Abstract
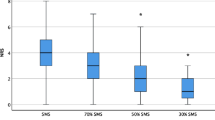
A more sensitive method than the train-of-four ratio seems required to detect low levels of residual neuromuscular blockade before tracheal extubation. The goal of the study was to determine the potential benefit of 5 s of 100 versus 200 Hz tetanic stimulation to quantify the residual block with mechanomyography in anesthetised patients. Twenty informed and consenting 18- to 80-year-old patients undergoing nose surgery were included. On the left hand, neuromuscular transmission was continuously monitored by acceleromyography. On the right side, a new mecanomyographic device (Isometric Thumb Force©) recorded the force of thumb adduction (N) developed during 5 s of 100- and 200 Hz tetanic stimulations of the ulnar nerve at three consecutive times: baseline before inducing the neuromuscular blockade, at the time of contralateral train-of-four ratio 0.9 recovery, and 3 min after additional sugammadex reversal. Tetanic Fade Ratios (TFR = F residual/F max) were compared between 100 and 200 Hz stimulations using Student’s t test. At the time of TOF ratio 0.9 recovery, both 100 and 200 Hz TFR were significantly decreased compared to baseline (0.61 and 0.16 on average, respectively, p < 0.0001). The 200 Hz TFR was significantly lower than the 100 Hz TFR (p < 0.0001). There were no differences between baseline and post-reversal TFR. The 200 Hz TFR has the potential to better describe low levels of residual neuromuscular blockade than the TOF ratio and 100 Hz TFR and would benefit from further investigations. Retrospectively registered in the Australian and New Zealand Clinical Trials Registry ACTRN12619000273189.


Similar content being viewed by others
Notes
This prototype device stems from the Laboratory of Microengineering and Bioinstrumentation—HEPIA/inSTI—University of Applied Sciences Western Switzerland (HES-SO Geneva), Campus Biotech, Chemin des Mines 9, CH-1202 Geneva, Switzerland. philippe.passeraub@hesge.ch / fabien.moreillon@hesge.ch.
References
Naguib M, Brull SJ, Kopman AF, et al. Consensus statement on perioperative use of neuromuscular monitoring. Anesth Analg. 2018;127:71–80.
Mencke T, Echternach M, Kleinschmidt S, et al. Laryngeal morbidity and quality of tracheal intubation: a randomized controlled trial. Anesthesiology. 2003;98:1049–56.
Madsen M, Staehr-Rye AK, Gätke MR, Claudius C. Neuromuscular blockade for optimising surgical conditions during abdominal and gynaecological surgery: a systematic review. Acta Anaesthesiol Scand. 2015;59:1–16.
Murphy GS, Brull SJ. Residual neuromuscular block: lessons unlearned. Part II: methods to reduce the risk of residual weakness. Anesth Analg. 2010;111:129–40.
Plaud B, Debaene B, Donati F, Marty J. Residual paralysis after emergence from anaesthesia. Anesthesiology. 2010;112:1013–22.
Viby-Mogensen J, Jensen E, Werner M, Nielsen HK. Measurement of acceleration: a new method of monitoring neuromuscular function. Acta Anaesthesiol Scand. 1988;32:45–8.
Claudius C, Viby-Mogensen J. Acceleromyography for use in scientific and clinical practice. A systematic review of the evidence. Anesthesiology. 2008;108:1117–40.
Capron F, Alla F, Hottier C, Meistelman C, Fuchs-Buder T. Can acceleromyography detect low levels of residual paralysis? A probability approach to detect a mechanomyographic train-of-four ratio of 0.9. Anesthesiology. 2004;100:1119–24.
Kirmeier E, Eriksson LI, Lewald H, et al. Post-anaesthesia pulmonary complications after use of muscle relaxants (POPULAR): a multicentre, prospective observational study. Lancet Respir Med. 2019;7:129–40.
Gissen AJ, Katz RL. Twitch, tetanus and posttetanic potentiation as indices of nerve-muscle block in man. Anesthesiology. 1969;30:481–7.
Waud BE, Waud DR. The relation between tetanic fade and receptor occlusion in the presence of competitive neuromuscular block. Anesthesiology. 1971;35:456–64.
Stanec A, Heyduk J, Stanec G, Orkin LR. Tetanic fade and post-tetanic tension in the absence of neuromuscular blocking agents in anesthetized man. Anesth Analg. 1978;57:102–7.
Kopman AF, Epstein RH, Flashburg MH. Use of 100-Hertz tetanus as an index of recovery from pancuronium-induced non-depolarizing neuromuscular blockade. Anesth Analg. 1982;61:439–41.
Ali HH, Savarese JJ, Lebowitz PW, Ramsey FM. Twitch, tetanus and train-of-four as indices of recovery from nondepolarizing neuromuscular blockade. Anesthesiology. 1981;54:294–7.
Passeraub P, Moreillon F, D’Hollander A, inventors; University of Applied Sciences HEPIA (HES-SO Geneva), assignee. 2016, Nov 25, Medical Device, Kit and Method for Sensing a Thumb Compression Force, Patent Application No. WO2018096077A1. https://patentscope.wipo.int/search/fr/detail.jsf?docId=WO2018096077&_cid=P21-K3RA8B-95513-1
Dubois PE, De Bel M, Jamart J, et al. Performance of acceleromyography with a short and light TOF-tube compared with mechanomyography. A clinical comparison. Eur J Anaesthesiol. 2014;31:404–10.
Suzuki T, Fukano N, Kitajima O, Saeki S, Ogawa S. Normalization of acceleromyographic train-of-four ratio by baseline value for detecting residual neuromuscular block. Br J Anaesth. 2006;96:44–7.
Silverman DG, Brull SJ. The effect of a tetanic stimulus on the response to subsequent tetanic stimulation. Anesth Analg. 1993;76:1284–7.
Baurain MJ, Hoton F, Dernovoi BS, d’Hollander AA. Influence and relative sensitivities of 50-Hz and 100-Hz tetanic stimuli on subsequent tetanic fade ratios in patients receiving vecuronium. Anesth Analg. 1996;82:139–42.
D’Hollander A, Duvaldestin P, Delcroix C, Nevelsteen M, Desmondts JM. Evolution of single twitch, train of four responses and of tetanic fade in relation to plasma concentrations of fazadinium in man. Anesth Analg. 1982;61:225–30.
Dupuis JY, Martin R, Tessonnier JM, Tétrault JP. Clinical assessment of the muscular response to tetanic nerve stimulation. Can J Anaesth. 1990;37:397–400.
Miller RD, Eger IE, Way WL, Stevens WC, Dolan WM. Comparative neuromuscular effects of Forane and halothane alone and in combinaison with d-tubocurarine in man. Anesthesiology. 1971;35:38–42.
Waud BE, Waud DR. The relation between the response to “train-of-four” stimulation and receptor occlusion during competitive neuromuscular block. Anesthesiology. 1972;37:413–6.
Funding
This work was supported by the Department of Anesthesiology and Scientific Support Unit of CHU UCL Namur site Godinne and benefited from a grant from the Fondation pour l’Anesthésie et la Réanimation (FAR), a philanthropic non-governmental organization founded in 1972, Vaduz, Principality of Lichtenstein.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation was performed by PAP, FM and AAd’. Data collection was performed by PED and JM. Data analysis was performed by MR. The first draft of the manuscript was written by PED and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Alain A D’Hollander is the President of the Fondation pour l’Anesthésie et la Réanimation (FAR) which granted this study. The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
Institutional Ethical Committee (CHU UCL Namur, Yvoir, Belgium, OM 050 Prof P. Evrard, under registration number 54/2017 B039201732500). Retrospectively included in the Australian and New Zealand Clinical Trials Registry (ACTRN12619000273189).
Informed consent
All patients provided written informed consent to participate to the study and for results publication.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Dubois, P.E., Mitchell, J., Regnier, M. et al. The interest of 100 versus 200 Hz tetanic stimulations to quantify low levels of residual neuromuscular blockade with mechanomyography: a pilot study. J Clin Monit Comput 36, 1131–1137 (2022). https://doi.org/10.1007/s10877-021-00745-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-021-00745-6