Abstract
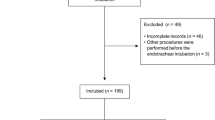
Tracheobronchial endoscopy with general anaesthesia for suspected foreign body aspiration exposes toddlers to acute hypoxemia. Better quantification of intraoperative hypoxemia could help identify and manage the most severe patients. We explored the hypoxic burden approach to account for both duration and depth of desaturation episodes during the procedure and determined risk factors for high hypoxic burden. We retrospectively analysed tracheobronchial endoscopies performed from September 2015 to September 2018 in children ≤ 36 months for suspected foreign body aspiration, in two French university hospitals. The hypoxic burden (area under 90% of the SpO2/time curve) was calculated. The median of non-zero burdens was used to delineate a subgroup with high hypoxic burden. Risk factors for high hypoxic burden were identified using multivariable analysis. Of 96 procedures, 56 (58%) were associated with at least one SpO2 value < 90%. Of them, the median [interquartile] hypoxic burden was 25 [5–87] %.min. Bradycardia < 100 bpm occurred in 11 procedures (11%). Initial admission to general hospitals (OR 0.23, 95% CI 0.06–0.86) and airway anaesthesia with topical lidocaine (OR 0.15, 95% CI 0.03–0.62) were associated with a reduced risk of high hypoxic burden. High hypoxic burden was associated with an increased risk of postoperative invasive ventilation (OR 32, 95% CI 1.7–617) and of hospital stay > 24 h (OR 4.0, 95% CI 1.6–10). No postoperative neurological sequelae were found. The hypoxic burden approach, when applied in tracheobronchial endoscopy for suspected foreign body aspiration in toddlers, enabled the quantification of hypoxemia and the search for specific risk factors.



Similar content being viewed by others
References
Fidkowski CW, Zheng H, Firth PG. The anesthetic considerations of tracheobronchial foreign bodies in children: a literature review of 12,979 cases. Anesth Analg. 2010;111:1016–25. https://doi.org/10.1213/ANE.0b013e3181ef3e9c.
Mohammad M, Saleem M, Mahseeri M, Alabdallat I, Alomari A, Za’atreh A, et al. Foreign body aspiration in children: a study of children who lived or died following aspiration. Int J Pediatr Otorhinolaryngol. 2017;98:29–31. https://doi.org/10.1016/j.ijporl.2017.04.029.
Hitter A, Hullo E, Durand C, Righini C-A. Diagnostic value of various investigations in children with suspected foreign body aspiration: review. Eur Ann Otorhinolaryngol Head Neck Dis. 2011;128:248–52. https://doi.org/10.1016/j.anorl.2010.12.011.
Laya BF, Restrepo R, Lee EY. Practical imaging evaluation of foreign bodies in children: an update. Radiol Clin N Am. 2017;55:845–67. https://doi.org/10.1016/j.rcl.2017.02.012.
Pitiot V, Grall M, Ploin D, Truy E, Ayari KS. The use of CT-scan in foreign body aspiration in children: a 6 years’ experience. Int J Pediatr Otorhinolaryngol. 2017;102:169–73. https://doi.org/10.1016/j.ijporl.2017.08.036.
Chen L, Zhang X, Li S, Liu Y, Zhang T, Wu J. The risk factors for hypoxemia in children younger than 5 years old undergoing rigid bronchoscopy for foreign body removal. Anesth Analg. 2009;109:1079–84. https://doi.org/10.1213/ane.0b013e3181b12cb5.
Bittencourt PFS, Camargos P, Picinin IF. Risk factors associated with hypoxemia during foreign body removal from airways in childhood. Int J Pediatr Otorhinolaryngol. 2013;77:986–9. https://doi.org/10.1016/j.ijporl.2013.03.026.
Chai J, Wu X-Y, Han N, Wang L-Y, Chen W-M. A retrospective study of anesthesia during rigid bronchoscopy for airway foreign body removal in children: propofol and sevoflurane with spontaneous ventilation. Paediatr Anaesth. 2014;24:1031–6. https://doi.org/10.1111/pan.12509.
Zhang X, Li W, Chen Y. Postoperative adverse respiratory events in preschool patients with inhaled foreign bodies: an analysis of 505 cases. Paediatr Anaesth. 2011;21:1003–8. https://doi.org/10.1111/j.1460-9592.2011.03603.x.
Hu S, Dong H, Sun Y, Xiong D, Zhang H, Chen S, et al. Anesthesia with sevoflurane and remifentanil under spontaneous respiration assisted with high-frequency jet ventilation for tracheobronchial foreign body removal in 586 children. Paediatr Anaesth. 2012;22:1100–4. https://doi.org/10.1111/j.1460-9592.2012.03874.x.
Maddali MM, Mathew M, Chandwani J, Alsajwani MJ, Ganguly SS. Outcomes after rigid bronchoscopy in children with suspected or confirmed foreign body aspiration: a retrospective study. J Cardiothorac Vasc Anesth. 2011;25:1005–8. https://doi.org/10.1053/j.jvca.2011.02.005.
Liao R, Li JY, Liu GY. Comparison of sevoflurane volatile induction/maintenance anaesthesia and propofol–remifentanil total intravenous anaesthesia for rigid bronchoscopy under spontaneous breathing for tracheal/bronchial foreign body removal in children. Eur J Anaesthesiol. 2010;27:930–4. https://doi.org/10.1097/EJA.0b013e32833d69ad.
Soodan A, Pawar D, Subramanium R. Anesthesia for removal of inhaled foreign bodies in children. Paediatr Anaesth. 2004;14:947–52. https://doi.org/10.1111/j.1460-9592.2004.01309.x.
de Graaff JC, Bijker JB, Kappen TH, van Wolfswinkel L, Zuithoff NPA, Kalkman CJ. Incidence of intraoperative hypoxemia in children in relation to age. Anesth Analg. 2013;117:169–75. https://doi.org/10.1213/ANE.0b013e31829332b5.
Azarbarzin A, Sands SA, Stone KL, Taranto-Montemurro L, Messineo L, Terrill PI, et al. The hypoxic burden of sleep apnoea predicts cardiovascular disease-related mortality: the Osteoporotic Fractures in Men Study and the Sleep Heart Health Study. Eur Heart J. 2019;40:1149–57. https://doi.org/10.1093/eurheartj/ehy624.
Leppänen T, Kulkas A, Töyräs J. The hypoxic burden: also known as the desaturation severity parameter. Eur Heart J. 2019;40:2991–3. https://doi.org/10.1093/eurheartj/ehz271.
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. Int J Surg. 2014;12:1495–9. https://doi.org/10.1016/j.ijsu.2014.07.013.
Trefethen L, Weideman J. The exponentially convergent trapezoidal rule. SIAM Rev. 2014;56:385–458. https://doi.org/10.1137/130932132.
Habre W, Disma N, Virag K, Becke K, Hansen TG, Jöhr M, et al. Incidence of severe critical events in paediatric anaesthesia (APRICOT): a prospective multicentre observational study in 261 hospitals in Europe. Lancet Respir Med. 2017;5:412–25. https://doi.org/10.1016/S2213-2600(17)30116-9.
Vik A, Nag T, Fredriksli OA, Skandsen T, Moen KG, Schirmer-Mikalsen K, et al. Relationship of “dose” of intracranial hypertension to outcome in severe traumatic brain injury. J Neurosurg. 2008;109:678–84. https://doi.org/10.3171/JNS/2008/109/10/0678.
Bickler P, Feiner J, Rollins M, Meng L. Tissue oximetry and clinical outcomes. Anesth Analg. 2017;124:72–82. https://doi.org/10.1213/ANE.0000000000001348.
Li L-W, He L, Ai Y, Chu Q, Zhang W. Site-directed topical lidocaine spray attenuates perioperative respiratory adverse events in children undergoing elective surgery. J Surg Res. 2016;203:206–10. https://doi.org/10.1016/j.jss.2016.03.011.
Roberts MH, Gildersleve CD. Lignocaine topicalization of the pediatric airway. Paediatr Anaesth. 2016;26:337–44. https://doi.org/10.1111/pan.12868.
Farrell PT. Rigid bronchoscopy for foreign body removal: anaesthesia and ventilation. Paediatr Anaesth. 2004;14:84–9. https://doi.org/10.1046/j.1460-9592.2003.01194.x
Acknowledgements
The authors warmly thank Mr. Hugo Terrisse for his statistical advice. They also thank Bow Medical for helping us to extract SpO2 data.
Author information
Authors and Affiliations
Contributions
SA, GI: Investigation, Writing—Original Draft. CG, BC, IA, SA: Writing—Review and Editing. LB, J-FP: Supervision, Writing—Review and Editing. J-NE: Conceptualization, Methodology, Formal analysis, Writing—Review and Editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethical statement
The study design was approved by the Ethics Committee of the French Society of Anaesthesia & Intensive Care Medicine (Institutional Review Board 00010254-2019-091) on June 23, 2019.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Aubanel, S., Izaute, G., Gariel, C. et al. Oxygen desaturation and time burden during tracheobronchial endoscopy for suspected foreign body in toddlers. J Clin Monit Comput 35, 1077–1084 (2021). https://doi.org/10.1007/s10877-020-00559-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-020-00559-y