Abstract
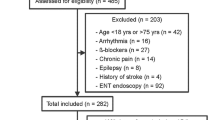
The ability to monitor the physiological effect of the analgesic agent is of interest in clinical practice. Nonstationary changes would appear in photoplethysmography (PPG) during the analgesics-driven transition to analgesia. The present work studied the properties of nonlinear methods including approximate entropy (ApEn) and sample entropy (SampEn) derived from PPG responding to a nociceptive stimulus under various opioid concentrations. Forty patients with ASA I or II were randomized to receive one of the four possible remifentanil effect-compartment target concentrations (Ceremi) of 0, 1, 3, and 5 ng·ml−1 and a propofol effect-compartment target-controlled infusion to maintain the state entropy (SE) at 50 ± 10. Laryngeal mask airway (LMA) insertion was applied as a standard noxious stimulation. To optimize the performance of ApEn and SampEn, different coefficients were carefully evaluated. The monotonicity of ApEn and SampEn changing from low Ceremi to high Ceremi was assessed with prediction probabilities (PK). The result showed that low Ceremi (0 and 1 ng·ml−1) could be differentiated from high Ceremi (3 and 5 ng·ml−1) by ApEn and SampEn. Depending on the coefficient employed in algorithm: ApEn with k = 0.15 yielded the largest PK value (0.875) whereas SampEn gained its largest PK of 0.867 with k = 0.2. Thus, PPG-based ApEn and SampEn with appropriate k values have the potential to offer good quantification of analgesia depth under general anesthesia.





Similar content being viewed by others
References
Eger EI, Sonner JM. Anaesthesia defined (gentlemen, this is no humbug). Best Pract Res Clin Anaesthesiol. 2006;20:23–9.
Guignard B. Monitoring analgesia. Best Pract Res Clin Anaesthesiol. 2006;20:161–80.
Fechner J, Ihmsen H, Schuttler J, et al. The impact of intra-operative sufentanil dosing on post-operative pain, hyperalgesia and morphine consumption after cardiac surgery. Eur J Pain. 2013;17:562–70.
Steyaert A, De Kock M. Chronic postsurgical pain. Curr Opin Anesthesiol. 2012;25:584–8.
Gruenewald M, Ilies C. Monitoring the nociception-anti-nociception balance. Best Pract Res Clin Anaesthesiol. 2013;27:235–47.
Korhonen I, Yli-Hankala A. Photoplethysmography and nociception. Acta Anaesthesiol Scand. 2009;53:975–85.
Huiku M, Uutela K, van Gils M, et al. Assessment of surgical stress during general anaesthesia. Br J Anaesth. 2007;98:447–55.
Bonhomme V, Uutela K, Hans G, et al. Comparison of the Surgical Pleth Index (TM) with haemodynamic variables to assess nociception-anti-nociception balance during general anaesthesia. Br J Anaesth. 2011;106:101–11.
Edry R, Recea V, Dikust Y, et al. Preliminary intraoperative validation of the nociception level index a noninvasive nociception monitor. Anesthesiology. 2016;125:193–203.
Choi BM, Park C, Lee YH, et al. Development of a new analgesic index using nasal photoplethysmography. Anaesthesia. 2018;73:1123–30.
Ni ZQ, Wang L, Meng J, et al. EEG signal processing in anesthesia feature extraction of time and frequency parameters. Procedia Environ Sci. 2011;8:215–20.
Jordan D, Stockmanns G, Kochs EF, et al. Electroencephalographic order pattern analysis for the separation of consciousness and unconsciousness an analysis of approximate entropy, permutation entropy, recurrence rate, and phase coupling of order recurrence plots. Anesthesiology. 2008;109:1014–22.
Wei Q, Liu Q, Fan SZ, et al. Analysis of EEG via multivariate empirical mode decomposition for depth of anesthesia based on sample entropy. Entropy. 2013;15:3458–70.
Kreuzer M. EEG based monitoring of general anesthesia: taking the next steps. Front Comput Neurosci. 2017;11:Art 56.
Koskinen M, Seppanen T, Tong SB, et al. Monotonicity of approximate entropy during transition from awareness to unresponsiveness due to propofol anesthetic induction. IEEE Trans Biomed Eng. 2006;53:669–75.
Vakkuri A, Yli-Hankala A, Talja P, et al. Time-frequency balanced spectral entropy as a measure of anesthetic drug effect in central nervous system during sevoflurane, propofol, and thiopental anesthesia. Acta Anaesthesiol Scand. 2004;48:145–53.
Schnider TW, Minto CF, Gambus PL, et al. The influence of method of administration and covariates on the pharmacokinetics of propofol in adult volunteers. Anesthesiology. 1998;88:1170–82.
Minto CF, Schnider TW, Egan TD, et al. Influence of age and gender on the pharmacokinetics and pharmacodynamics of remifentanil. I. Model development. Anesthesiology. 1997;86:10–23.
Pincus SM. Approximate entropy as a measure of system complexity. Proc Natl Acad Sci USA. 1991;88:2297–301.
Bruhn J, Ropcke H, Hoeft A. Approximate entropy as an electroencephalographic measure of anesthetic drug effect during desflurane anesthesia. Anesthesiology. 2000;92:715–26.
Liu Q, Chen YF, Fan SZ, et al. A comparison of five different algorithms for EEG signal analysis in artifacts rejection for monitoring depth of anesthesia. Biomed Signal Process Control. 2016;25:24–34.
Pincus SM, Goldberger AL. Physiological time-series analysis: what does regularity quantify. Am J Physiol. 1994;266:H1643–H16561656.
Kortelainen J, Koskinen M, Mustola S, et al. Effect of remifentanil on the nonlinear electroencephalographic entropy parameters in propofol anesthesia. In: Conf Proc IEEE Eng Med Biol Soc, 2009. p. 4994–7.
Shalbaf R, Behnam H, Sleigh J, et al. Measuring the effects of sevoflurane on electroencephalogram using sample entropy. Acta Anaesthesiol Scand. 2012;56:880–9.
Richman JS, Moorman JR. Physiological time-series analysis using approximate entropy and sample entropy. Am J Physiol Heart Circ Physiol. 2000;278:H2039–H20492049.
Liang ZH, Wang YH, Sun X, et al. EEG entropy measures in anesthesia. Front Comput Neurosci. 2015;9:Art 16.
Shalbaf R, Behnam H, Sleigh JW, et al. Monitoring the depth of anesthesia using entropy features and an artificial neural network. J Neurosci Methods. 2013;218:17–24.
Rantanen M, Yli-Hankala A, van Gils M, et al. Novel multiparameter approach for measurement of nociception at skin incision during general anaesthesia. Br J Anaesth. 2006;96:367–76.
Smith WD, Dutton RC, Smith NT. Measuring the performance of anesthetic depth indicators. Anesthesiology. 1996;84:38–51.
Shoushtarian M, Sahinovic MM, Absalom AR, et al. Comparisons of electroencephalographically derived measures of hypnosis and antinociception in response to standardized stimuli during target-controlled propofol–remifentanil anesthesia. Anesth Analg. 2016;122:382–92.
Martini CH, Boon M, Broens SJL, et al. Ability of the Nociception Level, a multiparameter composite of autonomic signals, to detect noxious stimuli during propofol–remifentanil anesthesia. Anesthesiology. 2015;123:524–34.
Weil G, Passot S, Servin F, et al. Does spectral entropy reflect the response to intubation or incision during propofol–remifentanil anesthesia. Anesth Analg. 2008;106:152–9.
von Dincklage F, Correll C, Schneider MHN, et al. Utility of nociceptive flexion reflex threshold, bispectral index, composite variability index and noxious stimulation response index as measures for nociception during general anaesthesia. Anaesthesia. 2012;67:899–905.
Gruenewald M, Ilies C, Herz J, et al. Influence of nociceptive stimulation on analgesia nociception index (ANI) during propofol–remifentanil anaesthesia. Br J Anaesth. 2013;110:1024–30.
Renaud-Roy E, Stöckle P-A, Maximos S, et al. Correlation between incremental remifentanil doses and the Nociception Level (NOL) index response after intraoperative noxious stimuli. Can J Anesth. 2019;66:1049–61.
Funcke S, Sauerlaender S, Pinnschmidt HO, et al. Validation of innovative techniques for monitoring nociception during general anesthesia a clinical study using tetanic and intracutaneous electrical stimulation. Anesthesiology. 2017;127:272–83.
Funding
This study was supported by the National Natural Science Foundation of China (Grant No: 81870868), Major Scientific Project of Zhejiang Lab (Grant No: 2018DG0ZX01) and China’s Natural Science Foundation #31627802.
Author information
Authors and Affiliations
Contributions
WC was responsible for study design, data analysis, manuscript preparation and revision. FJ contributed to the study design, data analysis and revised the manuscript for important intellectual content. XC and HC were involved in the study design, data collection, manuscript revision and project supervision. YF and CJ were responsible for data collection and interpretation of data. JM and SC contributed to data analysis and critical revision of the manuscript for important intellectual content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed on human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. This study was approved by the Research Ethics Committee (No. 20170131) and informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chen, W., Jiang, F., Chen, X. et al. Photoplethysmography-derived approximate entropy and sample entropy as measures of analgesia depth during propofol–remifentanil anesthesia. J Clin Monit Comput 35, 297–305 (2021). https://doi.org/10.1007/s10877-020-00470-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-020-00470-6