Abstract
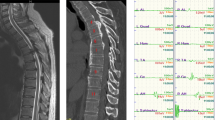
Transcranial electric motor evoked potentials (TCeMEPs) play an important role in reducing the risk of iatrogenic paraplegia. TCeMEPs could be obviously suppressed by neuromuscular blockade (NMB). The aims of this study were to examine the effects of NMB on TCeMEPs and to determine an appropriate level of partial neuromuscular blockade (pNMB) for TCeMEPs during surgical correction of idiopathic scoliosis under total intravenous anesthesia (TIVA). All patients were maintained with TIVA. The pNMB levels were classified into five phases: one or two train-of-four (TOF) counts (TOF1); three TOF counts, or T4/T1 (TOFR, T1,4, first or four twitch height of TOF) ≤ 15% (TOF2); TOFR at 16–25% (TOF3); TOFR at 26–50% (TOF4); and TOFR at 51–75% (TOF5). No neuromuscular blockade (nNMB) was achieved when TOFR was more than 75%. The absolute and relative latency, amplitude and area under curve (AUC), efficacy of TCeMEPs and rate of unexpected movement were compared among these phases. Neither the amplitude and AUC nor the efficacy of TCeMEPs were affected at TOF4−5 of abductor halluces muscles TCeMEPs (AH-TCeMEPs) or at TOF3−5 of tibialis anterior muscles TCeMEPs (TA-TCeMEPs) compared with nNMB. However, the rate of unexpected movement was increased significantly at TOF5 and nNMB compared with TOF1 and TOF4. The application of pNMB with TOFR aimed at 26–50% for AH-TCeMEPs or 16–50% for TA-TCeMEPs seems to be an appropriate regimen for TCeMEPs during surgical correction for idiopathic scoliosis under TIVA.




Similar content being viewed by others
References
Vitale MG, Moore DW, Matsumoto H, Emerson RG, Booker WA, Gomez JA, Gallo EJ, Hyman JE, Roye DP Jr. Risk factors for spinal cord injury during surgery for spinal deformity. J Bone Joint Surg. 2010;92(1):64–71. https://doi.org/10.2106/jbjs.h.01839.
Neira VM, Ghaffari K, Bulusu S, Moroz PJ, Jarvis JG, Barrowman N, Splinter W. Diagnostic accuracy of neuromonitoring for identification of new neurologic deficits in pediatric spinal fusion surgery. Anesth Analg. 2016;123(6):1556–66. https://doi.org/10.1213/ane.0000000000001503.
Pastorelli F, Di Silvestre M, Plasmati R, Michelucci R, Greggi T, Morigi A, Bacchin MR, Bonarelli S, Cioni A, Vommaro F, Fini N, Lolli F, Parisini P. The prevention of neural complications in the surgical treatment of scoliosis: the role of the neurophysiological intraoperative monitoring. Eur Spine J. 2011;20(Suppl 1):105–14. https://doi.org/10.1007/s00586-011-1756-z.
Thuet ED, Winscher JC, Padberg AM, Bridwell KH, Lenke LG, Dobbs MB, Schootman M, Luhmann SJ. Validity and reliability of intraoperative monitoring in pediatric spinal deformity surgery: a 23-year experience of 3436 surgical cases. Spine. 2010;35(20):1880–6. https://doi.org/10.1097/BRS.0b013e3181e53434.
Ohtaki S, Akiyama Y, Kanno A, Noshiro S, Hayase T, Yamakage M, Mikuni N. The influence of depth of anesthesia on motor evoked potential response during awake craniotomy. J Neurosurg. 2017;126(1):260–5. https://doi.org/10.3171/2015.11.jns151291.
Lieberman JA, Feiner J, Lyon R, Rollins MD. Effect of hemorrhage and hypotension on transcranial motor-evoked potentials in swine. Anesthesiology. 2013;119(5):1109–19. https://doi.org/10.1097/ALN.0b013e31829d4a92.
Sakamoto T, Kawaguchi M, Kakimoto M, Inoue S, Takahashi M, Furuya H. The effect of hypothermia on myogenic motor-evoked potentials to electrical stimulation with a single pulse and a train of pulses under propofol/ketamine/fentanyl anesthesia in rabbits. Anesth Analg. 2003;96(6):1692–7 (table of contents).
Sloan TB, Heyer EJ. Anesthesia for intraoperative neurophysiologic monitoring of the spinal cord. J Clin Neurophysiol. 2002;19(5):430–43.
Tsutsui S, Iwasaki H, Yamada H, Hashizume H, Minamide A, Nakagawa Y, Nishi H, Yoshida M. Augmentation of motor evoked potentials using multi-train transcranial electrical stimulation in intraoperative neurophysiologic monitoring during spinal surgery. J Clin Monit Comput. 2015;29(1):35–9. https://doi.org/10.1007/s10877-014-9565-7.
Yang J, Huang Z, Shu H, Chen Y, Sun X, Liu W, Dou Y, Xie C, Lin X, Hu Y. Improving successful rate of transcranial electrical motor-evoked potentials monitoring during spinal surgery in young children. Eur Spine J. 2012;21(5):980–4. https://doi.org/10.1007/s00586-011-1995-z.
Azabou E, Manel V, Andre-obadia N, Fischer C, Mauguiere F, Peiffer C, Lofaso F, Shils JL. Optimal parameters of transcranial electrical stimulation for intraoperative monitoring of motor evoked potentials of the tibialis anterior muscle during pediatric scoliosis surgery. Clin Neurophysiol. 2013;43(4):243–50. https://doi.org/10.1016/j.neucli.2013.08.001.
Mendiratta A, Emerson RG. Neurophysiologic intraoperative monitoring of scoliosis surgery. J Clin Neurophysiol. 2009;26(2):62–9. https://doi.org/10.1097/WNP.0b013e31819f9049.
Kalkman CJ, Drummond JC, Kennelly NA, Patel PM, Partridge BL. Intraoperative monitoring of tibialis anterior muscle motor evoked responses to transcranial electrical stimulation during partial neuromuscular blockade. Anesth Analg. 1992;75(4):584–9.
van Dongen EP, ter Beek HT, Schepens MA, Morshuis WJ, Langemeijer HJ, de Boer A, Boezeman EH. Within-patient variability of myogenic motor-evoked potentials to multipulse transcranial electrical stimulation during two levels of partial neuromuscular blockade in aortic surgery. Anesth Analg. 1999;88(1):22–7.
Cengiz M, Ganidagli S, Alatas N, San I, Baysal Z. Partial neuromuscular blockage levels with mivacurium during mastoidectomy allows intraoperative facial nerve monitoring. ORL. 2008;70(4):236–241. https://doi.org/10.1159/000130871.
Claudius C, Viby-Mogensen J. Acceleromyography for use in scientific and clinical practice: a systematic review of the evidence. Anesthesiology. 2008;108(6):1117–40. https://doi.org/10.1097/ALN.0b013e318173f62f.
Leon-Sarmiento FE, Rizzo-Sierra CV, Leon-Ariza JS, Leon-Ariza DS, Sobota R, Prada DG. A new neurometric dissection of the area-under-curve-associated jiggle of the motor evoked potential induced by transcranial magnetic stimulation. Physiol Behav. 2015;141:111–9. https://doi.org/10.1016/j.physbeh.2015.01.014.
Tamkus AA, Rice KS, Kim HL. Differential rates of false-positive findings in transcranial electric motor evoked potential monitoring when using inhalational anesthesia versus total intravenous anesthesia during spine surgeries. Spine J. 2014;14(8):1440–6. https://doi.org/10.1016/j.spinee.2013.08.037.
Zhuang Q, Wang S, Zhang J, Zhao H, Wang Y, Tian Y, Zhao Y, Li S, Weng X, Qiu G, Shen J. How to make the best use of intraoperative motor evoked potential monitoring? Experience in 1162 consecutive spinal deformity surgical procedures. Spine. 2014;39(24):E1425–32. https://doi.org/10.1097/brs.0000000000000589.
Sloan TB, Erian R. Effect of vecuronium-induced neuromuscular blockade on cortical motor evoked potentials. Anesthesiology. 1993;78(5):966–73.
Kim WH, Lee JJ, Lee SM, Park MN, Park SK, Seo DW, Chung IS. Comparison of motor-evoked potentials monitoring in response to transcranial electrical stimulation in subjects undergoing neurosurgery with partial vs no neuromuscular block. Br J Anaesth. 2013;110(4):567–76. https://doi.org/10.1093/bja/aes395.
Hemmer LB, Zeeni C, Bebawy JF, Bendok BR, Cotton MA, Shah NB, Gupta DK, Koht A. The incidence of unacceptable movement with motor evoked potentials during craniotomy for aneurysm clipping. World Neurosurg. 2014;81(1):99–104. https://doi.org/10.1016/j.wneu.2012.05.034.
Yamamoto Y, Kawaguchi M, Hayashi H, Horiuchi T, Inoue S, Nakase H, Sakaki T, Furuya H. The effects of the neuromuscular blockade levels on amplitudes of posttetanic motor-evoked potentials and movement in response to transcranial stimulation in patients receiving propofol and fentanyl anesthesia. Anesth Analg. 2008;106(3):930–4. https://doi.org/10.1213/ane.0b013e3181617508 (table of contents).
Mahmoud M, Sadhasivam S, Salisbury S, Nick TG, Schnell B, Sestokas AK, Wiggins C, Samuels P, Kabalin T, McAuliffe J. Susceptibility of transcranial electric motor-evoked potentials to varying targeted blood levels of dexmedetomidine during spine surgery. Anesthesiology. 2010;112(6):1364–73. https://doi.org/10.1097/ALN.0b013e3181d74f55.
Schwartz DM, Sestokas AK, Dormans JP, Vaccaro AR, Hilibrand AS, Flynn JM, Li PM, Shah SA, Welch W, Drummond DS, Albert TJ. Transcranial electric motor evoked potential monitoring during spine surgery: is it safe? Spine. 2011;36(13):1046–9. https://doi.org/10.1097/BRS.0b013e3181ecbe77.
Oro J, Haghighi SS. Effects of altering core body temperature on somatosensory and motor evoked potentials in rats. Spine. 1992;17(5):498–503.
Schwartz DM, Auerbach JD, Dormans JP, Flynn J, Drummond DS, Bowe JA, Laufer S, Shah SA, Bowen JR, Pizzutillo PD, Jones KJ, Drummond DS. Neurophysiological detection of impending spinal cord injury during scoliosis surgery. J Bone Joint Surg. 2007;89(11):2440–9. https://doi.org/10.2106/jbjs.f.01476.
Acknowledgements
The study was funded by the National Natural Science Foundation (81371207), the Key Talent’s of 13th Five-year Plan for Strengthening Health of Jiangsu Province (ZDRCA2016069), the Key Talent’s Project in Medical Science of Jiangsu Province (RC2011006), the Fundamental Research Funds for the Central Universities (0214-14380338), the Natural Science Foundation of Jiangsu Province of China (BK20170654) and the National Natural Science Foundation (81701371). We thank Hua-ye Xu, Jie Chen, Fen Song and Shi-he Cui, who are anesthetists in the department of Anesthesiology, Affiliated Drum Tower Hospital of Medical Department of Nanjing University. We also thank Jun-yin Qiu, neurologist in the department of Orthopaedic Surgery, Affiliated Drum Tower Hospital of Medical Department of Nanjing University for her invaluable assistance in collecting the data in this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Liu, Hy., Xia, Tj., Zhu, Zz. et al. Effect of neuromuscular blockade on transcranial electric motor evoked potentials during surgical correction for idiopathic scoliosis under total intravenous anesthesia. J Clin Monit Comput 33, 471–479 (2019). https://doi.org/10.1007/s10877-018-0182-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-018-0182-8