Abstract
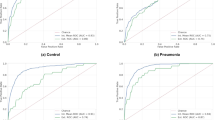
Capnography monitors trigger high priority ‘no breath’ alarms when CO2 measurements do not exceed a given threshold over a specified time-period. False alarms occur when the underlying breathing pattern is stable, but the alarm is triggered when the CO2 value reduces even slightly below the threshold. True ‘no breath’ events can be falsely classified as breathing if waveform artifact causes an aberrant spike in CO2 values above the threshold. The aim of this study was to determine the accuracy of a deep learning approach to classifying segments of capnography waveforms as either ‘breath’ or ‘no breath’. A post hoc secondary analysis of data from 9 North American sites included in the PRediction of Opioid-induced Respiratory Depression In Patients Monitored by capnoGraphY (PRODIGY) study was conducted. We used a convolutional neural network to classify 15 s capnography waveform segments drawn from a random sample of 400 participants. Loss was calculated over batches of 32 using the binary cross-entropy loss function with weights updated using the Adam optimizer. Internal-external validation was performed by iteratively fitting the model using data from all but one hospital and then assessing its performance in the remaining hospital. The labelled dataset consisted of 10,391 capnography waveform segments. The neural network’s accuracy was 0.97, precision was 0.97 and recall was 0.96. Performance was consistent across hospitals in internal-external validation. The neural network could reduce false capnography alarms. Further research is needed to compare the frequency of alarms derived from the neural network with the standard approach.









Similar content being viewed by others
Abbreviations
- AUROC:
-
Area under the receiver operating characteristics curve
- ETCO2 :
-
End-tidal carbon dioxide
- CO2:
-
Carbon dioxide
References
Drew BJ, Harris P, Zegre-Hemsey JK, et al. Insights into the problem of alarm fatigue with physiologic monitor devices: a comprehensive observational study of consecutive intensive care unit patients. PLoS ONE. 2014;9(10):e110274.
Winters BD, Cvach MM, Bonafide CP, et al. Technological distractions (part 2): a summary of approaches to manage clinical alarms with intent to reduce alarm fatigue. Crit Care Med. 2018;46(1):130–7.
Cvach M. Monitor alarm fatigue: an integrative review. Biomed Instrum Technol. 2012;46(4):268–77.
Wallis L. Alarm fatigue linked to patient’s death. AJN Am J Nurs. 2010;110(7):16.
Sun Z, Sessler DI, Dalton JE, et al. Postoperative hypoxemia is common and persistent: a prospective blinded observational study. Anesth Analg. 2015;121(3):709.
Overdyk F, Dahan A, Roozekrans M, der Schrier R, Aarts L, Niesters M. Opioid-induced respiratory depression in the acute care setting: a compendium of case reports. Pain Manag. 2014;4(4):317–25. https://doi.org/10.2217/pmt.14.19.
Khanna AK, Saager L, Bergese SD, et al. Opioid-induced respiratory depression increases hospital costs and length of stay in patients recovering on the general care floor. BMC Anesthesiol. 2021;21(1):1–12.
Khanna AK, Bergese SD, Jungquist CR, et al. Prediction of opioid-induced respiratory depression on inpatient wards using continuous capnography and oximetry: an international prospective, observational trial. Anesth Analg. 2020;131(4):1012. https://doi.org/10.1213/ANE.0000000000004788.
Pedregosa F, Michel V, Grisel O, et al. Scikit-learn: machine learning in python. J Mach Learn Res. 2011;12:2825–30.
He K, Zhang X, Ren S, Sun J. Deep residual learning for image recognition. In: Proceedings of the IEEE Conference on Computer Vision and Pattern Recognition (CVPR). 2016;770–778.
Smith LN. Cyclical learning rates for training neural networks. Proceedings – 2017 IEEE Winter Conference on Applications of Computer Vision, WACV 2017. Published online May 11, 2017:464–472. https://doi.org/10.1109/WACV.2017.58.
Abadi M, Barham P, Chen J et al. TensorFlow: a system for large-scale machine learning. In: 12th USENIX symposium on operating systems design and implementation (OSDI 16). USENIX Association; 2016:265–283. https://www.usenix.org/conference/osdi16/technical-sessions/presentation/abadi.
Seabold S, Perktold J, Statsmodels. Econometric and statistical modeling with python. In: Proceedings of the 9th Python in Science Conference. 2010;57:10-25080.
Steyerberg EW, Harrell FE Jr. Prediction models need appropriate internal, internal-external, and external validation. J Clin Epidemiol. 2016;69:245–7. https://doi.org/10.1016/j.jclinepi.2015.04.005.
Urman RD, Khanna AK, Bergese SD, et al. Postoperative opioid administration characteristics associated with opioid-induced respiratory depression: results from the PRODIGY trial. J Clin Anesth. 2021;70:110167.
Waljee JF, Zhong L, Hou H, Sears E, Brummet C, Chung KC. The utilization of opioid analgesics following common upper extremity surgical procedures: a national, population-based study. Plast Reconstr Surg. 2016;137(2):355e.
Bhagya D, Manikandan S. Speed of sound-based capnographic sensor with second-generation CNN for automated classification of cardiorespiratory abnormalities. IEEE Sens J. 2019;19(19):8887–94.
Mieloszyk RJ, Verghese GC, Deitch K, et al. Automated quantitative analysis of capnogram shape for COPD–normal and COPD–CHF classification. IEEE Trans Biomed Eng. 2014;61(12):2882–90.
Bhagya D, Suchetha M. A 1-D deformable convolutional neural network for the quantitative analysis of capnographic sensor. IEEE Sens J. 2020;21(5):6672–8.
Pertzov B, Ronen M, Rosengarten D, et al. Use of capnography for prediction of obstruction severity in non-intubated COPD and asthma patients. Respir Res. 2021;22(1):1–9.
El-Badawy IM, Singh OP, Omar Z. Automatic classification of regular and irregular capnogram segments using time-and frequency-domain features: a machine learning-based approach. Technol Health Care. 2021;29(1):59–72.
El-Badawy IM, Omar Z, Singh OP. An effective machine learning approach for classifying artefact-free and distorted capnogram segments using simple time-domain features. IEEE Access. 2022;10:8767–78. https://doi.org/10.1109/ACCESS.2022.3143617.
Jaffe MB. Using the features of the time and volumetric capnogram for classification and prediction. J Clin Monit Comput. 2017;31(1):19–41.
Herry CL, Townsend D, Green GC, Bravi A, Seely AJE. Segmentation and classification of capnograms: application in respiratory variability analysis. Physiol Meas. 2014;35(12):2343. https://doi.org/10.1088/0967-3334/35/12/2343.
Smith SW, Walsh B, Grauer K, et al. A deep neural network learning algorithm outperforms a conventional algorithm for emergency department electrocardiogram interpretation. J Electrocardiol. 2019;52:88–95. https://doi.org/10.1016/J.JELECTROCARD.2018.11.013.
Maille B, Wilkin M, Million M, et al. Smartwatch electrocardiogram and artificial intelligence for assessing cardiac-rhythm safety of drug therapy in the COVID-19 pandemic. The QT-logs study. Int J Cardiol. 2021;331:333–9. https://doi.org/10.1016/J.IJCARD.2021.01.002.
Fiorina L, Maupain C, Gardella C, et al. Evaluation of an ambulatory ECG analysis platform using deep neural networks in routine clinical practice. J Am Heart Assoc. 2022;11(18):26196. https://doi.org/10.1161/JAHA.122.026196.
Brattain LJ, Pierce TT, Gjesteby LA, et al. AI-enabled, ultrasound-guided handheld robotic device for femoral vascular access. Biosens 2021. 2021;11(12):522. https://doi.org/10.3390/BIOS11120522.
Mafeld S, Musing ELS, Conway A, Kennedy S, Oreopoulos G, Rajan D. Avoiding and managing error in interventional radiology practice: tips and tools. Can Assoc Radiol J. 2020;71(4):528–35. https://doi.org/10.1177/0846537119899215.
Conway A, Collins P, Chang K, et al. Pre-apneic capnography waveform abnormalities during procedural sedation and analgesia. J Clin Monit Comput. 2020;34(5):1061–8.
Conway A, Jungquist CR, Chang K, et al. Predicting prolonged apnea during nurse-administered procedural sedation: machine learning study. JMIR Perioper Med. 2021;4(2):e29200.
Conway A, Rolley J, Page K, Fulbrook P. Issues and challenges associated with nurse-administered procedural sedation and analgesia in the cardiac catheterisation laboratory: a qualitative study. J Clin Nurs. 2014;23(3–4):374–84.
Conway A, Collins P, Chang K, et al. High flow nasal oxygen during procedural sedation for cardiac implantable electronic device procedures: a randomised controlled trial. Eur J Anaesthesiology. 2021;38(8):839–49.
Howard JP, Cook CM, van de Hoef TP, et al. Artificial Intelligence for aortic pressure Waveform Analysis during Coronary Angiography: machine learning for Patient Safety. JACC Cardiovasc Interv. 2019;12(20):2093–101. https://doi.org/10.1016/J.JCIN.2019.06.036.
Arnold AD, Howard JP, Gopi A, et al. Discriminating electrocardiographic responses to his-bundle pacing using machine learning. Cardiovasc Digit Health J. 2020;1(1):11–20. https://doi.org/10.1016/J.CVDHJ.2020.07.001.
Funding
Data from this study were obtained from the PRODIGY trial, which was funded by Medtronic. The current study received no funding.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Labelling of data was performed by AC and MG. Data analysis was performed by AC and WZ. The first draft of the manuscript was written by AC and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Conway, A., Goudarzi Rad, M., Zhou, W. et al. Deep learning classification of capnography waveforms: secondary analysis of the PRODIGY study. J Clin Monit Comput 37, 1327–1339 (2023). https://doi.org/10.1007/s10877-023-01028-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-023-01028-y