. Comparing the compensatory reserve metric obtained from invasive arterial measurements and photoplethysmographic volume-clamp during simulated hemorrhage. J Clin Monit Comput (2024). https://doi.org/10.1007/s10877-024-01166-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10877-024-01166-x