Abstract
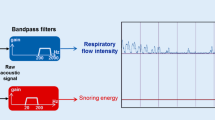
Apnea should be monitored continuously in the post anesthesia care unit (PACU) to avoid serious complications. It has been confirmed that tracheal sounds can be used to detect apnea during sedation in healthy subjects, but the performance of this acoustic method has not been evaluated in patients with frequent apnea events in the PACU. Tracheal sounds were acquired from the patients in the PACU using a microphone encased in a plastic bell. Concurrently, a processed nasal pressure signal was used as a reference standard to identify real respiratory events. The logarithm of the tracheal sound variance (log-var) was used to detect apnea, and the results were compared to the reference method. Sensitivity, specificity, positive likelihood ratios (PLR), and negative likelihood ratios (NLR) were calculated. One hundred and twenty-one patients aged 55.5 ± 13.2 years (mean ± SD) with a body mass index of 24.6 ± 3.7 kg/m2 were included in data analysis. The total monitoring time was 52.6 h. Thirty-four patients experienced 236 events of apnea lasting for a total of 122.2 min. The log-var apnea detection algorithm detected apnea with 92% sensitivity, 98% specificity, 46 PLR and 0.08 NLR. The performance of apnea detection in the PACU using the log-var tracheal sounds method proved to be reliable and accurate. Tracheal sounds could be used to minimize the potential risks from apnea in PACU patients.






Similar content being viewed by others
References
Voscopoulos C, Theos K, Tillmann HHA, George E. A risk stratification algorithm using non-invasive respiratory volume monitoring to improve safety when using post-operative opioids in the PACU. J Clin Monit Comput. 2017;31:417–26.
Dahan A, Aarts L, Smith TW. Incidence, reversal, and prevention of opioid-induced respiratory depression. Anesthesiology. 2010;112:226–38.
Kasuya Y, Akça O, Sessler DI, Ozaki M, Komatsu R. Accuracy of postoperative end-tidal Pco2 measurements with mainstream and sidestream capnography in non-obese patients and in obese patients with and without obstructive sleep apnea. Anesthesiology. 2009;111:609–15.
Maddox RR, Williams CK, Oglesby H, Butler B, Colclasure B. Clinical experience with patient-controlled analgesia using continuous respiratory monitoring and a smart infusion system. Am J Health Syst Pharm. 2006;63:157–64.
George JA, Lin EE, Hanna MN, Murphy JD, Kumar K, et al. The effect of intravenous opioid patient-controlled analgesia with and without background infusion on respiratory depression: a meta-analysis. J Opioid Manag. 2010;6:47–54.
Overdyk FJ, Carter R, Maddox RR, Callura J, Herrin AE, Henriquez C. Continuous oximetry/capnometry monitoring reveals frequent desaturation and bradypnea during patient-controlled analgesia. Anesth Analg. 2007;105:412.
Waugh JB, Epps CA, Khodneva YA. Capnography enhances surveillance of respiratory events during procedural sedation: a meta-analysis. J Clin Anesth. 2011;23:189–96.
Miller RD, Cohen NH, Eriksson LI, Fleisher LA, et al. (2015). Miller’s anesthesia. Philadelphia: Elsevier/Saunders.
Hogan J. Why don’t nurses monitor the respiratory rates of patients. Br J Nurs. 2006;15:489–92.
Lovett PB, Buchwald JM, Kai S, Bijur P. The vexatious vital: neither clinical measurements by nurses nor an electronic monitor provides accurate measurements of respiratory rate in triage. Ann Emerg Med. 2005;45:68–76.
Fu ES, Downs JB, Schweiger JW, Miguel RV, Smith RA. Supplemental oxygen impairs detection of hypoventilation by pulse oximetry. Chest. 2004;126:1552.
Keidan I, Gravenstein D, Berkenstadt H, Ziv A, Shavit I, Sidi A. Supplemental oxygen compromises the use of pulse oximetry for detection of apnea and hypoventilation during sedation in simulated pediatric patients. Pediatrics. 2008;122:293–8.
Cacho G, Pérez-Calle JL, Barbado A, Lledó JL, Ojea R, Fernández-Rodríguez CM. Capnography is superior to pulse oximetry for the detection of respiratory depression during colonoscopy. Rev Esp Enferm Dig. 2010;102:86–9.
Patino M, Redford DT, Quigley TW, Mahmoud M, Kurth CD, Szmuk P. Accuracy of acoustic respiration rate monitoring in pediatric patients. Paediatr Anaesth. 2013;23:1166–73.
Friesen RH, Alswang M. End-tidal PCO2 monitoring via nasal cannulae in pediatric patients: accuracy and sources of error. J Clin Monit Comput. 1996;12:155–9.
Gaucher A, Frasca D, Mimoz O, Debaene B. Accuracy of respiratory rate monitoring by capnometry using the Capnomask(R) in extubated patients receiving supplemental oxygen after surgery. Br J Anaesth. 2012;108:316–20.
Drummond GB, Bates A, Mann J, Arvind DK. Validation of a new non-invasive automatic monitor of respiratory rate for postoperative subjects. Br J Anaesth. 2011;107:462–9.
Nassi N, Piumelli R, Lombardi E, Landini L, Donzelli G, De MM. Comparison between pulse oximetry and transthoracic impedance alarm traces during home monitoring. Arch Dis Child. 2008;93:126–32.
Yu L, Ting CK, Hill BE, Orr JA, Brewer LM, et al. Using the entropy of tracheal sounds to detect apnea during sedation in healthy nonobese volunteers. Anesthesiology. 2013;118:1341–9.
Yadollahi A, Moussavi ZM. The effect of anthropometric variations on acoustical flow estimation: proposing a novel approach for flow estimation without the need for individual calibration. IEEE Trans Biomed Eng. 2011;58:1663–70.
Yadollahi A, Giannouli E, Moussavi Z. Sleep apnea monitoring and diagnosis based on pulse oximetry and tracheal sound signals. Med Biol Eng Comput. 2010;48:1087–97.
Yadollahi A, Moussavi ZM. A robust method for heart sounds localization using lung sounds entropy. IEEE Trans Biomed Eng. 2006;53:497–502.
Huq S, Yadollahi A, Moussavi Z. Breath analysis of respiratory flow using tracheal sounds. In IEEE International Symposium on Signal Processing and Information Technology. IEEE Xplore; 2008. pp. 414–18
Yadollahi A, Moussavi Z. (2008) Comparison of flow-sound relationship for different features of tracheal sound. In IEEE Engineering in Medicine and Biology Society; 2008. pp. 805–808.
Apfelbaum JL, Silverstein JH, Chung FF, Connis RT, Fillmore RB, et al. Practice guidelines for postanesthetic care: an updated report by the American Society of Anesthesiologists Task Force on Postanesthetic Care. Anesthesiology. 2013;118:291–307.
Yadollahi A, Moussavi ZM. A robust method for estimating respiratory flow using tracheal sounds entropy. IEEE Trans Biomed Eng. 2006;53:662–8.
Farré R, Rigau J, Montserrat JM, Ballester E, Navajas D. Relevance of linearizing nasal prongs for assessing hypopneas and flow limitation during sleep. Am J Respir Crit Care Med. 2001;163:494–7.
Ramsay MA, Usman M, Lagow E, Mendoza M, Untalan E, De Vol E. The accuracy, precision and reliability of measuring ventilatory rate and detecting ventilatory pause by rainbow acoustic monitoring and capnometry. Anesth Analg. 2013;117:69–75.
Mimoz O, Benard T, Gaucher A, Frasca D, Debaene B. Accuracy of respiratory rate monitoring using a non-invasive acoustic method after general anaesthesia. Br J Anaesth. 2012;108:872.
Lee LA, Caplan RA, Stephens LS, Posner KL, Terman GW, et al. Postoperative opioid-induced respiratory depression: a closed claims analysis. Anesthesiology. 2015;122:659.
Berry RB, Budhiraja R, Gottlieb DJ, Gozal D, Iber C, et al. Rules for scoring respiratory events in sleep: update of the 2007 AASM Manual for the Scoring of Sleep and Associated Events. Deliberations of the Sleep Apnea Definitions Task Force of the American Academy of Sleep Medicine. J Clin Sleep Med. 2012;8:597–619.
Funding
This study was funded by the National Natural Science Foundation of China, Beijing, P.R. China (Grant No. 81401485).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Liu, J., Ai, C., Zhang, B. et al. Tracheal sounds accurately detect apnea in patients recovering from anesthesia. J Clin Monit Comput 33, 437–444 (2019). https://doi.org/10.1007/s10877-018-0192-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-018-0192-6