Abstract
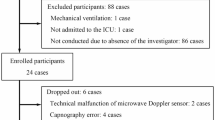
Our aim was to determine the agreement of heart rate (HR) and respiratory rate (RR) measurements by the Philips Biosensor with a reference monitor (General Electric Carescape B650) in severely obese patients during and after bariatric surgery. Additionally, sensor reliability was assessed. Ninety-four severely obese patients were monitored with both the Biosensor and reference monitor during and after bariatric surgery. Agreement was defined as the mean absolute difference between both monitoring devices. Bland Altman plots and Clarke Error Grid analysis (CEG) were used to visualise differences. Sensor reliability was reflected by the amount, duration and causes of data loss. The mean absolute difference for HR was 1.26 beats per minute (bpm) (SD 0.84) during surgery and 1.84 bpm (SD 1.22) during recovery, and never exceeded the 8 bpm limit of agreement. The mean absolute difference for RR was 1.78 breaths per minute (brpm) (SD 1.90) during surgery and 4.24 brpm (SD 2.75) during recovery. The Biosensor’s RR measurements exceeded the 2 brpm limit of agreement in 58% of the compared measurements. Averaging 15 min of measurements for both devices improved agreement. CEG showed that 99% of averaged RR measurements resulted in adequate treatment. Data loss was limited to 4.5% of the total duration of measurements for RR. No clear causes for data loss were found. The Biosensor is suitable for remote monitoring of HR, but not RR in morbidly obese patients. Future research should focus on improving RR measurements, the interpretation of continuous data, and development of smart alarm systems.




Similar content being viewed by others

Availability of data and material
Data is available upon reasonable request
Code availability
We used the statistical software R (version 3.6.1, www.r-project.org). Figures were created using the R-package ‘ggplot2’.
References
Tevis SE, Kennedy GE. Postoperative complications and implications on patient-centered outcomes. J Surg Res. 2013;181:106–13. https://doi.org/10.1016/j.jss.2013.01.032.
Beth Smith ME, Chiovaro JC, O’Neil M, et al. Early warning system scores for clinical deterioration in hospitalized patients: a systematic review. Ann Am Thorac Soc. 2014;11:1454–65. https://doi.org/10.1513/AnnalsATS.201403-102OC.
Alam N, Hobbelink EL, van Tienhoven AJ, Van de Ven PM, Jansma EP, Nanayakkara PWB. The impact of the use of the Early Warning Score (EWS) on patient outcomes: a systematic review. Resuscitation. 2014;85:587–94. https://doi.org/10.1016/j.resuscitation.2014.01.013.
Cretikos MA, Bellomo R, Hillman K, Chen J, Finfer S, Flabouris A. Respiratory rate: the neglected vital sign. Med J Aust. 2008;188:657–9. https://doi.org/10.5694/j.1326-5377.2008.tb01825.x.
Subbe CP, Davies RG, Williams E, Rutherford P, Gemmell L. Effect of introducing the Modified Early Warning score on clinical outcomes, cardio-pulmonary arrests and intensive care utilisation in acute medical admissions. Anaesthesia. 2003;58:797–802. https://doi.org/10.1046/j.1365-2044.2003.03258.x.
Fieselmann JF, Hendryx MS, Helms CM, Wakefield DS. Respiratory rate predicts cardiopulmonary arrest for internal medicine inpatients. J Gen Intern Med. 1993;8:354–60. https://doi.org/10.1007/BF02600071.
Young MP, Gooder VJ, McBride K, James B, Fisher ES. Inpatient transfers to the intensive care unit: delays are associated with increased mortality and morbidity. J Gen Intern Med. 2003;18:77–83. https://doi.org/10.1046/j.1525-1497.2003.20441.x.
Pashikanti L, Von Ah D. Impact of early mobilization protocol on the medical-surgical inpatient population: an integrated review of literature. Clin Nurse Spec. 2012;26:87–94. https://doi.org/10.1097/NUR.0b013e31824590e6.
Markey DW, Brown RJ. An interdisciplinary approach to addressing patient activity and mobility in the medical-surgical patient. J Nurs Care Qual. 2002;16:1–12. https://doi.org/10.1097/00001786-200207000-00002.
Joshi M, Ashrafian H, Aufegger L, Khan S, Arora S, Cooke G, Darzi A. Wearable sensors to improve detection of patient deterioration. Expert Rev Med Dev. 2019;16:145–54. https://doi.org/10.1080/17434440.2019.1563480.
Boer C, Touw HR, Loer SA. Postanesthesia care by remote monitoring of vital signs in surgical wards. Curr Opin Anaesthesiol. 2018;31:716–22. https://doi.org/10.1097/ACO.0000000000000650.
Watkins T, Whisman L, Booker P. Nursing assessment of continuous vital sign surveillance to improve patient safety on the medical/surgical unit. J Clin Nurs. 2016;25:278–81. https://doi.org/10.1111/jocn.13102.
Saugel B, Hoppe P, Khanna AK. Automated continuous noninvasive ward monitoring: validation of measurement systems is the real challenge. Anesthesiology. 2020;132:407–10. https://doi.org/10.1097/ALN.0000000000003100.
Michard F, Kalkman CJ. Rethinking patient surveillance on hospital wards. Anesthesiology. 2021;135:531–40. https://doi.org/10.1097/ALN.0000000000003843.
Izmailova ES, McLean IL, Bhatia G, et al. Evaluation of wearable digital devices in a phase I clinical trial. Clin Transl Sci. 2019;12:247–56. https://doi.org/10.1111/cts.12602.
Breteler MJMM, Huizinga E, van Loon K, Leenen LPH, Dohmen DAJ, Kalkman CJ, Blokhuis TJ. Reliability of wireless monitoring using a wearable patch sensor in high-risk surgical patients at a step-down unit in the Netherlands: a clinical validation study. BMJ Open. 2018;8:e020162. https://doi.org/10.1136/bmjopen-2017-020162.
Selvaraj N, Nallathambi G, Moghadam R, Aga A. Fully disposable wireless patch sensor for continuous remote patient monitoring. Conf Proc IEEE Eng Med Biol Soc. 2018. https://doi.org/10.1109/EMBC.2018.8512569.
Koenders N, Seeger JPH, Van Der Giessen T, et al. Validation of a wireless patch sensor to monitor mobility tested in both an experimental and a hospital setup: a cross-sectional study. PLoS ONE. 2018;13:e0206304. https://doi.org/10.1371/journal.pone.0206304.
Weenk M, Koeneman M, van de Belt TH, Engelen LJLPG, Van Goor H, Bredie SJH. Wireless and continuous monitoring of vital signs in patients at the general ward. Resuscitation. 2019;136:47–53. https://doi.org/10.1016/j.resuscitation.2019.01.017.
Weenk M, van Goor H, Frietman B, et al. Continuous Monitoring of Vital Signs Using Wearable Devices on the General Ward: Pilot Study. JMIR mHealth uHealth. 2017;5:91. https://doi.org/10.2196/mhealth.7208.
Li T, Divatia S, McKittrick J, Moss J, Hijnen NM, Becker LB. A pilot study of respiratory rate derived from a wearable biosensor compared with capnography in emergency department patients. Open Access Emerg Med. 2019;11:103–8. https://doi.org/10.2147/OAEM.S198842.
Selvaraj N, Nallathambi G, Kettle P. A novel synthetic simulation platform for validation of breathing rate measurement. Conf Proc IEEE Eng Med Biol Soc. 2018. https://doi.org/10.1109/EMBC.2018.8512352.
Breteler MJM, KleinJan EJ, Dohmen DAJ, et al. Vital signs monitoring with wearable sensors in high-risk surgical patients: a clinical validation study. Anesthesiology. 2019;132:424–39. https://doi.org/10.1097/ALN.0000000000003029.
Finucane MM, Stevens GA, Cowan MJ, et al. National, regional, and global trends in body-mass index since 1980: systematic analysis of health examination surveys and epidemiological studies with 960 country-years and 9.1 million participants. Lancet. 2011;377:557–67. https://doi.org/10.1016/S0140-6736(10)62037-5.
Chan AM, Ferdosi N, Narasimhan R. Ambulatory respiratory rate detection using ECG and a triaxial accelerometer. Annu Int Conf IEEE Eng Med Biol Soc. 2013. https://doi.org/10.1109/EMBC.2013.6610436.
Subbe CP, Kruger M, Rutherford P, Gemmel L. Validation of a modified Early Warning Score in medical admissions. QJM. 2001;94:521–6.
Wickham H. ggplot2: elegant graphics for data analysis. New York: Springer; 2016.
Schmolze D (2017). ega: Error Grid Analysis. R package version 2.0.0. https://CRAN.R-project.org/package=ega
Keim-Malpass J, Clark MT, Lake DE, Moorman JR. Towards development of alert thresholds for clinical deterioration using continuous predictive analytics monitoring. J Clin Monit Comput. 2020;34(4):797–804. https://doi.org/10.1007/s10877-019-00361-5.
Van Rossum MC, Vlaskamp LB, Posthuma LM, Visscher MJ, Breteler MJM, Hermens HJ, Kalkman CJ, Preckel B. Adaptive threshold-based alarm strategies for continuous vital signs monitoring. J Clin Monit Comput. 2021. https://doi.org/10.1007/s10877-021-00666-4.
Acknowledgements
NK and GMP contributed equally to this work. The authors would like to thank the following persons from Rijnstate Hospital: José W.J.M. Geurts PhD and Pascal S.H. Smulders MSc, Department of Anesthesiology and Pain Management, for logistical support, Sjoerd J.A. Boogaard and Heleen M. Schoorl, Department of Information Technology, for technical support, Marieke J. Bosch, and Laura N. Deden, Vitalys Obesity Centre for the recruitment of patients. Finally, we would like to thank all the nurses from the Department of Bariatric Surgery, and patients for participating in this study.
Funding
Biosensors were provided free of charge by Philips. Other than that, support was provided solely from hospital and university sources.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Biosensors were provided free of charge by Philips. Other than that, support was provided solely from hospital and university sources. The authors declare no competing interests.
Ethical approval
Ethical approval for this study was asked for and waived by the Medical Research Ethics Committee Arnhem-Nijmegen, (registration 2019–5489). The study fell outside the remit of the law for Medical Research Involving Human Subjects Act and was approved by the local ethical committee.
Consent to participate
Written informed consent was obtained from all participants.
Consent for publication
Written informed consent for publication of their data to be used for scientific publication was obtained from all participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kant, N., Peters, G.M., Voorthuis, B.J. et al. Continuous vital sign monitoring using a wearable patch sensor in obese patients: a validation study in a clinical setting. J Clin Monit Comput 36, 1449–1459 (2022). https://doi.org/10.1007/s10877-021-00785-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-021-00785-y